![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
49 Cards in this Set
- Front
- Back
|
Ecf versus ICF make up how much percentage each total body fluid.
EC is broken up into what to components? Are they alike in composition ? |
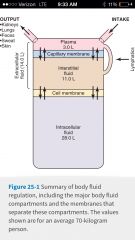
ECf: one third icf : 2/3 rd
ECf is made of plasma and interstitial fluid. Yes they are alike in composition. But icf is different |
|
|
Five areas that we lose water through ? Where do we lose most of our water from ?
Do we only lose water through these places? So because we lose sodium through these five areas what does that mean? |
Kidneys, lungs, feces, sweat, skin.
Most is lost through urine! No we also lose electrolytes! It means that we need some sodium intake in our diet. |
|
|
Fluid and electrolyte balance are necessary to maintain what?
Therefore fluid loss and electrolyte loss have to equal what and what? |
To maintain life.
Fluid loss equals food intake. Electrolyte loss equals electrolyte intake. |
|
|
Fluid intake is regulated by?
Electrolyte intake is regulated by? Fluid output Is regulated by? Electrolyte output is regulated by? |
Fluid intake is regulated mainly by thirst mechanism and habits.
Electrolyte intake is a regulated by dietary habits Fluid output is regulated mainly By kidneys Electrolyte output is maintained by the kidneys. |
|
|
Do we get all of the water in our body from ingesting it?
|
No we also produce water from Burning carbohydrates and the beta oxidation of fatty acids.
|
|
|
Do we get all of the water in our body from ingesting it?
|
No we also produce water from Burning carbohydrates and the beta oxidation of fatty acids. This is how bears hibernate in the winter.
|
|
|
Extreme heat and exercise do what to the kidneys? What could this result in? So we need to do what? Why? What two things are very important to kidneys?
|
Heat And exercise equals extreme sympathetic response which equals efferent arteriolar construction which equals less blood flow to kidneys . This could equal renal failure. We see it a lot in firefighter training. So we need to stay hydrated ! Because two things that are very important to kidneys are maintaining blood volume and maintaining blood pressure.
|
|
|
Extreme high sodium meal means and increase in what? Therefore we take in more what? Ie: Chinese example
|
Hi sodium intake equals increased thirst which equals ingestion of more water. This is why we feel like we are hungry shortly after eating very salty Chinese food. We are not actually hungry were really thirsty but our brain cannot recognize the difference.
|
|
|
Food balance during heavy exercise;
Fluid ingested needs to be increased or decreased? What happens in the loss of water and electrolytes through insensible loss , sweat and in urine? |
Fluids need to be increased to maintain balance. We would sweat more hAve more insensible loss through the lungs but NOT through the skin and May pee less during heavy exercise.
|
|
|
How does obesity relate to body water percentage? What about infancy? What do we need to remember about these patients? What about age?
|
Obese patients have a smaller body water percentage because fat contains less water . Older patients have less percentage of body water. Loss of lean mass equals less muscle. Muscle holds lots of water.
Infants have a higher water percentage. But remember they are tiny so a half liter in or out makes a big difference so they can become dehydrated very quickly although they are mostly water. |
|
|
Balance between ECf and ICF are maintained at what membrane? What is this membrane made of? what can get through this membrane? How do electrolytes get through this membrane? What is one of the main reasons that potassium is inside of the cell and sodium is mostly outside the cell?
|
The balance is maintained at the cell membrane? The cell membrane is a phospholipid bilayer. Electrolytes get in and out through channels. only small molecules can just diffuse through.
Because the sodium potassium pump is always running. |
|
|
Distribution across cell membranes is determined by what?
Distribution across capillaries is determined by what? |
Distribution across cell membranes is determined by osmotic forces mainly from electrolytes.
Distribution across capillaries is determined by hydrostatic and colloidal osmotic forces. |
|
|
Why does water move out at the arterial end of the capillary bed and move back in at the venous end?
|
It's because there is increased hydrostatic pressure at the arterial end and increased colloidal osmotic pressure due to the plasma protein at the venous end
|
|
|
What is the osmotic pressure formula?
If C = mOsm/L then Pi equals C times ______ mmHg |
pi = CRT
C = concentration (osm/liter) R = gas constant (62.3 if pi equals mmhg) T= in Kelvin equals 310° Pi= 19,300 mmHg/osm So if C =mOsm/liter then Pi =C x 19. 3 mmHg |
|
|
Why do hydrostatic pressure differences only have a small effect on fluid movement across the cell membrane?
|
It's because the intracellular fluid and the extracellular fluid do not have a big pressure difference that therefore there is not a large pressure gradient.
|
|
|
What is the osmolarity of Isosmotic fluids versus hyperosmotic fluids versus hypoosmotic fluids when compared to the body fluids?
|
Isosmotic fluids have the same osmolarity as body fluids.
Hyper osmotic fluids have a higher osmolarity than body fluids. Hypo-osmotic fluids have a lower osmolarity then body fluids. |
|
|
What is the osmolarity of a 5% glucose solution? Is it ISO , hypo, or hyper osmotic?
|
The molecular weight of glucose equals 180 g per mole . 5% glucose equals 5 g / 100 ml equaling 50 g/L.
So 50 g/L x 1mol/ 180 g = 0.278 moles/L. But we have to convert moles To mOsm so... .278 mol/L x 1000 mOsm / mol = 278 mOsm/L. The benchmark for isotonicity is 285 mOsm/ liter. If it is around there is isotonic. |
|
|
What is the osmolarity of 3% nacl solution? Is it ISO , hypo, or hyper osmotic?
|
The molecular weight of sodium chloride equals 58.5 g per mole . 3% nacl equals 3g / 100 ml equaling 30 g/L.
So 30 g/L x 1mol/ 58.5 g = 513 moles/L. But we still have to convert moles to mOsm . So nacl is 2 molecules so 1mmol =2 mOsm so... 513 mmol/L x 2 mOsm/mmol = 1026 mOsm/L. The benchmark for isotonicity is 285 mOsm/ liter. If it is around there is isotonic. This is clearly more so it's hypertonic. |
|
|
What happens to eCF volume and osmolarity as well as ICF volume and osmolarity if you add two liters of 3% sodium chloride to veins.
|
ECF rises more than 2 L because it pulls water out of the cell as well and overall osmolarity arises.
Intracellular fluid volume is going to fall because were pulling water out of the cells. ECF osmolarity increases as we put a lot of sodium and chloride i the ECF. ICF osmolarity also increases as we pull water away from the solutes |
|
|
What are the effects of adding 2 L water Iv on eCF volume and osmolarity as well as ICF volume and osmolarity?
|
Overall osmolarity falls due to delutional effect. Water can as well spread to both ICF and ECF and so both ECF and ICF volumes increase. It does not matter that it is hypotonic because water flows by osmosis therefore it will flow according to solute concentration.
|
|
|
During a high-protein low-carb diet, what still gets filtered into the urine and what follows this out of the body?
|
Amino acids ! gets filtered into your urine. water is going to follow the free amino acids and urea the byproduct of extra protein intake out of the body so we lose water weight.
|
|
|
What are the effects of adding 2 L 0.9 ns Iv on eCF volume and osmolarity as well as ICF volume and osmolarity?
|
0.9 normal saline is isotonic therefore osmolarity does not change. ECF volume rises because that's where we are putting the fluid but ICF volume stays the same.
|
|
|
What are the effects of adding 2 L 5% glucose (isotonic) Iv on eCF volume and osmolarity as well as ICF volume and osmolarity?
|
Initially osmolarity is unchanged but ECF volume rises due to the addition of fluid into the vein. But what happens is the cell over time metabolizes glucose which is going to in turn make that cell swell thereby increasing ICF. And so as the glucose metabolizes it vanishes which is like adding straight water to an Iv Which decreases overall osmolarity. So five percent glucose is only isotonic in the bag and for a short time in the vein.
|
|
|
Simple dehydration due to a water loss: (losing water from both ECf and ICF.)
Losing water from ECF causes what? what is effect on the osmolarity? |
Lost volume from the ECF causes a fluid shift from ICF to ECF. The osmolarity however it does not change.
|
|
|
If a person is dehydrated or if you electrolytes are added, then their osmolarity does what? Conversely if water is added then there osmolarity does what?
|
Dehydration or addition of electrolytes equals rise in osmolarity. Add water osmolarity goes down.
|
|
|
Hypernatremia is due to what two things? Is it a increase or decrease and sodium concentration?
|
It is an increase in sodium concentration. And is due to water loss or sodium excess
|
|
|
Hyponatremia is due to what two things? Is it a increase or decrease and sodium concentration?
|
It is a decrease in sodium concentration. And is due to water excess or sodium loss.
|
|
|
Normal plasma sodium is? Why is this important?
|
140 to 145 mmol per liter. About half of the osmolarity of our plasma is due to a Sodium
|
|
|
Hyponatremia causes cells to do what ? Hypernatremia causes cells to do what?
|
Hyponatremia causes cells to swell hypernatremia causes cells to shrink
|
|
|
Hyponatremia causes cells to do what ? Hypernatremia causes cells to do what? Where does this have a profound effect? What can rapid shrinking cause? What does rapid swelling cause? So if you are going to fix any of these problems how do you have to do it? Anytime we have k or na off we're thinking of a change in where?
|
Hyponatremia causes cells to swell hypernatremia causes cells to shrink. It has a profound effect in the brain! Rapid shrinking can cause tearing of the vessels or hemorrhage. Rapid swelling can cause herniation. You have to fix these problems slowly! We're thinking of a change in action potentials .
|
|
|
Hypernatremia with decreased vs increased ECf explain . What lab tests can diagnose this?
|
With decreased ECf fluid is lost so sodium is hyper concentrated - called hyperosmotic dehydration
With increased ECf a lot of sodium chloride is added - called hyperosmotic over hydration Diagnostic lab tests are hematocrit , plasma protein, urine volume |
|
|
Hyper natremia with increased ECF volume:
Define What happens to hematocrit , plasma proteins and urine volume what diseases can this happen with? |
Excess sodium chloride equals increased water over hydrating. This equals decreased hematocrit and plasma proteins and increased urine volume.
Primary aldosteronism- causes us to hold onto sodium and water by excess production of aldosterone through stimulation of the adrenal cortex. Cushing's disease- also stimulates the adrenal cortex but it results in an increase of both Cortisone and aldosterone |
|
|
Compare and contrast Cushing's disease to primary aldosteronism
|
They both result in retention of water and sodium causing over hydrated hypernateremia.
Primary aldosteronism- causes us to hold onto sodium and water by excess production of aldosterone through stimulation of the adrenal cortex. Cushing's disease- also stimulates the adrenal cortex but it results in an increase of both Cortisol and aldosterone. With the retention of sodium we will see the exact opposite with potassium . It will be very very low in the plasma. |
|
|
Hyponatremia- what two forms are possible?
|
Hyponatremia w increased or decreased ECF volume
|
|
|
What five things can cause hyponatremia with decreased extracellular fluid volume? What happens to hematocrit and plasma proteins during this state?
|
Diarrhea, vomiting, Addison's disease (decreased aldosterone), overuse of diuretics, sodium wasting renal diseases.
We would expect to see increased hematocrit as well as increased plasma proteins. |
|
|
What is the cause of hypo natremia with increased extracellular fluid volume? What happens to hematocrit and plasma proteins in this state?
|
The important one is circulatory failure i.e. congestive heart failure! But it can also happen from inappropriate ADH syndrome, a bronchogenic tumor, or tuberculous lung lesions. Hematocrit and plasma protein both decrease
|
|
|
Which of the following would lead to the most severe hyponatremia?
1. restriction of fluid intake 2. Excess ADH secretion 3. Excess aldosterone secretion 4. Administration of 2 L of 0.9 ns |
The answer is 2. Restriction of fluid intake as well as excess aldosterone secretion will equal high plasma sodium. Addition of 0.9 Ns won't make any changes either way
|
|
|
What is the difference between aldosterone and ADH?
|
ADH helps maintain water balance in the blood by making the distal tubule and collecting ducts more permeable to water.
Aldosterone helps maintain blood volume and pressure. It achieves this by making the distal tubule and collecting duct more permeable to sodium which creates more osmotic pressure making more water enter the blood. |
|
|
Four causes of intracellular edema:
|
Hyponatremia
Depression of tissue metabolic systems i.e. hypothyroidism- this is the most important one because it causes myxedema which is swelling in the face Inadequate tissue nutrition i.e. Ischemia or stroke Inflammation of tissues i.e. increased cell membrane permeability |
|
|
The two causes of extra cellular edema (increased interstitial fluid volume)
|
Increased capillary filtration and the failure of lymphatics to return interstitial fluid to circulation
|
|
|
Lymphatic failure equals what?
|
Edema!
|
|
|
What three safety factors are there against edema? How many millimeters of mercury safety factor does this total?
|
Low compliance of interstitium when the interstitial fluid pressure negative averages -3 mmHg lymphatic pull
Increased extracellular fluid equals increased lymphatic flow that averages 7 mmHg pull Wash down of interstitial protein and High lymph flow rates equals 7 mmHg look at it These three factors combined equal 17 mmHg safety factor against edema |
|
|
Hi lymph flow washes down what?
|
It washes down the interstitial proteins which creates a safety mechanism against edema
|
|
|
Hi capillary hydrostatic pressure can cause what? In what two ways can this happen?
|
It causes edema! This can happen by decreased arterial resistance (ie vasodilator drugs or autonomic insufficiency.) It can also happen by increased Venous pressure (I.e. congestive heart failure, high output heart failure (anemia ), venous obstruction, venous valve failure, cirrhosis)
|
|
|
Decreased plasma proteins equals low oncotic pressure. What does this cause? How does this condition come about?
|
This causes edema! This can happen from loss of proteins, burns, wounds, nephrosis, gastroenteropathy, failure to produce proteins, malnutrition, cirrhosis, and analbuminemia.
|
|
|
What are the four conditions that cause edema?
|
High capillary hydrostatic pressure, decreased plasma proteins, increased capillary permeability blockage of lymphatics
|
|
|
Increased capillary permeability causes what ? Which filtration coefficient is elevated? What six things Cause increased capillary permeability ?
|
It causes edema! Immune reactions such as histamine, toxins, burns, prolonged ischemia, vitamin deficiency (ie vitamin C, ) preeclampsia and eclampsia and pregnancy is the most important he said in class!
|
|
|
Blockage of lymphatics results in what? It is caused by what three things?
|
It results in edema! It can be caused by cancer surgery or infections
|
|
|
Hyper natremia with decreased extracellular fluid volume...
What is lost with this condition? What is the other name for this loss? What happens with hematocrit and the plasma proteins? What will we see as to the concentration of urine? What is diabetes insipidus and what is it caused by? |
The Water loss equals hyper osmotic dehydration. We will see a small volume of concentrated urine from the dehydration and excessive sweating. We will also see a large volume of dilute urine and the diabetes as in diabetes insipidus . Diabetes insipidus can happen from a lack of ADH which is called central diabetes insipidus or you can have nephrogenic DI
Increased hematocrit increased plasma proteins |

