![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
85 Cards in this Set
- Front
- Back
|
Implant use for maxillary and mandibular fractures with FAS 0-3 |
- Closed reduction and external skeletal fixation
- Bone plate and screws (miniplates)
- Maxilomandibular fixation for vertical ramus |
|
|
Implant use for maxillary and mandibular fractures with FAS 4-7 |
- Interdental fixation techniques
- Bone plate and screws
- External skeletal fixation |
|
|
Implant use for maxillary and mandibular fractures with FAS 8-10 |
- Tape muzzle
- Interdental fixation techniques
- Interfragmentary wiring
- Cerclage wire (sympyseal fractures) |
|
|
Conservative management of scapular fracture |
Velpeau sling and limited exercise for most closed, minimally displaced fractures of the scapular body and spine in dogs that will heal rapidly.
Velpeau slings should not be left on for longer than 2-3 weeks, taking care to prevent contracture of the carpus |
|
|
Treatment of articular fractures of the shoulder joint |
Open reduction, anatomic alignment and rigid fixation.
Fixation systems used: Plates and screws, orthopaedic wire, and K-wires. Plates and screws offer the most stable form of fixation. |
|
|
Nerves and arteries to be consider with scapular fracture repair |
- Suprascapular nerve and artery course over the scapular notch and under the acromial process
- Axillary artery and nerve are located immediately caudal to the joint so not usually visualised during surgery |
|
|
Nerves and vessels of the lateral humerus to be aware of |
- Radial nerve courses from medial to lateral in the musculospiral groove of the distal humerus under the triceps and over the brachialis mm. (radial nerve injury can result from distal humerus fracture) - Cephalic vein is craniolateral over the brachicephalicus m. |
|
|
Nerves and vessels of the medial humerus to be aware of |
Neurovascular bundle running subcutaneously over the triceps and biceps brachii mm.:
- Median, musculocutaneous and ulnar nerves plus the brachial artery and vein |
|
|
PE findings of humerus diaphyseal fracture |
- Non weight bearing - Varying degrees of limb swelling - Pain and crepitus on limb manipulation - Dragging of limb while walking and may not lift paw when proprioception is checked (Radial n. injury or pain and swelling making patient reluctant to move) |
|
|
Implant use for fractures of the humeral diaphysis with FAS 0-3 |
- Bone plate and IM pin
- Bone plate and screws
- Interlocking nail
- Modified type 1b ESF with IM pin |
|
|
Implant use for fractures of the humeral diaphysis with FAS 4-7 |
- ESF with or without IM pin
- Bone plate and screws
- Interlocking nail |
|
|
Implant use for fractures of the humeral diaphysis with FAS 8-10 |
- IM pin with cerclage wires or ESF
- Flexible bone plate and screws
- External coaptation (casts and splints) |
|
|
Articular fracture |
Fracture involving the joint surface |
|
|
Physeal fracture |
Fracture involving the growth plates in immature animals |
|
|
Epiphyseal fracture and Metaphyseal fracture |
Occur in the trabecular bone at the proximal or distal end of the humerus |
|
|
Y/T- Fracture of the humeral condyle |
Fractures of the distal humerus (elbow) that include fractures of the lateral and medial portions of the condyle.
Especially common in Spaniels with incomplete ossification between the medial and lateral portions of the humeral condyle. |
|
|
Why are lateral condyle fractures more common? |
- The radial head articulates with the lateral portion of the condyle, transmitting weight-bearing forces primarily through the lateral portion of the condyle - The anatomic position of the lateral condyle is eccentric to the bony column, causing WB forces to be transmitted through the weak epicondylar ridge to the humeral diaphysis |
|
|
When do fractures of the lateral portion of the condyle normally occur? |
- When young/toy breed dogs fall or jump from furniture or their owner's arms with elbow extended. When they land, high loads are transmitted through the radial head-lateral condylar axis, resulting in separation of the lateral portion of the condyle - Incomplete ossification of the humeral condyles in Spaniels |
|
|
Implant use for Humeral Condylar Fractures with FAS 4-10 |
- Lag screws plus K-wires
- Self-compressing pin |
|
|
Implant use for Humeral Condylar Fractures with FAS 0-3 |
Lag screws plus plate |
|
|
Anatomical landmarks of the elbow |
- Medial and lateral epicondyles - Olecranon - Cephalic vein within the subq tissues along the craniolateral surface of the limb - Radial nerve lies beneath the lateral head of the triceps near the distal 1/3 of the humerus and superficial to the brachialis and ulnar nerve along the cranial edge of the medial head of the triceps |
|
|
What factors contribute to the high frequency of delayed unions and nonunions in toy breed dogs with distlas radial diaphyseal fractures? |
- Short oblique nature of the fractures and lack of bone space to place adequate # of pins/screws
- Lack of distal diaphyseal vasculature compared with large breeds
- Limited surrounding soft tissue for the extraosseous vasculature |
|
|
Surgical anatomy of the radius and ulna |
- Craniomedial surface of the radius and the caudal lateral surface of the ulna have no muscle - Extensor muscles are located cranial to and flexor muscles caudal to the radius (can be retracted to expose the bone) - Cephalic vein in medial part of distal radius - Lateral radial head is beneath the extensor mm. of forearm |
|
|
Deciding to do an open or closed reduction for radial diaphyseal fractures |
- Open reduction: Displaced reducible fractures with plate application - Limited open reduction: Displaced reducible fractures with ESF and comminuted fractures for cancellous bone graft placement - Closed reduction: Nondisplaced fractures with external coaptation or ESF and comminuted nonreducible fractures with ESF |
|
|
Implant use for radial diaphyseal fractures with an FAS 0-3 |
- Bone plate and screws
- Type II ESF |
|
|
Implant use for radial diaphyseal fractures with an FAS 4-7 |
- Type Ib or type II ESF
- Bone plates and screws |
|
|
Implant use for radial diaphyseal fractures with an FAS 8-10 |
- Type Ia or type Ib ESF
- Cast (NOT TOY BREEDS) |
|
|
Why are IM pins contraindicated with radial fractures? |
- Due to the narrow configuration of the radial medullary canal.
- The necessity of invading the carpal joint to position the pin.
(IM pins can however, be used in the ulna) |
|
|
Common errors in radial and ulnar diaphyseal fracture fixation |
- IM pin placement through the carpus causes degenerative joint disease and LOF - Inadequate rotational stabilisation for transverse or short oblique fractures causes delayed union or nonion, esp. in toy breed dogs - Premature removal of fixation from slowly healing distal radial #s (nonunions more likely) - Valgus deformities after comminuted # fixation due to malalignment of ESF |
|
|
Proximal ulnar fractures |
Require implant systems that resist the pull of the triceps (tension band wires and plates/screws) |
|
|
Surgical anatomy of the ulna |
- Olecranon and caudal border of ulna
- Ulnar nerve courses over the medial aspect of the elbow, caudal to the medial humeral epicondyle |
|
|
Surgical anatomy of the antebrachial carpal joint |
- Supported by the short radial collateral ligaments (O: medial styloid process of the radius), the dorsal radiocarpal ligament (O: dorsal surface of distal radius), and the short ulnar collateral and radioulnar ligaments (O: ulnar styloid process) |
|
|
Complications with physeal fractures |
- Premature closure of the physis often occurs which may affect bone length in young dogs - Implants can migrate - If intra-articular DJD may result - Bone resorption and implant loosening - Fatigue breakage of implants (olecranon osteotomy repair) due to being a heavy WB area - Decreased ROM |
|
|
Implant use for distal radial and ulnar fractures with an FAS of 0-3 |
- Lag screw
- K-wire |
|
|
Implant use for distal radial and ulnar fractures with an FAS of 4-7 |
- Lag screw
- Tension band wire (figure 8)
- K- wire |
|
|
Implant use for distal radial and ulnar fractures with an FAS of 8-10 |
- Tension band wire with K-wire |
|
|
Post-op care of distal radial/ulnar fractures |
- W/ internal fixation a soft-padded bandage is used few days to control swelling/support ST - Often supported by a splint for 6 weeks - Physio starts after splint is removed - Open wounds treated with wet-to-dry dressings until granulation bed has formed and then covered with a non-adhesive pad |
|
|
Complications of distal radial/ulnar fractures |
- DJD with articular fractures possible
- Delayed union and nonunion with inadequate stabilisation due to constant tensile stress exerted on the fracture line from the pull of the triceps muscle or collateral ligaments |
|
|
Why is the physis weaker than surrounding bone and ligaments? |
Because it is cartilaginous, so it is more susceptible to injury.
The weakest portion of the physis is the junction of the zone of hypertrophying cells (weak) with the zone of ossification (strong). |
|
|
Why is the junction of the zone of hypertrophying cells with the zone of ossification the weakest point of the physis? |
- The ZOHCs has a large cell-to-cell matrix ratio, giving it a weak structure - Stress [ ] is created when two areas w/ different mechanical properties are adjacent to each other - If a physis is fractured, separation normally occurs through the ZOHCs. A fracture here does NOT affect proliferating cells and will NOT compromise potential growth |
|
|
What type of Salter Harris fractures normally occur in the proximal and distal radial physes? |
- SH Type I
- SH Type II
- Infrequently ocult SH Type V (diagnosed after forelimb growth altered) |
|
|
What type of Salter Harris fractures normally occur with the distal ulnar physis? |
SH Type V (traumatic and may be associated with radial fracture)
Not visible radiographically until 2-3 weeks post-trauma when premature closure of the physis is observed, |
|
|
DDx of physeal fractures |
- Joint luxation
- Soft tissue trauma
Can be differentiated via radiographs |
|
|
What is key for choosing implants for a physeal fracture repair |
Only use SMOOTH implants |
|
|
How do you determine physeal function after physeal injury? |
- 2-3 weeks after injury radiographs of the injured leg can be compared to radiographs of the contralateral limb and their bone length compared - Cartilage physes that are healing properly will appear as a lucent line on radiographs - Increased bone length should be apparent |
|
|
When should implants be removed with physeal fractures? |
After 4 weeks (how long it takes for physeal healing) to allow for continued bone growth of the physis if it is still functional |
|
|
Complications with radial and ulnar physeal fractures |
- Premature physeal closure with resulting growth deformities (severity depends on the animal's age when physeal closure occurs and location/extent of physeal closure) - Young animals with > growth potential have more severe sequelae - Premature closure of the ulnar physis can interefere with radial growth too and result in shortening, rotation and angulation of radius - Asynchrony of the paired bones causes incongruity of the elbow/carpal joints - DJD due to partial closure of GP causing angular deformity |
|
|
Growth of radius and ulna |
Radius: 40% proximal physis + 60% distal physis
Ulnar: 15% proximal physis + 85% distal physis
Growth accelerates rapidly during 4th-6th months and tapers in the 9th-10th months |
|
|
What will a forelimb look like with premature closure of the distal ulna physis? |
- Cranial bowing and shortening of the forelimb
- Valgus (lateral) deviation of the carpus |
|
|
What will a forelimb look like with symmetrical closure of the radial physes? |
- Minimal angular deformity
- Pain on palpation of the elbow |
|
|
What will a forelimb look like with aymmetric premature closure of the distal radial physes? |
- Angular deformity depending on the location of the closure |
|
|
What must physeal closure causing growth deformities be distinguished from? |
Poor confirmation and laxity or contracture of supporting soft tissue structures such as ligament and tendons |
|
|
How are immature dogs treated for damaged physes? |
- Ostectomy of the affected bone coupled with placement of a free autogenous fat graft to prevent premature union of the segment - Resecting the bone-bridged part of a asymmetric physeal closure and placement of a fat graft in removed spot of physis - Complete closure requires R/U osteotomy and continuous distraction to mimic growth |
|
|
How are mature dogs treated for angular limb deformities caused by premature closure of the distal ulnar physis? |
- Aimed at correcting angular and rotational deformities while preserving limb length and improving joint congruity - Oblique radial and ulnar corrective osteotomy stabilised w/ Type II ESF - Hybrid ESF - Continuous distraction with circular ESF |
|
|
How are mature dogs treated for premature closure of the proximal or distal radial physis? |
- Improve limb function by re-establishing normal radial length and elbow congruency |
|
|
Complications with ulnar and radial physeal injuries |
- Delayed union - Nonunion - Osteomyelitis - Pin tract infection - Fixation failure |
|
|
Types of carpal fractures |
- Distal row of bones: Compression fractures with carpal extension injuries - Avulsion of bone fragments by ligamentous attachments - Slab or stress fractures - Accessory C bone fractures in racing greyhound - Fractures due to incomplete ossification - Avulsion accessory bone fractures |
|
|
Types of tarsal fractures |
- Calcaneal fractures (distracted by the pull of the gastrocnemius m. bone fragment contact is prevented and intereferes with healing so treatment must resists tensile force) - Talar neck fractures (cats) - Condylar fractures - Central tarsal bone fractures (Ghounds) often resulting in 4th tarsal bone and calcaneous # |
|
|
PE signs of carpus/tarsal fracture |
- Acute: Non-WB lameness, attempts to place weight on limb cause C/T to collapse in a plantigrade stance - Chronic: Intermittent WB lameness, reduced carpal ROM, ST swelling - Angular deformity |
|
|
DDx for C/T fractures |
- Ligamentous injuries (may occur concurrently with fractures) - Calcaneal #s must be differentiated from lacerations/rupture of the calcaneal tendon. Acute lacerations have an open wound and ST swelling proximal to calcaneal tuberosity. - Calcaneous # exhibits swelling caudal to tarsus |
|
|
Is conservative management of C/T fractures possible? |
NO, rigid fixation must be applied since there is so these joints play such a major WB role.
Casts and splints are not effective (do not counteract tensile force of ligaments/tendons) |
|
|
Chip fragments in C/T |
If small should be removed
If large should be anatomically reduced w/ lag screws and K-wires |
|
|
Carpal arthrodesis should be used to fix: |
- Chronic radial carpal bone fractures - Severely comminuted fractures - Osteoarthritis - Luxation - Bone loss - Osteomyelitis |
|
|
Calcaneal fracture fixation |
Pull of gastrocnemius m. must be resisted with a tension band wire, lag screws or a plate. |
|
|
Articular fractures of the talus |
Anatomically reduced and rigidly stabilised |
|
|
If fracture repair of the tarsus is not feasible: |
Consider arthrodesis of the tarsocrural joint |
|
|
Carpus anatomy |
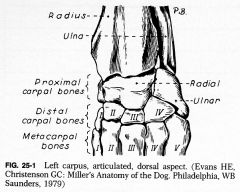
Proximal and distal row of carpal bones (radial is major WB area) |
|
|
Tarsus Anatomy |
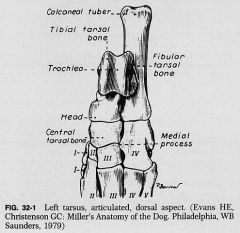
Achilles tendon inserts on calcaneal tuber.
Talus articulates with tibia/fibula and central tarsal bone |
|
|
Post-op rehab |
- Short leash walking - Passive flexion and extension of the carpus/tarsus to maintain joint motion, enhance patient comfort and improve synovial nutrient presentation to the articular cartilage |
|
|
Sesamoid bone |
Small, round/oblong bones found adjacent to joints |
|
|
How are metacarpal/metatarsal fractures classified? |
According to location:
- Base or proximal end of the bone - Shaft - Diaphysis - Head or distal end of bone |
|
|
Where do avulsion fractures of the MC/MT bones usually occur? |
The 2nd and 5th bones because of their ligamentous insertions |
|
|
Sesamoid fractures |
Occur after excessive tension on the digital flexor tendons
Sesamoid bones 2 and 7 of the FL are most often affected
Less obvious lameness than MT/MC fractures |
|
|
Bivalve cast or a metasplint treatment of MC/Mt injuries |
- Closed, nondisplaced MC/MT diaphyseal fractures affecting one or two bones (2nd and 5th esp.) - Cats with comminuted nonreducible fractures - Phalangeal and acute sesamoid bone fractures - Cast shouldn't be removed until radiographic evidence of fracture bridging is present (4-8 weeks) |
|
|
Plate fixation of MC/MT fractures |
- FAS is low - When athletic function is desired
- Bridging plates for comminuted #s, compression plates for transverse #s, lag screw compression and neutralisation plate for oblique #s |
|
|
Lag screw fixation for avulsion fractures |
Lag screws are used to counteract the pull of adjacent ligaments or to compress oblique fractures |
|
|
Treatment considerations for MC/MT fractures |
- #s of 1/2 MT/MC bones: splint/cast
- #s of 3/4 MC/MT bones: internal fixation
- Large displaced avulsion #s: Lag screws
- Splint/bivalve cast used with internal fixation until bone healing occurs |
|
|
IM pins in MC/Mt fractures |
Used to treat multiple transverse or short oblique fractures in patients with high FAS |
|
|
Treatment considerations for MC/MT luxations |
- Acute luxations in working/racing dog best treated w/ open reduction and suturing of the joint capsule and collateral ligaments - Chronic luxations of the 2nd/5th toe can be treated with amputation - Arthrodesis of metacarpophalangeal and interphalangeal joints can result in good function and pain relief |
|
|
Implant use for MC/MT/phalangeal fractures with a FAS of 0-3 |
- Bridging plates - ESF - Lag screws for avulsion fractures
- Choice depends on number of bones fractured, comminution, displacement, number of limbs injured and desired function in animal |
|
|
Implant use for MC/MT/phalangeal fractures with a FAS of 4-7 |
- Bone plates and screws - IM pins - Lag screws for avulsion fractures
- Choice depends on number of bones fractured, comminution, displacement, number of limbs injured and desired function in animal |
|
|
Implant use for MC/MT/phalangeal fractures with a FAS of 8-10 |
- Splint or cast - IM pins - Tension band wire for avulsion fractures
- Choice depends on number of bones fractured, comminution, displacement, number of limbs injured and desired function in animal |
|
|
What are the primary WB bones of the MC/MT? |
- 3rd and 4th digits |
|
|
Surgical anatomy of MC/MT |
- Superficial dorsal MC/MT artery runs over the dorsal aspect of the paw - Extensor tendons down dorsal aspect of digits - Flexor tendons & superficial + deep MC/MT artery/vein on palmar/plantar aspect of the digits - Joints have medial + lateral collateral ligaments - Paired proximal sesamoid bones are caudal to MTP/MCP joints w/ ligamentous attachments |
|
|
Tourniquet use |
- Useful to control haemorrhage during surgery
- Applied to distal limb
- Maintained for < 1 hour |

