![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
78 Cards in this Set
- Front
- Back
|
Analgesic - given to relieve pain Sedatives - given to calm, sooth or produce sedation Hypnotics - given to produce sleep |
Pain is - subjective - both psychological and physiological components - some have higher pain threshold because of conditiong, ethnic background, sensitivity or physiological factors (endorphin release) |
|
|
Endorphins - endogenous analgesics produced within body as a reaction to severe pain or intense exercise (e.g. runner's high) - block transmission of pain - may be responsible for placebo effect (relief from pain without administration of an analgesic) |
Analgesics - opioid (full or pure agonists, partial agonists or mixed agonsists-antagonists) - nonopioid - adjuvant Agonists bind to and activate opiate receptors and cause analgesia, miosis (pupillary dilation), respiratory depression, and decreased GI motility. |
|
|
Types of Opioids (Analgesics) Full agonist (morphine, hydromorphone, oxycodone, and fentanyl) similar to opium, altering perception of pain (they do not have medication level at which there is no enhanced analgesia) Pure Agonist (buprenorphrine, butorphanol and nalbuphine): willnot reverse analgesia |
Opioids - potential abuse and psychological dependence (controlled substances in U.S. include natural - opium alkaloids (morphine and codeine), - semisynthetics (hydromophone and oxycodone) and - the synthetics (e.g. meperidine [Demerol] and fentanyl [Duragesic] |
|
|
Nov 2010, FDA request market withdrawal of all products containing propoxyphene (Darvon and Darvocet) which linked to cardiac abnormalities and death from overdose |
Opioids - tend to cause Tolerance (larger dose of opiod is needed to achieve same level of analgesia) and physiological dependence (physical adaptation of body to opioid and withdrawal symptoms after abrupt drug discontinuation) *not used for extended periods except to relieve chronic pain, (cancer pain, terminal illness and nonmalignant pain in selected patients who do not benefit from other pain methods) |
|
|
More effective pain control: combine opiods with nonopiod and adjuvant drugs - Analgesic should be given to terminally ill patients with constant around-the-clock pain. with additional "as needed" doses for breakthru pain and dosages adjusted to acceptable level of side effects |
Chronic Pain therapy - back pain: additional tricyclic antidepressant or anticonvulsants to analgesic regimen - drugs that enhance analgesic effects (adjuvant analgesic) (can reduce needed dosage of opioids) |
|
|
Side effects of Opioids - sedation, confusion, euphoria, restlessness, agitation - headache, dizziness, hypotension, bradycardia - urinary retention; sexual dysfunction - nausea and vomiting and constipation - respiratory depression (appropriate dose titration reduces risk) - physical and or emotional dependence; tolerance - blurred vision, seizures with large doses - flushing, rash, and pruritus (opiate agonist cause histamine release, esp codeine, morphine and meperidine) |
Precautions or Contraindications with Opioids - Head injury (conditions with increased intracranial pressure) - cardiac disease (methadone associated with AQ prolongation - cause cardiac arrhythmia can be fatal) and hypotension - CNS depression, GI, Hepatic, Renal, and Thyroid Diseases - Sleep apnea, pregnancy, lactation, children, older adults and debilitated patients - driving or operating machinery (may impair mental or physical abilities) - addiction prone, suicidal and alcoholic persons - opiate agonist hypersensitivity (can try opioid from different chemical class with close monitoring - abrupt drug discontinuation in patients taking opioids chronically |
|
|
Interactions of Opioids with all CNS depressants (include potentiation of effect of opioid) - psychotropics - alcohol - sedatives and hypnotics - muscle relaxants - antihistamine - antiemetics - antiarrhythmics or antihypertensives |
Pre operation: Opioid (Fentanyl) usually administered parenterally before start of anesthesia - Meperidine not recommended for routine use due to metabolite that may accumulate and cause seizures in patients with kidney disease (useful for treatment of post-op shivering) - Morphine and hydromorphone use to manage moderate to severe pain due to longer duration of effect and potency. - Hydromorphone is 4-8 times more potent than morphine ** - FDA announced drug manufacturers to limit strength of acetaminophen i n Rx drug (combo of acetaminophen and opioids) to 325 mg per dosage form. = help reduce risk of severe liver injury (acetaminophen( |
|
|
Hydrocodone-containing products (Schedule III controlled substance) = most commonly prescribed in 2011. - most abused drugs along with oxycodone - movement by DEA to move hydrocodone-containing products to Schedule II Controlled Substsance (limit which kind of health care practitioners can write and how many times) |
Tramadol (Ultram) - centrally acting synthetic analog of codeine with dual mechanism action - produces analgesia by weak inhibition of norepinephrine and serotonin reuptake and is an opioid receptor agonist - has LESS POTENTIAL for ABUSE or Respiratory Depression (although both may occur) - Not Classified as Controlled Substance) *Doses above normal therapeutic range produce several negative side effects |
|
|
Tapentadol (Nucynta) - take advantage of positives associated with tramadol and fewer of its negatives - does not involve serotonin reuptake - lower incidence of GI adverse effects - Classified as Schedule II Controlled Substance Side Effects and Precautions of Tramadol and Tapentadol (Similar to ones listed for Opioids) Interactions: - MAOIs or neuroletpics (may increase seizure risk) - Carbamazepine (tegretol) antagonizes tramadol action - Selective serotonin reuptake inhibitors (SSRIs) esp Paxil, Zoloft, tricyclic antidepressants and triptans (may cause serotonin syndrome and increase seizure risk) |
Opioid Antagonist - reversal agent naloxone (Narcan) used in treatment of of opioid overdoses and in operating room, delivery room, newborn nursery for opiate-induced respiratory depression - ◦ Antagonists bind to opioid receptors but block the action of morphine-like agonists and do not have analgesic properties of their own. - Naltrexone (ReVia) pure opioid antagonist and sublingual buprenorphine (partial opioid antagonist) used separately and together (Suboxone) in treatment of opioid dependence. |
|
|
Table 19-1 Opioid Analgesics page 355-356 lists generic name, trade name, dosage, uses/comments |
Nonopioid Analgesics - many available without Rx as OTC - relieve mild to moderate pain, fever, and anti-inflammatory conditions. Ex: arthritis - also used as coanalgesic in severe acute or chronic pain requiring opioids - Salicylates (aspirin) most commonly used for their analgesic and antipyretic properties and anti-inflammatory action. - Ibuprofen also used for analgesic properties - NSAIDS (chapter 21) - Acetaminophen (analgesic and antipyretic but very little effect on inflammation) - Aspirin and Acetaminophen frequently combined with Opioids or other drugs effective analgesic action -include the NSAIDs, Aspirin and Tylenol. |
|
|
Table 19-2 Nonopioid Analgesic and Antipyretics pg 357 |
Salicylates and other NSAIDs - Salicylate analgesic and anti-inflammatory actions associated primarily with preventing formation of prostaglandins and subsequent inflammatory repsonse prostaglandins help to induce - Side Effects esp with prolonged use and high doses = prolonged bleeding time, bleeding and frequent bruising, gastric distress, ulceration and bleeding (may be silent), Tinnitus (ringing in ears) hearing loss with overdose*, hepatic dysfunction, renal insufficiency, decreased urine output with sodium and water retention, renal failure, drowsiness, dizziness, headache, sweating, euphoria, and depression, Rash, Coma, respiratory failure, or anaphylaxis (result from hypersensitivity or overdosage esp in children (aspirin allergy), GI symptoms (can be minimized by admin with food or milk or aspirin buffer with antacids or in enteric-coated form) - poisoning (keep out of reach of children) |
|
|
Precautions and Contraindications for Salicylates and Other NSAIDS - GI ulcer and bleeding, bleeding disorders (taking with anticoagulant) - asthma - under 15 with influenza-like illness (danger of Reye's Syndrome) - treatment of pain with NSAIDs after heart surgery - Pregnancy - Lactation - Vitamin K deficiency - Allergy to ASA |
Caution in Salicylates and other NSAIDs - anemia - hepatic disease - renal disease - hodgkin's disease - pre or postoperative conditions (discontinue 5-7 days before elective surgery) Interactions - alcohol (may increase potential for ulceration and bleeding - anticoagulants (potentiation) - corticosteroids (gastric ulcer) - Antacids in high doses (decreased effect) - NSAIDS (decreased effect, increased GI side effect) - Do not give salicylate and NSAIDs together (unless approved by a physician) - insulin or oral antidiabetic agents (increased effects; may interfere with certain urinary glucose test) - methotrexate (increased effects - Probenecid (decreased effects) - Antihypertensives: angiotensin-converting enzyme (ACE) inhibitors, beta-blockers and diuretics (decreased effect) - carbonic anhydrase inhibitors (toxic effects e.g. Diamox) |
|
|
Acetaminophen (Tylenol) use for treatment of mild to moderate pain and fever - has very little effect on inflammation) - has fewer adverse side effects than Salicylates (does not cause gastric irritation or precipitate bleeding - sometimes used only for its analgesic properties in treating chronic pain of arthritis, (so salicylate dosage may be reduced to safer levels with fewer side effects in patients. |
Side effects of Acetaminophen (rare but large dose) - severe liver toxicity - renal insufficiency (decreased urine output) - rash or urticaria - blood dyscrasia caution: must be used with frequent acetaminophen use and alcohol ingestion because of potentiation liver damage (caution must be used with pregnancy and breast-feeding) Contraindication with hypersensitivity to acetaminophen or any component of combination product |
|
|
Acetaminophen lowered dosage from 4,000 to 3,000 daily |
Adjuvant Analgesics - intended for treatment of conditions other than pain - may enhance analgesic effect with opioids and nonopioids , produce analgesia alone or reduce side effects of analgesics
|
|
|
Adjuvant Analgesics treats: Fibromyalgia - chronic, widespread musculoskeletal pain - muscle tenderness sleep disturbances and - profound fatigue Neuropathic Pain: Nerve pain can be caused by certain disease states (diabetic neuropathy) infections (postherapeutic neuralgia) and medications (certain chemotherapeutic agents and antiretrovirals) |
Lidocaine (topical patch - Lidoderm) effective treat nerve pain and other types of localized pain while avoiding adverse effects of oral or parenterally administered meds. |
|
|
Tricyclic Antidepressants - treat fibromyalgia and nerve pain (herpes, arthritis, diabetes, and cancer;migraine or tension headaches; insomnia; and depression) - describe pain as "burning" - increasing available norepinephrine and serotonin (blocks pain transmission) Drugs: amitriptyline, desipramine, and nortriptyline *Allow 2-3 weeks to see therapeutic effects |
Side effects of Tricyclic Antidepressants (more so with amitriptyline) - drymouth, urinary retention, delirium and constipation - sedation (take at bed time) - orthostatic hypotension - tachyarrhythmias - heart block in cardiac patients = degree of side effects varies with each antidepressant (side effects may be additive with opioids (increased constipation, hypotension and sedation) Caution: must be used with tricyclics if used with prostatic hypertrophy, urinary retention, increased intraocular pressure and glaucoma Precautions/Contraindications apply to hypersensitivity and recovery phase of myocardial infarction |
|
|
Serotonin Norepinephrine Reuptake Inhibitors (SNRI) Duloxetine (Cymbalta) and venlafaxine (Effexor XR) = antidepressants that inhibit reuptake of both serotonin and norepinephrine - do not affect histamine or muscarinic receptors like tricyclics = anticholinergic side effects are not present - SNRI antidepressants used to treat diabetic neuropathy and fibromyalgia -*Milnacipran (Savella) SNRI with antidepressant activity indicated only for fibromyalgia* |
Side effects of SNRIs - sleep disturbance, headache, nausea, stomach pain, diarrhea, constipation, dizziness and sweating, Venlafaxine has potential to increase blood pressure and heart rate Precautions/Contraindications: - apply to narrow-angle glaucoma, hepatic (duloxetine, venlafaxine) or renal (milnacipran) impairment, abrupt discontinuation, patients with history of suicidal ideation or behaviors and substantial alcohol use Interactions: - all SNRIs and serotonergics (MAOIs and SSRIs) = serotonin syndrome (rapid dev of hyperthermia, hypertension, rigidity, autonomic instability, mental status changes (coma and delirium), Milnacipran has fewer interactions than other SNRIs) |
|
|
Anticonvulsants (Neurontin and Tegretol), like tricyclic antidepressants commonly used for managing nerve pain associated with neuralgia, herpes zoster (shingles) and cancer. - anticonvulsant therapy implemented when patient describes pain as "sharp, shooting, shock-like, lightning pain" - Gabapentin (Neurontin) considered first-line anticonvulsants for neuropathic pain therapy - Second line: carbamazepine (Tegretol) and Lamotrigine (Lamictal) - Carbamazepine indicated for trigeminal neuralgia (tic douloureux) symptoms include: episodes of facial pain, (painful spasms of facial muscles) Pregabalin (Lyrica): chemically and structurally similar to gabapentin (second gen anticonvulsant approved by FDA for Fibromyalgia, diabetic neuropathy and postherapeutic neuralgia) - has been designated as a Schedule V controlled substance because potential for abuse and dependence |
Side effects of anticonvulsants - sedation, dizziness, confusion, nausea, vomiting, contipation and anorexia - ataxia and unsteadiness, hepatitis (not Lyrica) - Rash, Stevens-Johnson syndrome (Lamictal- start low, low titration upward) - Bone marrow suppression - Nystagmus, diplopia (double vision) and blurred vision - Gingivitis (gabapentin) - weight gain and peripheral edema (pregbalin) Caution: - if used with allergies, hepatitis, cardiac disease and renal disease. CAUTION: do not CONFUSE Lamictal (anticonvulsant) with Lamisil (antifungal) Precautions or Contraindications - hypersensitivity, psychiatric conditions (increased risk of suicidal ideation and behavior) pregnancy, SA (sinoatrial) and AV (atrioventricular) block with (Tegretol) - Hemolytic disorders (Tegretol) - Abrupt discontinuation Interactions: - alcohol (decreased effect), antacids (decreased effect with Neurontin) - Antineoplastics (decreased effect with Tegretol) - CNS depressants (decreased effects with Tegretol) - Folic Acid (decreased effects with Lamictal) - ACE inhibitors and antidiabetic agents Actos and Avandia with Lyrica (increased risk of angioedema) - Antiretrovirals (increased or decreased effects) with Lamictal and Tegretol |
|
|
Local Anesthetics - Lidocaine patch (Lidoderm): approved for management of postherpeticneuraliga (can provide significant analgesia in other forms of neuropathic pain include diabetic neuropathy, musculoskeletal pain- osteoarthritis and lower back pain) - topical Lidocaine provide pain relief thru peripheral effect and has little if any central action. - penetration of lidocaine into intact skin is sufficient to produce analgesic effect but less amount necessary to produce anesthesia. |
Lidocaine patch must be applied to intact skin* - patches may be cut into smaller sizes with scissors before removal of release liner - to reduce potential for serious adverse effects, patch only worn up to 12 hours within a 24 hour period then removed - May take up to 2 weeks to achieve desired outcomes Side effects of Lidocaine patch: generally mild and transient - Erythema, edema and hives, allergic reactions Precautions or Contraindications for lidocaine patch - sensitivity to local anesthetics, hepatic disease, nonintact skin, pregnancy, breast feeding, pediatric use, handling and disposal to prevent access by children or pets Drug Interactions - antiarrhythmic drugs (mexiletene) and local anesthetics |
|
|
Sometimes local vasoconstricting agent (epinephrine) given in conjunction with local anesthetic injection (lidocaine) to further help localize effect and prolong duration of effect |
Migraine = most common neurovascular headache (include nausea, vomiting, sensitivity to light or noise) - simple analgesics, NSAIDs, and opioid analgesics can be effective if taken at initial sign of migraine |
|
|
Antimigraine Agents - Serotonin Receptor Agonists (SRAs) if unresponsive to simple analgesics, NSAIDs, and opioid analgesics, Action: serotonin levels decrease, while vasodilation and inflammation of blood vessels in brain increase as migraine symptoms worsen - Effective in treating associated nausea and vomiting (serotonin receptors also found in GI tract) - First "triptan" approved was sumatriptan (Imitrex) followed by 6 others - SRA indicated for acute treatment of migraines in adults and are not FDA approved for prophylactic management of migraine headaches |
Side effects of SRAs - Malaise, fatigue, dizziness, and drowsiness - nausea, vomiting, diarrhea - asthenia, tingling, parethesias, and flushing - pain or pressur ein chest, neck or jaw - arrhythmias, angina, palpitations, myocardial infarction and cardiac arrest Precautions or Contraindications - Patients with cerebrovascular or cardiovascular disease - uncontrolled hypertension - peripheral vascular disease - hepatic or renal disease (dose adjustment may be needed) - older adults (who are more likely to have decreased hepatic function and more pronounced blood pressure increases are at risk for coronary artery disease) - pregnancy and lactation - children Drug Interactions - Ergot alkaloids (methylergonovine; additive vasospastic effects) - MAOIs elevate plasma levels of most triptans (do not use within 2 weeks of discontinuing use of MAOI) - most antidepressants potentiate effects of serotonin (SSRIs and tricyclics) and may result in serotonin syndrome (mental status changes, diaphoresis, tremor, hyperreflexia and fever) when used in combination - macrolide antibiotics, antiretroviral protease inhibitors and "azole" antifungals with eletrptan (increased plasma levels) (do not use within at least 71 hours of each other) |
|
|
TABLE 19-4 antimigraine agents pg 365 |
Sedatives and Hypnotics - Medications used to promote sedation in smaller doses - Promote sleep in larger doses =prevalence of insomnia higher in women and older people - used prior to procedures - Hypnotics are used to manage insomnia. Drugs here : bensodiazepines (BZD) and nonbenzodiazepines (non-BZDs) (some psychotropic drugs like trazodone and mirttazapine and some antihistamines are used as sedative-hypnotics) * These agents have no analgesic properties. |
|
|
Sedatives and Hypnotics 1.Antihistamine:diphenhydramine (benadryl, Nytol, Sominex) and doxylamine (Unisome) have extended half-life remain in system longer- slower metabolism and impaired circulation (older or debilitated pateient susceptible to side effects (bluured vision, dizziness, hypotension, confusion and decreased coordination. Can develop "morning-after" problems if used long time, tolerance can develop to sleep-inducing effect but not side effects - antihistamine not as effective as other sedative hypnotics (should not be used more than 10 days except under medical supervision (potential for psychological and physical dependence), depress REM phase sleep, withdrawal after prolonged use can result in severe rebound night mares and hallucinations short term for one week may result in rebound insomnia - gradual reduction * 2. before treatment, patient should be encouraged to use nondrug interventions to combat insomnia 3. Barbiturates rarely used as sedative hypnotics bceause of serious potentially dangerous side effects esp CNS depression*, Phenobarbital still used treat seizure disorder Barbituate used for sedation is restricted to specific limited circumstances |
Benzodiazepines and Nonbenzodiazepines -BZDs like temazepam (Restoril) and NON BZDs (like zolpidem (Ambien) - less potential for abuse - Controlled substances due to phys and psyc dependence - withdrawal effects observed after long-term use and respiratory depression (when taken with alcohol) can potentially be fatal - short term 7-10 days recommended Side Effects: daytime sedation, confusion, headache-hangover, increased risk of falls (esp in older adults or long=acting hypnotics) dependence or withdrawal symptoms, amnesia, hallucinations, bizarre behavior (may occur more with triazolam( [Halcion] than other benzodiazepines Metallic aftertaste with Lunesta (eszopiclone) Sleepwalking and engaging in complex task (sleep eating, sleep driving and sleep-sex) |
|
|
Precautions/Contraindications with Sedativehypnotics - hypersensitivity - severe liver impairment - coadminstration of azole antifungals or protease inhibitors with triazolam - severe renal impairment - porphyria (with BZDs) - abrupt discontinuation - older adults - debilitated patients - addiction-prone patients - renal impairemen, liver impairment - depressed and mentally unstable people - individuals who have suicidal ideation or behavior - pregnancy and lactation - children, COPD and sleep apnea Interactions - psychotropic drugs, alcohol, muscle relaxants, antiemetics, antihistamines, analgesics |
Melatonin Receptor Agonst - Ramelteon (Rozerem): first FDA-approved prescription medication that acts on melatonin receptor - Mimics action of melatonin to trigger sleep onset - Dependence and abuse potential are eliminated - Not classified as a controlled substance - Works quickly, generally inducing sleep in less than one hour - dose reduction not required in older adults, should be used with caution in patients with hepatic impairment - contraindicated with fluvoxamine (Luvox) inhibits metabolism of ramelteon (do not use ramelteon with melatonin due to potential for additive sedative effects) |
|
|
Page 368 table 19-5 Sedatives and Hypnotics (Use Hypnotics Short Term ONLY) Benzodiazepines, Nonbenzodiazepines - Melatonin Receptor Agonist |
Patient Ed taking analgesic, sedatives or hypnotics - withdrawal after prolonged use of sedatives and hypnotics - mental alertness and physical coordination impairment cause accidents or falls - not discontinuing abruptly, take limited doses for short period of time except to relieve pain in terminal illness - caution with interactions , not taking meds that potentiate CNS depression potential for physical and psychological dependence and tolerance with opioids, sedatives, and hypnotics - potential for overdose of sedatives or hypnotics and paradoxical reactions with older adults (confusion, agitation, hallucinations and hyperexcitability)
|
|
|
Seventy-two year old Maureen O'Malley is in recovery room after just have undergone a right total hip replacement for severe arthritis. - The recovery room nurse will administer which category of medication first to relieve Maureen's pain? = Analgesic page 357 (for arthritis) |
After administering an opioid analgesic, nurse should observe Maureen for which side effect? - Respiratory Depression |
|
|
The best method to assess Maureen's response to analgesic is to observe - her respiratory rate |
While reviewing Maureen's Medication orders, nurse keeps in mind that which additional drug can cause potentiation of opioid? - muscle relaxant |
|
|
The nurse administering an opioid to Maureen will use extreme caution if she has history of = COPD |
Case Study B Hypnotics Sanjay Rudip has been experiencing insomnia for past 6 weeks. At his annual physical, Sanjay reports to his physician that he saw a commercial for Lunesta (eszopiclone) and wants to know if this med is right for him |
|
|
1. The physician explains to Sanjay that hypnotic meds should not be used for extended amounts of time except under close medical supervision. What is the primary reason? = an increase in REM sleep as a withdrawal symptom |
Eszopiclone falls into which category of sedatives or hypnotics = Nonbenzodiazepine |
|
|
The physician discusses possible interactions of other drugs and hypnotic meds with Sanjay. Which category of drug may potentiate CNS depression when taken in conjunction with hypnotic and should therefore be AVOIDED? = Anticoagulant |
A side effect of prolonged use of a hypnotic is = Asthma |
|
|
Tricyclic antidepressant / adjuvant = amitriptyline |
Opioid analgesic with acetaminophen = Vicodin |
|
|
Antimigraine = Imitrex |
Opioid analgesic and narcotic withdrawal = methadone |
|
|
Opioid analgesic with aspirin = Percodan |
Opioid antagonist = Duragesic |
|
|
Opioid antagonist = fentanyl |
Opioid antagonist = codeine |
|
|
Opioid antagonist = Narcan |
Anticonvulsant / adjuvant analgesic = Tegretol |
|
|
Which medication is used to treat opiate-induced respiratory depression = Naloxone |
Nonopioid analgesics are commonly obtained by which method = over the counter |
|
|
Salicylates are most commonly used for which properties = Anti-inflammatory |
Which group of medications is used as a coanalgesic in severe or chronic pain = Opioids |
|
|
GI symptoms experienced from taking salicylates can be minimized by taking the medication by which of the following methods = Divided doses |
Chapter 20 Psychotropic Meds, alcohol and drug abuse |
|
|
Psychtropic - refers to any substance that acts on the mind - Psychotropic medications are drugs that can exert a therapeutic effect on a person’s mental processes, emotions, or behavior = Classified according to the purpose for administration: (5) CNS stimulants, antidepressants, anxiolytics, antimanic, and antipsychotic medications - Frequently prescribed concurrently with psychotherapy or professional counseling |
CNS stimulants CNS (central nervous system) stimulant medications - Given to promote CNS functioning Ex: caffeine, amphetamine/methylphenidate prep and wakefulness-promoting agents |
|
|
Caffeine - Helps fight fatigue and drowsiness - Examples: NoDoz, Vivarin, and caffeine citrate (Cafcit) = prescription only - reat neonatal apena to stimulate CNS's respiratory drive = Prolonged, high intake of caffeine in any form may produce tolerance, habituation, and psychological dependence - Doses 100-200 mg not more often than every 3-4 hours - Physical signs of withdrawal: headaches, irritation, nervousness, anxiety, dizziness may occur upon abrupt discontinuation of stimulant |
Excessive consumption of caffeine (esp when taken with alcohol or other drugs) can lead to life-threatening irregular heartbeats, heart attacks and seizures. - Caffeine crosses placenta, distributed into milk of nursing women, pregnant (due to high risk of miscarriage) or nursing should avoid or limit their consumption of foods, beverages and drugs containing caffeine (ex: OTC analgesic or decongestants) |
|
|
Amphetamine.Methylphenidate Preparations - Treats attention-deficit hyperactivity disorder (ADHD) in children over age six and for narcolepsy (first line therapy for ADHD) = Examples: Amphetamines (Adderall) and (methylphenidate) Ritalin = Schedule II controlled substance - Ritalin also occasionally used to treat senile apathy and major depression refractory to other therapies |
Amphetamine.Methylphenidate Preparations - Daytrana - transdermal system contains methylphenidate in a multipolymeric adhesive matrix (make drug difficult to extract) difficult to reapply once taken off. - Vyvanse - prodrug converted to dextroamphetamine in GI tract used to treat ADHD = *both products have potential for lower risk of abuse than other formulations* |
|
|
Amphetamine.Methylphenidate Preparations - use of amphetamines to reduce appetite in treatment of obesity is NOT RECOMMENDED because tolerance develops rapidly and physical and /or psychological dependence may develop within a few weeks - These drugs have high potential for abuse and should be used only under medical supervision for diagnosed medical disorders. |
Side effects of controlled CNS stimulants (Amphetamine.Methylphenidate Preparations ) - nervousness, insomnia, irritability, seizures, psychosis from overdose - Tachycardia, palpitations, hypertension, cardiac arrhythmias - dizziness, headache, blurred vision(dilated pupils with photophobia) - GI disturbances,( anorexia, nausea, vomiting, abdominal pain and dry mouth) - Habituation and dependence possible with prolonged use *FDA report serious cardiovascular adverse events in patients taking usual doses of ADHD products= sudden death in patients with underlying serious heart problems or defects and reports of stroke and heart attack in adults (with certain risk factors) - patients need to work with doctor for a treatment plan, careful history, eval current status, |
|
|
Precautions or contraindications for CNS stimulants (Amphetamine.Methylphenidate Preparations ) - treatment for obesity (never more than 3-6 weeks) without diet and exercise modifications (weight gain resumes after discontinuation of med) - anxiety or agitation - history of drug dependence, alcoholism, or eating disorders - hyperthryoidism - cardiovascular disorders - closed-angle glaucoma (not modafinil) - Pregnant or nursing women - abrupt withdrawal (depression results) - use with MAOIs (may cause hypertensive crisis) Caution: must be used with sustained-release prep differing in designations (CD, ER, LA, SR) and their respective dosing requirements Pediatric Precautions: - prolonged admin of CNS stimulants with ADHD - cause at least a temp suppression of normal weight and or height patterns in some, - close monitoring required. - growth rebound observed after discontinuation, attainment of normal adult weight and height does not appear to be compromised. - exacerbate vocal tics and Tourette's disorders and clinical eval for these should precede use - observe carefully for dev of tics while receiving drug Abuse of amphetamines: signs and symptoms of chronic amphetamine abuse and acute toxicity |
Wakefulness-Promoting Agents - Modafinil (Provigil) is a psychostimulant approved for narcolepsy, sleep apnea, and shift-work sleep disorder (adults and adolescent >16) - potential for abuse and dependence lower than amphetamines and methylphenidate - Modafinil effective in treating ADHD in children and adolescent (not adults) was not approved by FDA for this purpose (side effects that developed with doses used in clinical trials) - not demonstrated to promote weight loss* |
|
|
Side effects of modafinil (Provigil) Wakefulness-Promoting Agents - mild headache, dizziness, nausea, and anorexia - anxiety, insomnia, depression, and mood changes - hypertension, palpitations, tachyarrythmia Caution: - possible causes of fatigue and sleepiness should be determined before stimulant. without adequate investigation: common disorders (diabetes and sleep apnea) might go underdiagnosed - reducing necessary amount of restorative sleep for prolonged periods of time = mental physical problems (esp neurological and cardiovascular effects) = |
Patient Ed for controlled CNS stimulants - potential side effects - potential abuse and take meds only according to drs orders - taking meds early in day to reduce insomnia - abrupt withdrawal may result in depression, irritability, fatigue, agitation and disturbed sleep - watch signs of tics, gastric disturbances, insomnia, weight loss, nervousenss (children) receiving amphetamines and methylphenidate and report them to drs. - potential for dangerous cardiovascular side effects - not chewing or crushing sustained- releaseproducts - necessity for regular sleep in sufficient amounts to restore mental/pysch functioning to optimal level while taking modafinil |
|
|
Selective Norepinephrine Reuptake Inhibitor (SNRI) for ADHD - Atomoxetine (Strattera) - Selective norepinephrine reuptake inhibitor - First nonstimulant, noncontrolled drug approved for attention-deficit hyperactivity disorder (ADHD) - Structurally related to fluoxetine - Does not have a potential for abuse, has less insomnia, less effect on growth, and has been shown to be safe and effective (children 6 and adults with ADHD) |
Selective Norepinephrine Reuptake Inhibitor (SNRI) for ADHD - side effects : dry mouth, reduced appetite, and fatigue, nausea, vomiting, constipation and dyspepsia, urinary hesitation or retention - increased risk of suicidal tendencies in children/adolescents ("black box" warning) Precautions or Contraindications - narrow-angle glaucoma - cerebrovascular, heart or hepatic disease - possible growth disturbance during treatment Interactions - Methylphenidate (combo not studied) - Beta-antagonists, vasopressor agents, and quinidine - Fluoxetine, paroxetine, venlafaxine, and MAOIs |
|
|
Table 20-1 CNS stimulant and Nonstimulant Meds page 378 caffeine citrate amphetamine lisdexamfetamine methylphenidate modafinil atomoxetine |
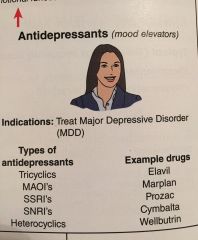
Antidepressants - Major depressive disorder (MDD) - Mental disorder characterized by an all-encompassing low mood accompanied by low self-esteem and loss of interest or pleasure in normally enjoyable activities - Antidepressant medications, sometimes called mood elevators, are used primarily to treat patients with various types of depression - exact cause of depression unknown but may result from chemical imbalance in brain - Neurotransmitters: dopamine, serotonin, and norepinephrine (shortage = depression) - if NT reabsorbed by one nerve ending before they have chance to make contact with next nerve cell, they cannot perform function |
|
|
Antidepressants sometimes called mood elevators (primarily treat various types of depression) 5 categories - tricyclic antidepressants - MAOIs - SSRIs - SNRIs - heterocyclic antidepressants *although symptoms may be relieved in first month, generally advisable to counsel patients to continue antidepressant therapy for 6-12 months to prevent relapse - FDA directed all manufacturers of ALL antidepressants to include "black box" warning - increase risk of suicidal thinking and behavior (particularly during first few months) in short term studies with children (manic depressive disorder and other psychiatric disorders) |
Tricyclics Antidepressants - Mechanism of action involves potentiation of norepinephrine and serotonin activity by blocking their reuptake - includes strong anticholinergic activity responsible for many side effects sen - may be lethal in overdose (cardiac conduction abnormalities or dysrhythmias) - have delayed action, elevating mood and increasing alertness after 2-4 weeks - frequently given at bedtime (mild sedative effect) - used with caution in older adults strong sedative and anticholinergic properties and increased risk of falls - may be more effective than SSRIs in some severe depression, used an adjunct in neuropathic pain control. |
|
|
Side effects of Tricyclics (imipramine (Tofranil) are anticholinergic in action - dryness of mouth, increased appetite and weight gain, drowsiness and dizziness, blurred vision - constipation, urinary retention, esp with benign prostatic hyperplasia (BPH) - sexual dysfunction, postural hypotension, cardiac arrhythmias, and palpitation - confusion (in older adults) Precautions/Contraindications - cardiac, renal, GI, liver disorders - older adults, glaucoma, obesity, seizure disorder - pregnancy, lactatin, concomitant use with MAOIs, SSRIs (increase tricyclic blood levels) INteractions: - certain antiarrhthmics and some quinolones (QT prolongation) - Clonidine (causing hypertensive crisis) - CNS drugs and alcohol |
Monoamine Oxidase Inhibitors (MAOIs) - Mechanism of action involves increasing concentrations of serotonin, norepinephrine, and dopamine in the neuronal synapse by inhibiting the MAO enzyme that degrades or breaks down these nuerotransmitters - phenelzine (Nardil) rarely used today because of potential serious side effects and numerous food, herbal and drug interactions discontinued = reserved for refractory or atypical depression or associated with panic disorders/phobias |
|
|
Side effects of MAOI are adrenergic in action - nervousness, agitation, insomnia, headache - stiff neck, hypertension or hypertensive crisis (can be fatal) - Tachycardia, palpitation, chest pain - nausea, vomiting and diarrhea, blurred vision Precautions/Contraindications - Patients with cerebrovascular, heart, liver and renal disease - children under 16 years - pregnancy and lactation - abrupt discontinuation Interactions with some drugs, foods, and herbal supplements can cause hypertensive crisis (severe headache, palpitation, sweating, chest pain, possible intracranial hemorrhage, even death) - may occur with adrenergic drugs and levodopa, SSRI and SNRIs (result in seizures, fever, hypertension, confusion" serotonin syndrome") - CNS depressants (result in circulatory collapse) - foods containing tyramine, tryptamine or tryptophan (yogurt, sour cream all cheeses, liver (esp chicken) pickleld herring, figs, raisins, bananas, pineapple, avocados, broad beans (chinese pea pods) meat tenderizers, alcoholic bevs (wine and beer) and all fermented aged foods (corn beef, salami, pepperoni) - Ensam (selegiline) selective MAOI type B administered as transdermal patch indicated for treatment of MDD in adults - blockade of MAO enzyme reduce metabolism of dopamine but not norepinephrine or serotonin. - transdermal allow lower doses and direct absorption into blood stream- reduce likelihood of dietary tyramine-induced hypersensitivity crisis |
Selective Serotonin Reuptake Inhibitors (SSRI) - First-line medications for treatment of depression - Selectively block reabsorption of serotonin, helping to restore the brain’s chemical balance - drugs: fluoxetine (Prozac) and sertraline (Zoloft) - therapy may be required for several months or longer - symptomatic relief may require 1-4 weeks and there is prolonged elimination of drug *SSRI do not significantly affect cognition in older adults - Fluoxetine and escitalopram (Lexapro) only antidepressants recommended for treatment of MDD in 12-17 years old - Fluoxetine approved for children 8 years and older |
|
|
Side effects of SSRIs (Fluoxetine and sertraline ) - sexual dysfunction - nausea and other GI effects (most common during first 2 weeks of therapy but often transient) - anorexia and sweating, insomnia, anxiety, nervousness, tremor, drowsiness, fatigue, dizziness, and headache - bleeding (impaired platelet aggregation, hyponatremia(low sodium levels), QT prolongation with citalopram (Celexa) doses >40 mg per day that can lead to abnormal heart rhythm - can be fatal Caution: - liver, renal impairment, suicide prone, diabetes, bipolar disorders (may precipitate manic attacks) - underweight, eating disorders, pregnancy and lactation, abrupt discontinuation Interactions: - MAOIs (never take concurrently)** - amphetamines, most antidepressants, certain analgesics (fentanyl, tramadol), antiemetics (metoclopramide), antimigraines ("triptans", antibiotics (linezolid) and OTC products (dextromethorpha, St. John's wort, tryptophan) - can result in serotonin syndrome- potentially life-threatening reaction to excessive serotonin activity in CNS - anticoagulants, antiplatelet drugs, NSAIDs and aspirin (increased risk of bleeding complications) |
Selective Noreinpinephrine Reuptake Inhibitors (SNRI) - Inhibit reuptake of serotonin and norepinephrine - Examples: Duloxetine (Cymbalta) and venlafaxine (Effexor) - also effective in patients with chronic pain (neuropathic pain, fibromyalgia, and musculoskeletal pain) - Desvenlafaxine (Pristiq) also SNRI, major metabolite of venlafaxine, equiactive and equipotent to its parent compound. 0 indicated for treatment of MDD. (warnings, problems, precautions similar to other SNRI) |
|
|
Heterocyclic Antidepressant - Comparable efficacy to first-generation tricyclic antidepressants, - Differing effects on dopamine, norepinephrine, and serotonin - Distinctly different adverse effect profiles - Examples: bupropion (Wellbutrin) and mirtazapine (Remeron) - Bupropion (Wellbutrin) an activating antidepressant (like most SSRIs) can be useful in cases of severe depression characterized by extreme fatigue, lethargy, and psychomotor retardation. useful in helping reduce relapse rates in person who are quitting smoking (Zyban) |
Heterocyclic Antidepressants Mirtazapine (Remeron) - calming antidepressant that can be useful in treating agitated depression, mixed anxiety depression, and fibromyalgia - common side effect: weight gain. Trazodone is highly sedating and used in low doses as hypnotic- can be useful in higher doses in older adults for treating agitation secondary to dementia and treating activation side effects caused by SSRIs. |
|
|
Side effects of heterocyclic antidepressants - drowsiness- common (except bupropion) - dry mouth, nausea, dizziness and confusion - priapism or impotence (trazodone; discontinue drug) - weight gain (mirtazapine, trazodone) Interactions: - other CNS depressants, including alcohol, may potentiate sedation (mirtazapine, trazodone) or increase risk of seizures (bupropion) MAOIs (never take concurrently) food may decrease incidence of light-headedness Caution: - patients who are suicidal - patients who are anorexia, and bulimia (buproprion) - seizure disorder - cardiac or liver disorders |
Antimanic Agents - Bipolar disorder: Mental illness characterized by severe fluctuations in mood extremes - Patients may experience high (mania) and low (depression) mood swings with a diminished capacity for daily functioning - most likely imbalance in brain chemicals affect mood - without treatment, bipolar disorder is a debilitating condition that will not improve on own. drugs; Lithium, |
|
|
20-2 antidepressants page 384 tricyclics MAOIs SSRIs SNRIs Heterocyclics |
Lithium (Antimanic) - Prevents manic episodes when compared with depressive episodes - approved for treatment of mania and prophylaxis of bipolar disorder. - the only mood stabilizer that has LOWERED SUICIDE rate in bipolar patients - maintenance dose est by monitoring blood levels - serum levels checked 7 days after starting or changing lithium dose and every 6-12 months once stable dose established, maintain level of 0.8-1.2 mEq/mL (must be monitored for signs of toxicity |
|
|
Side Effects of Lithium - GI distress (usually initially and resolves - take medicine with meals) - cardiac arrhythmias and hypotension - thirst and polyuria (dehydration may cause acute toxicity - weight gain - tremors (can be treated with propranolol) - thyroid problems- hyperthyroid goiter Signs of lithium Toxicity - tremors, muscle weakness, seizures, coma, and cardiovascular collapse Caution: - seizure disorders and parkinsonism - cardiovascular and kidney disorders - older adults and debilitated patients - thyroid disease |
Interactions of Lithium - occur with CNS drugs, most antidepressants , diuretics, NSAIDS, ACE inhibitors and sodium salts - anticonvulsants valproate (Depakote, Depakene), lamotrigine (Lamictal) and carbamazepine (Tegretol) used for mood stabilization in bipolar illness - Symbyax (combo of atypical antipsychotic olanzapine and SSRI fluoxetine - first FDA approved for depressive phase of Bipolardisorder) |
|
|
Table 20-3 Antimanic Agents pg 386 lithium cabamzepine - lamotrigine - valproate - olaznapine.fluoxetine |
Anxiolytics Types of anxiety disorders - Social anxiety, post-traumatic stress disorder, (PTSD) panic attacks, and obsessive compulsive behavior - become disorder when excessive and difficult to control and leads to sig distress and impairment Benzodiazepines, (short term use only) |
|
|
Anxiolytics Benzodiazepines (BDZs) - For short-term treatment of anxiety disorders, some psychosomatic disorders and insomnia, and alcohol withdrawal - Examples: diazepam (Valium), clonazepam (Klonopin), and midazolam (Versed) - Diazepam (Valium) used as muscle relaxants (anticonvulsants in preprocedure testing, or preoperatively for sedation induction) - Clonazepam (Klonopin) primarily manage seizures also used treat panic disorder - Anxiolytic BDZ, give small doses can reduce anxiety and promote relaxation without causing sedation, large doses: use at bedtime for sedative effect - role of BDZ in treating anxiety disorder= provide acute relief of anxiety symptoms while waiting for long-term treatment (SSRI or SNRI antidepressants) - BDZ do not treat underlying cause of anxiety (abnormality of NT) but mask symptoms |
Minor tranquilizers should not be taken for prolonged periods of time - tolerance and physical and psychological dependence may develop. - Alprazolam (Xanax) most abused BDZs, due to quick onset of action - leads to Euphoria **ALL BDZs (Anxiolytic) are Schedule IV controlled Substances** - sudden withdrawal (missed doses/discontinuation) after prolonged use of Anxiolytic may result in: seizures, agitation, psychosis, insomnia and gastric distress - BDZs wtih long half-life (clrazepate (Tranxene) and diazepam should be avoided in older Adults. - Oxazepam (Serax) and lorazepam (Ativan) have medium to short half-lives and inactive metabolites and less prone to accumulation in older adult patients or those with liver disease. |
|
|
Side Effects of BDZs Benzodiazpines - depression, hallucinations, confusion, agitation, bizarre behavior, and amnesia - drowsiness, lethargy and headache - ataxia and tremor - increased risk of falls in older patients by ~50% - rash and itching - sensitivity to sunlight Precautions or Contraindications - mental depression, suicidal tendencies, history of substance abuse, depressed vital signs pulmonary disease and respiratory depression - pregnancy and lactation, children, liver and kidney dysfunction, older adults and debilitated patients (paradoxical reactions) and prolonged elimination time, persons operating machinery - Interactions with potentiation effect may occur CNS depressants (analgesics, anesthetics, sedative hypnotics, other muscle relaxants, antihistamines, and alcohol) *potentially lethal overdose when BDZs mixed with alcohol or opioids* antiretroviral protease inhibitors, macrolides (erythromycin), azole antifungals (ketoconazole, itraconazole), oral contraceptives, calcium channel blockers (dilitiazem, verapamil) all reduce elimination ofmost BDZs. - lead to increased and excessive sedation or impaired psychomotor function - Phenytoin (potentiation of phenytoin by raising serum concentration) Grapefruit juice (can potentiate effects of orally administered alprazolam, midazolam and diazepam and should not be taken concurrently) |
Midazolam (Versed) potent BDZ - used preoperatively to relieve anxiety and provide sedation, light anesthesia, amnesia of operative events. - more rapid onset of sedative effects and more pronounced amnesic effects during first hour following administration, = drug of choice for short surgical procedures. - usually administered IV and duration of amnesia is about 1h. - also used orally for preoperative sedation and relieve anxiety with good results |
|
|
Midazolam (BDZ) - may be used alone or in combo with opioid (fentanyl for painful procedures - endoscopy and cardiac catheterization with or without intervention. - used IV for induction of general anesthesia along with opioid - potent sedative requires individualized dosage with adjustment for age, weight, clinical condition and procedure Side Effects of Midazolam - depressed respiration with large doses, esp in older adults with those COPD , paradoxical reactions (agitation or involuntary movements) occur occasionally) nausea and vomiting (occasionally) Cautions: - watch for apnea, hypoxia, and or cardiac arrest - respiratory status should be monitored continuously during parenteral use - facilities and quip for respiratory and cardiovascular support should be readily available: vital signs should be monitored carefully for changes in blood pressure or decreased in heart rate - patients with electrolyte imbalance, renal impairment and congestive heart failure and children are at increased risk complication. Contraindicated: -- in pregnancy and those with acute narrow-angle glaucoma Interactions: can potentiate possible respiratory depression - Cimetidine (Tagamet) and ranitidine (Zantac), same meds listed under BDZs |
Other Anxiolytics Buspirone (BuSpar) - Indicated for treatment of generalized anxiety disorder, but not other anxiety disorders (or depression) - unlike the BDZs, buspirone has no anticonvulsants or muscle relaxant activity, does not substantially impair psychomotor function and has little sedative effect. - indicated for treatment of generalized anxiety disorder but not other anxiety disorders, does not have activity against depression. (may be effective for cognitive and interpersonal probs) Hydroxyzine (Vistaril) - Used IM as a pre- and postoperative antiemetic and sedative, and antipruritic Side Effects of Hydroxyzine (generally anticholinergic may include) - drowsiness, ataxia, and dizziness - urinary retention and mydriasis Caution - GI, Hepatic, respiratory, and urinary disorders - closed-angle glaucoma - older adults - pregnancy (esp first trimester) |
|
|
Table 20-4 Antianxiety meds (Anxiolytics) pg 389 alprazolam chlordizaepoxide clorazepate diazepam -lorazepam - midazolam - oxazepam Other Anxiolytics: busipirone, hydroxyzine |
Antipsychotic Medications / Major Tranquilizers - aka Neuroleptics (consist of traditional or typical (first-gen) and newer or atypical (second gen) agents - Work primarily by blocking dopamine receptors = Results in unbalanced cholinergic activity - Causes frequent extrapyramidal side effects to include tardive dyskinesia - Two ways useful 1. Relieving symptoms of psychoses (delusion, hallucinations, agitation and combativeness) 2. Relieving nausea and vomiting (prochlorperazine (Compazine)) Most typical Antipsychotics: Phenothiazines (chloropromazine -Thorazine) or butyrophenone derivatives haloperidol (Haldol) - dosage regulated to modify disturbed behavior and relieve severe anxiety in profound impairment of consciousness = block dopamine receptors (antiemetic effects) but results in unbalanced cholinergic activities cause frequent extrapyramidal side effects (EPS) to include tardive dyskinesia (TD) |
|
|
Extrapyramidal system (EPS) - controls equilibrium and muscle tone - can include muscle rigidity; tremors; difficulty walking and involuntary, repetitive and purposeless body movements = Tardive Dyskinesia Typical Antipsychotics (Phenothiazines) still commonly used in acute hospital setting because they are only medication in this class available for IV administration |
Antipsychotic Medications / Major Tranquilizers other class: Atypical Antipsychotics - risperidone: different from phenothiazines (block both serotonin and transiently blocking dopamine receptors) = results in less potential for adverse effects (EPS and TD) - direct antagonism at serotonin receptor (histamine-1receptor) may account for weight gain and other metabolic abnormalities with atypical agents - The use of Clozaril is limited to schizophrenia unresponsive to conventional therapy because of concerns with agranulocytosis. - The newest agent is Invega, a metabolite of Risperdal. - Thorazine is also used in the treatment of intractable hiccups. |
|
|
Antipsychotics helpful in treating behavioral and psych symptoms of dementia - typical or atypical antipsychotic drugs not FDA approved (black box warning) for treating geriatric patients with dementia-related psychosis. - cerebrovascular adverse events, include fatalities reported in older adults with dementia related psychosis (Alzheimer's, vascular and mixed) being treated with antipsychotics * use lowest effective dose for shortest duration (antipsychotics for dementia-related behaviors)* |
Side effects of Antipsychotics - low-potency: chlorpromazine and thioridizaine more likely to produce sedation, hypotension and anticholinergic effects - remaining typical high-potency agents (haloperiodol, fluphenazine and trifluoroperazine) likely to produce EPS Side Effects of all antipsychotics may include - Anticholinergic effects dry mouth, constipation, urinary retention, blurred vision, - fever, confusion, restlessness, agitation, and headache - Jaundice, rash, photosensitivity or hypersensitivity reactions, - prolactin elevation with typicals, Agranulocytosis with clozapine (can be fatal), - metabolic effects (increased risk of hyperglycemia, insulin resistance, diabetes, weight gain, elevated cholesterol) with atypicals - Extrapyramidal side effects, severe CNS adverse effects include: Parkinsonian symptoms (ex tremors, drooling, dysphagia (more common in older adults) - TD (involuntary and maybe irreversible, abnormal orofacial movements (tics- more common in older female adults) - Dystonic reactions (spasms or abnormal muscle tone of head, neck, or tongue - more frequent in children) - Akathisia (uncontrollable motor restlessness- more common in children). |
|
|
Treatment of Parkinsonian Symptoms - concomitant administration of an anticholinergic antiparkinsonian agent (Artane or Cogentin) - prophylactic administration of these drugs will not prevent extrapyramidal symptoms. These drugs will not alleviate symptoms of TD and can make them worse. - Dystonic reactions usually appear early in therapy and subside rapidly when antipsychotic drug is discontinued = Trihexyphenidyl (Artane), benztropine (Cogentin) or diphenhydramine (Benadryl) treat dystonic reactions. |
Precautions/Contraindications for Antipsychotics - Seizure disorders, Parkinsonian Syndrome, Cerebrovascular disease, Severe depression, Pregnancy, blood dyscrasias, older adults and children, hepatic, cardiovascular and renal diseases, prostatic hyperplasia and diabetes Interactions: - potentiation with CNS depressants, anticholinergics and antihypertensives - drugs that prolong QT interval and increase risk of life-threatening cardiac arrhythmias (antiarrhythmic agents, dolasetron, certain quinolones) with phenothiazines and ziprasidone. - Dopamine antagonists (metoclopramide or promethazine) which increase risk of TD and EPS - Antagonism with anticonvulsants (seizure activity may increase)) |
|
|
Patient Education for Antipsychotics - compliant with meds and non med therapy - potential for psychological and physical dependence (with prolonged use) - report adverse side effects to physician at once (dizziness, blurred vision, nervousness, palpitations and other cardiac symptoms, urinary retention, GI symptoms, adverse mental changes and EPS) - avoid chemical abuse (alcohol, nicotine, or drugs) and obtain professional treatment - possible severe withdrawal reactions (seizures) after prolonged use of psychotropic meds (withdrawal should never be abrupt, med supervision) - caution with interaction (not taking other meds that can potentiate CNS depression (analgesics, alcohol, muscle relaxants, antihistamines, antiemetics, cardiac medications or antihypertensives) - Not taking Grapefruit juice with BDZs esp alprazolam and diazepam - older adults more at risk for side effects mentioned earlier (slowed metabolism and cardiovascular, kidney, liver, and visual impairment) - rise slowly (potential hypotension) - avoid operating machinery or driving while taking drugs - Avoid taking OTC drugs or herbal supplements without med supervision |
Antipsychotic med/ major tranquillizers table 20-5 pg 395 - Typical: Phenothiazines (chlorpramazine, fluphenazine, perphenazine, prochlorperazine, thioridazine, trifluoperazine) Butryrophenone - haloperidol (for agitation, esp with schizophrenia and delusions in older adults) - Atypical: aripiprazole, clozapine, olanzapine, paliperidone, quetiapine, risperidone, ziprasidone |
|
|
Antipsychotic Medications/Major Tranquilizers - Atypical antipsychotics = Block both serotonin and transiently block dopamine receptors = Less potential for adverse effects - There is no “ideal” antipsychotic medication - Both conventional and atypical antipsychotic medications are associated with significant adverse drug reactions |
Drug Abuse - What is drug abuse? = The use of a drug for other than therapeutic purposes - What is drug addiction? = A combination of tolerance, psychological dependence, physical dependence, and withdrawal syndrome with physiological effects |
|

|
|
|
|
|
|
|
|
|
|
Drug addiction -- combination of all 4 of following: tolerance, psychological dependence, physical dependence, withdrawal syndrome with physiological effects - habituation consist of psychological dependence only. - Chemical dependency: condition in which alcohol or drugs have taken control of an individual's life despite problems related to use and affect normal functioning. |
Alcohol (ethyl alcohol, ethanol) - Classified as a psychotropic drug and a CNS depressant - Number one drug problem in the U.S. - fast acting depressant - body reacts to alcohol with excitement, sedation, and finally anesthesia. - large amounts = alcoholic stupor, cerebral edema and depressed respiration. - alcohol is rapidly absorbed from GI tract into blood stream - depresses primitive areas of cortex first and then decrease control over judgment, memory and other intellectual and emotional functioning. - within few hours motor areas affected: producing unsteady gait, slurred speech and incoordination. - prolonged use can cause permanent CNS damage results in peripheral neuritis, convulsive disorder (seizure?), Wernicke's syndrome, and Korsakoff's psychosis with mental deterioration, memory loss and ataxia (loss of full control of body movements) - Prolonged use affects almost all organs - chronic drinking = liver damage and pancreatitis - alcohol irritates mucosa of digestive system, = gastritis, ulceration and hemorrhage. - alcohol can lead to malabsorption of nutrients and malnutrition. - cardiovascular effects: peripheral vasodilation (flushing, sweating with intoxication), and vasoconstriction of the coronary arteries - increases heart rate and with chronic use can cause cardiac myopathy, (directly or thru metabolic and electrolyte imbalances) - Potassium deficiency can cause cardiac arrhythmias |
|
|
Alcohol Poisoning - Symptoms include cold, clammy skin; stupor; slow, noisy respirations; and alcoholic breath - Mortality associated with acute alcohol poisoning alone is uncommon, but can be an important factor when mixed with recreational drugs - Treatment = respiratory problems (establish and maintain airway), vomiting (prevent aspirations), seizures (do not require treatment unless status epilepticus occurs), cerebral edema (diuretics sometimes required (mannitol), Electrolyte imbalance (IV fluids with thiamine, folic acid, magnesium sulfate and vitamins added (banana bag), Alcohol withdrawal syndromes and delirium tremens (treated with IV BDZs)
|
Fetal Alcohol Syndrome (FAS)
- teratogenic effect of ethanol - as 2 drinks early in pregnancy - more commonly seen in infants whose mother's consume 4 or 5 drinks per day. |
|
|
Chronic alcoholism - Symptoms = frequent falls and accidents, blackouts and memory loss, dulling of mental facilities, neuritis and muscular weakness, irritability, tremors, conjunctivitis, Gastroenteritis, neglect personal appearance and responsibilities - Treatment: can include an intensive in-house rehabiliation program in treatment facilities - Vitamin B (thiamine) IV, IM or PO; multiple vitamins and golic acid - low carb and high protein diet to combat hypoglycemia - elimination of caffeine (coffee, tea, chocolate and soft drinks) - Reeducation of patient, with intensive individual, group and family counseling, including Alcoholics Anonymous techniques Pharmacologic Therapy - (disulfiram (Antabuse)) use with patient cooperation part of "behavior modification", patient taught to receive daily dose of disulfiram and taught to expect very unpleasant reaction if even small amount of alcohol is ingested - treatment used less frequently because of severe reaction potential and poor compliance |
Disulfiram-alcohol reactions - flushing and throbbing headache - nausea, vomiting and metallic aftertaste - sweating and dyspnea - palpitation, tachycardia, and hypotension - vertigo, and blurred vision - Anxiety and Confusion Patient ed taking Disulfiram - not taking within 12 hour of alcohol containing prep - avoid cough syrups, sauces, vinegars, elixirs and other prep containing alcohol - caution with external app of liniments, lotions, aftershave or perfume - signs of disulfriam-alcohol reaction - reporting to emergency facility if effects do not subside or with severe reaction - carry identification card noting therapy - avoiding other meds that may interact with disulfiram (metronidazole, anticoagulants and phenytoin) - |
|
|
another treatment for alcoholism: daily maintenance doses of naltrexone (ReVia) part of counseling program - keep alcoholics sober after detox. (naltrexone is long-acting opiate antagonist, acts by blocking pleasurable sensation associated with alcohol (and opiates) and lessen desire or craving. = reduces frequency and risk of heavy drinking, but does not necessarily enhance abstinence. (better tolerated than disulfiram) Side Effects of Naltrexone - GI side effects and decreased appetite - headache, dizziness, and anxiety - nausea, and joint pains - liver damage occur with larger doses than recommended (of 50mg daily) Caution: if given to someone currently dependent on opiates, can send addict instantly into severe, life-threatening withdrawal, initiate therapy only if opiate free for 7-10 days |
Prescription drug abuse - Nation's fastest growing drug problem - Second most-abused category of drugs after marijuana - According to the CDC, death rates from opioid overdoses have more than tripled since 1999 - Rx drugs most often abused by medical personnel are hydrocodone, oxycodone, and the BDZs. - Treatment: opiate addiction (fentanyl, oxycodone, hydrocodone etc) = consist of combo counseling, behavioral therapy and meds. = Methadone, naltrexone and buprenorphine are meds approved for treatment of opiate addiction - Methadone - sublingual buprenorphine (Subutex - partial opioid antagonist) and buprenorphine with opiate receptor antagonist naloxone (Suboxone) can be used during detoxification process and for maintenance treatment - Naltrexone (ReVia) pure opioid antagonist used maintain therapy to block pleasurable effects of opiates |
|
|
Illegal Drug Abuse 4 types substances produced illegally - amphetamines, marijuana, cocaine, and hallucinogens (LSD and PCP) |
Amphetamines -Examples: methamphetamine (“crystal,” “crank,” “ice,” “meth,” “speed”) and methylenedioxymethamphetamine (MDMA, “Ecstasy”) - at normal dosage levels, admin of amphetamine may produce tolerance within a few weeks. - in hypersensitive individuals: psychotic syndrome may occur within36-48 h of a single large dose (some emotionally unstable depend on pleasant mental stimulation) |
|
|
Symptoms of Chronic Abuse of amphetamines - emotional lability, irritability, - anorexia - mental impairment, confusion, amnesia, and neurotoxicity - occupational deterioration and social withdrawal - continuous chewing or teeth grinding - resulting in trauma or ulcers of tongue and lip - photophobia- frequently wearing sunglasses indoors - Paranoid syndrome with hallucinations with prolonged use of high doses - Tooth decay ("meth mouth") Symptoms of acute toxicity - strokes, cardiovascular symptoms (flushing or pallor, palpitation, tachypnea, tremor, extreme fluctuations of pulse and blood pressure, cardiac arrhythmias, chest pain, circulatory collapse) - dilated pupils, diaphoresis and hyperpyrexia - mental disturbances (confusion, delirium, belligerence, combativeness, restlessness, paranoia, and suicidal or homicidal tendencies) - fatigue and depression usually follow CNS stimulation Treatment: - no specific antidote for overdose - symptomatic and includes attention to airway, breathing, circulation and administration of sedative drugs (BDZs) - treatment for shock or cardiac irregularities - admin of activated charcoal may help if admin within 1-2 hour after substance ingested. - external cooling devices may be used to treat hyperthermia since antipyretics are not effective in this situation. - abrupt withdrawal of amphetamines may unmask mental problems (patients require careful supervision during withdrawal and long-term followup since some manifestations(depression) may persist for prolong period. - Combat Meth Epidemic Act 2005 (banned OTC sales of ingredients commonly used to make methamphetamine) - PSE pseudoephedrine- popular effective oral nasal decongestant primary target. can be stored and sold under special conditions (behind counter) |
DEA classified MDPV Methylenedioxypyrovalerone (bathsalts, isomers and salts of isomers) = Schedule I substances = illegal for anyone to sell or be in possession of these products |
|
|
Marijuana Active ingredient: Tetrahydrocannabinol (THC) - classified as a CNS depressant (possess properties of euphoriant, sedative and hallucinogen) - Marinol (dronabinol- synthetic form of THC) approved for prevention of chemotherapy-induced nausea and vomit - used as appetite stimulant in cachexia associated with AIDS/Cancer - Cannabis: difficult to evaluate potential therapeutic effects for certain disorders, illegal under federal law. - Medical marijuana = 1. severe nausea, 2. weight loss associated with debilitating illness, 3. spasticity secondary to neurologic diseases, 4. pain syndromes and 5. glaucoma. |
THC active ingredient released in marijuana is smoked = fat soluble and stored in many fat cells (esp in brain and reproductive organs) - THC metabolizes slowly - a week after person smokes one marijuana cigarette, 30-50% of THC remains in body and 4-6 weeks required to eliminate all THC. |
|
|
Side effects of marijuana - short-term memory loss, impaired learning, and slowed intellectual performance - perceptual inaccuracies, and impaired reflex reaction (dangerous with driving) - apathy (lack of interest), lethargy and decreased motivation - increased heart rate, anxiety and panic attacks - lung irritation, chronic cough, frequent respiratory infection - reduced testosterone level and sperm count - reduced estrogen level, crossing placental barrier and transmission through mother's milk; miscarriage and stillbirth possible - delayed development of coping mechanisms in children and adolescents Newer illicit drug class (synthetic cannabinoids "spice" K2, skunk, fake weed. - smoking for hallucinogenic effects - somecases stronger and unpredictable effects (rapid heart rate, hypertension, seizures, acute kidney injury and myocardial ischemia and some associated with heart attacks) - high potential for abuse and no medical benefit - DEA scheduled I controlled substances (illegal to sell, buy or possess) just like Bath Salts |
Cocaine CNS stimulant - Produces euphoria and increased expenditure of energy - Highly addictive (cause dependence after short time use) - abused intranasal application (sniff or short), intravenous injection or inhalation (smoking crack) - nasal app can damage mucous membranes and or nasal septum. - effects of IV extremely rapid and dangerous - can be fatal - smoking causes addiction, sometimes after 1 use - only approved medical use: local anesthetic (applied topically only) to mucous membranes of the laryngeal, nasal and oral cavities - cocaine crosses placental barrier - babies who are irritable, jittery, anorexic and seizure prone. - severe depression can be associated with withdrawal (lengthy and difficult) Side effects: - Euphoria, agitation, excitation, hypertension, chest pain, tachycardia, cardiac arrhythmias, or cardiac failure - anorexia, nausea, and vomiting - tremor and seizures - hallucinations, possible psychosis and possible violent behavior - respiratory failure, strokes and possible death from circulatory collapse - perforated nasal septum from prolonged nasal use |
|
|
Hallucinogens - Produce bizarre mental reactions and distortion of physical senses - Examples: lysergic acid (LSD) and phencyclidine (PCP), animal tranquilizer - hallucinations and delusions common with confused perception of time and space - PCP is also amnesic (partial or total loss of memory) Side effects: - increased pulse and heart rate and rise in blood pressure and temperature - possible flashbacks months later - panic or paranoia (lack of control) - possible psychotic episodes; chronic mental disorders - possible physical injury to self and others |
Dextomethorphan (DXM) - Semisynthetic morphine derivative - Safe, effective, nonaddictive, OTC cough suppressant when used appropriately - Often abused by teens because of its phencyclidine-like euphoric effect- and abuse may be associated with psychosis and mania - abuse can be serious, can cause serious adverse events (brain damage, seizure, loss of consciousness, irregular heartbeat and even death) |
|
|
Flunitrazepam (Rohypnol) - Potent benzodiazepine approved for use in Central and South America for ethanol withdrawal -Known on the street as “roofies” and the “date-rape drug” - not approved in US- used as recreational drug (sometimes snorted to offset cocaine withdrawal) - also acquired "date-rape drug" due to its ability to induce amnesia, preventing victim from recalling specific events while under influence. |
The Role of Medical Personnel - Have a thorough knowledge of psychotropic drugs, action, and side effects - Be willing to participate in the education of the patient, patient’s family, and others - Give competent care to those under the influence of drugs in a nonjudgmental way - Recognize drug abuse and make appropriate referrals without exception - Keep complete and accurate records of controlled stocks of drugs that could be considered potential drugs of abuse - Report any observed drug abuse to the proper person in authority |
|
|
Fifteen-year old Adan has major depressive disorder. which antidepressant is recommended for treating major depressive disorder in adolescents? = escitalopram |
Franklin is taking an antipsychotic that acts by blocking serotonin receptors and transiently blocking dopamine receptors. What antipsychotic might he be taking? = clozapine |

