![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
31 Cards in this Set
- Front
- Back
|
ANTI-DEPRESSANT ERA |
•Antidepressants for adults constitute a multibillion dollar market globally •in the last five years, prescriptions for children have increased at an exponential rate |
|
|
General facts |
•When antidepressants were introduced 40 years ago ( MAOIs ), medications were used primarily to treat depression •currently, antidepressants are used to treat a variety of disorders, including anxiety, impulsive aggression, and chronic pain •current literature and practice indicate that all the different classes of antidepressants are about equally effective |
|
|
good news/bad news |
-Good –one half to two thirds of depressed clients on any antidepressant respond positively to it; half may progress into full remission within six months of treatment; antidepressants seem to significantly reduce relapse. -Bad –many responders on meds never reach full remission; 20-30% tend to "poop out"or wear off after about 18 months on antidepressants |
|
|
Clinically, "normal" mood is referred to as |
-a state of Euythmia -concept has two different meanings: a clinical state where one is neither manic or depressed; tranquil or joyous state of mind -mood assessment is the practice of understanding mood state and introducing pharmacologic agents to keep clients’moods within parameters clinically described as "normal"or "euthymic" -elevated mood above normal is not described as pathological on the DSM IV, TR, until it reaches Hypomanicstatus
|
|
|
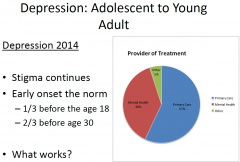
Depression: Adolescent to YoungAdult |
|
|
|
History of Classification labels used to identify Depression |
•Melancholic depression •Severe depression •Reactive/situational depression •Neurotic depression •Personality disorder w/depression •Dysthymia •Disruptive mood dysregulation •Persistent Depressive Disorder •Major Depressive Disorder •Premenstrual Dysphoric Disorder •Substance/Medication Induced Depressive Disorder |
|
|
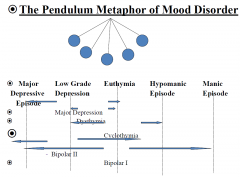
The Pendulum Metaphor of Mood Disorder |
|
|
|
Characteristics of Mood Disorder |
-Major depression, also called unipolardepression is characterized by recurring episodes of dysphoriaand negative thinking that also reflected in behavior. -Bipolar disorder is also cyclic but moods swing from depression to mania over time -Mood disorders are among the most common forms of mental illness currently -Mood disorder is so severe that the individual withdraws from life and social interactions |
|
|
Characteristics of Mood Disorder 2 |
•If left untreated, most episodes of unipolar disorders improve in about six to nine months, however reoccur throughout life often increasing in frequency and in intensity in later years. •Later episodes of depression are more likely to occur without the influence of psychosocial stress •Mania rarely occurs alone but rather alternates with periods of depression to form bipolar disorder •The primary symptom of mania is elation |
|
|
Common Vegetative Symptoms in Major Depressive Disorder |
Sleep disturbance (early morning waking, frequent awakening, occasional hypersomnia) |
|
|
Characteristics of Mania |
•Individuals with mania typically feel faultless, full of fun, and bursting with energy: need for sleep is significantly reduced, tend to be more talkative than usual, and experience racing thoughts and ideas.; tend to make impulsive decisions in a grandiose way and have unlimited confidence; becomes involved in activities that have a high potential for negative consequences such as foolish business investments, wreckless driving, buying sprees, or sexual indiscretions |
|
|
What is Bipolar Disorder? |
•It is cyclic brain disorder with recurrent fluctuations in mood, energy, and behavior. |
|
|
Myths of Bipolar Disorder |
•Uncommon disorder |
|
|
Unipolar VS. Bipolar |
Uniporlar •Diagnosed when there are problems of depressed mood, but there is no reported history of any manic episodes, hypomanic episodes, or mixed episodes Bipolar •Diagnosed when there is a presence of at least one/any manic, hypomanic, or mixed episode. |
|
|
Diagnosing Depression |
•Differentials |
|
|
Diagnosis: What are the Indicators of Bipolar Disorder? |
•Indicators of BD |
|
|
Bipolar Disorder |
•Considerable psychiatric comorbidity |
|
|
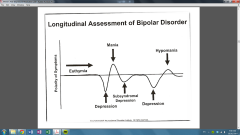
Longitudinal Assessment of Bipolar Disorder |
|
|
|
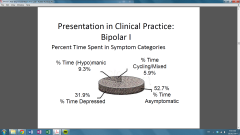
Presentation in Clinical Practice: Bipolar I |
|
|
|
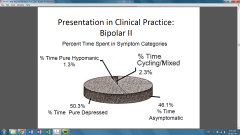
Presentation in Clinical Practice: Bipolar II |
|
|
|
Rapid Cycling |
•Frequency of cycled less than three days |
|
|
Diagnostic Issues for Depression:Is it Unipolaror Bipolar? |
•Compared with unipolar, depression in BPD patients associated with: |
|
|
The Mood Disorder Questionnaire (MDQ) |
•Validated for adolescents and adults |
|
|
Major Goals for Treatment in Bipolar Disorder |
•Prevent future episodes of mania |
|
|
Why Treat Bipolar Disorder with Psychotherapy? |
•Increase adherence to medication |
|
|
Empirically Tested Psychotherapies for Bipolar Disorder |
•Cognitive Behavioral Therapy (CBT) |
|
|
Reasons for Nonadherance |
•Forgetting to take dose |
|
|
Interventions to Improve Adherance |
•Most effective interventions only lead to small improvement in adherence or outcomes |
|
|
Bipolar Maintenance: General Management |
•Maintain medication •Train to monitor for prodromal symptoms |
|
|
Summary (BIPOLAR) |
•The evidence base for the treatment and maintenace of bipolar disorder depression is relatively weak, and practice guidelines differ
|
|
|
Drug Treatment for Bipolar Disorder |
•Lithium Carbonate is treatment of choice |

