![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
60 Cards in this Set
- Front
- Back
|
Respiration |
3 Separate Processes: 1. Ventilation (breathing) 2. Gas exchange between blood and lungs between blood and tissues 3. Oxygen utilization by tissues to make ATP
Ventilation and gas exchange in lungs = external respiration Oxygen utilization and gas exchange in tissues = internal respiration |
|
|
Respiratory Structures |
Air travels down the nasal cavity -> Pharynx -> Larynx -> Trachea -> Right and left primary bronchi -> Secondary bronchi -> Tertiary bronchi ->(more branching) -> Terminal bronchioles -> Respiratory zone (respiratory bronchioles) -> Terminal alveolar sacs |
|
|
Gas Exchange in Lungs |
Occurs via diffusion
O2concentration is higher in the lungs than in the blood, so O2 diffuses into blood.
CO2 concentration in the blood is higher than in the lungs, so CO2 diffuses out of blood. |
|
|
Alveoli |
Air sacs in the lungs where gas exchange occurs
300 million of them -Provide large surface area (760 square feet) to increase diffusion rate
|
|
|
Alveolar Cells: Type 1 & 2 |
Type I: 95−97% total surface area where gas exchange occurs
Type II: secrete pulmonary surfactantand reabsorb sodium and water, preventing fluid buildup
Macrophages: remove pathogens |
|
|
Atmospheric Pressure |
Can be measured using a barometer
At sea level, the atmospheric pressure is 760 mmHg. |
|
|
Lung Pressures |
Atmospheric pressure: pressure of air outside the body
Intrapulmonary pressure: pressure in the lungs
Intrapleural pressure: pressure within the intrapleuralspace (between parietal and visceral pleura |
|
|
Lung Pressures: Transpulmonary pressure: |
Pressure difference between intrapulmonary and intraplueral pressures -Keeps lungs adhering to thoracic wall and therefore functioning -Lungs are actually much smaller than thoracic cavity |
|
|
Boyle’s Law |
States that the pressure of a gas is inversely proportional to its volume -P = 1/V -An increase in lung volume during inspiration decreases intrapulmonary pressure to subatmospheric levels.Air goes in.
A decrease in lung volume during exhalation increases intrapulmonary pressure above atmospheric levels. -Air goes out. |
|
|
Ventilation |
Air moves from higher to lower pressure.
Pressure differences between the two ends of the conducting zone occur due to changing lung volumes.
Compliance, elasticity, and surface tension are important physical properties of the lungs. |
|
|
Pressure Differences When Breathing |
Inhalation: Intrapulmonary pressure is lower than atmospheric pressure.Pressure below that of the atmosphere is called subatmosphericor negative pressure
Exhalation: Intrapulmonary pressure is greater than atmospheric pressure. |
|
|
Breathing |
AKA: pulmonary ventilation -Inspiration: breathe in -Expiration: breathe out
Accomplished by changing thoracic cavity/ lung volume
Cyclic pressure changes in lung volume drive air in and out by utilizing principle of Boyle’s Law. |
|
|
Muscles Involved in Breathing |
Diaphragm: most important. -Contracts in inspiration -Relaxes in expiration
Inspiration: external intercostals
Expiration: internal intercostals, abs |
|
|
Physiological Problem |
Oxygen diffusion (and CO2) require a water interface for efficient transfer from lungs to tissue The behavior of water gets in the way of the regulation of lung volume and alveolar space…. -Surface tension |
|
|
What is surface tension? |
Contractive tendency of the surface of a liquid that allows it to resist an external force. -Caused by cohesion of similar molecules, and is responsible for many of the behaviors of liquids. -Hydrogen bonding
It is the reason why liquids form droplets and why insects can “walk on water” |
|
|
Law of Laplace |
Pressure is directly proportional to surface tension and inversely proportional to radius of alveolus. (smaller something becomes, more pressure excerpted by surface tension of water)
-Small alveoli would be at greater risk of collapse without surfactant. *read more in book, test* |
|
|
Surfactant |
-Secreted by type II alveolar cells -Consists of hydrophobic protein attached to a phospholipid -Reduces surface tension between water molecules -More concentrated in smaller alveoli -Prevents collapse, especially in smallest alveoli
(destroys the surface tension that water has) |
|
|
Dalton’s Law |
The total pressure of a gas mixture is equal to the sum of the pressures of each gas in it.
Partial pressure: the pressure of an individual gas; can be measured by multiplying the % of that gas by the total pressure O2 makes up 21% of the atmosphere, so partial pressure of O2= 760 X 21% = 160 mmHg. -Or PO2= 160 mmHg |
|
|
Total Pressure |
Nitrogen makes up 78% of the atmosphere, O2 21%, and CO2 1%. Pdry= PN2+ PO2+ PCO2= 760 mmHg
When air gets to our lungs, it is humid, so the calculation changes to: Pwet= PN2+ PO2+ PCO2+ PH2O= 760 mmHg |
|
|
Partial Pressure |
Addition of water vapor also takes away from the total atmospheric pressure when calculating partial pressure O2. |
|
|
Role of Gas Exchange |
In the alveoli, the percentage of oxygen decreases and CO2 increases, changing the partial pressure of each. |
|
|
Partial Pressure in Blood |
Alveoli and blood capillaries quickly reach equilibrium for O2and CO2.This helps maximize the amount of gas dissolved in fluid. -Henry’s Law predicts this.
|
|
|
Henry’s Law |
The amount of gas that can dissolve in liquid depends on: -Solubility of the gas in the liquid (constant) -Temperature of the fluid (more gas can dissolve in cold liquid); doesn’t change for blood -Partial pressure of the gases, the determining factor
The solubility of a gas in a liquid is directly proportional to the partial pressure of the gas above the liquid |
|
|
Partial Pressure of Gas in Blood |
If partial pressure oxygen in blood is more than 5 mmHg below that of lungs, gas exchange is impaired. |
|
|
Red Blood Cells (RBCs) |
-function as the oxygen carrier for cellular aerobic respiration. They possess a special oxygen carrying protein called hemoglobin (Hb). RBCs have no nucleus or mitochondria. Do not use the oxygen they carry. |
|
|
Oxygen Content of Blood |
In 100 ml of blood there is a total of 20ml of O2
Very little of O2 is dissolved (0.3 ml/100 ml)1.5% Need at least 5 ml of O2just to stay alive
-Most 02in blood is bound to Hbinside RBCs as oxyhemoglobin -Hb greatly increases 02 carrying capacity of blood -Does not actually count to the partial pressure because it is bound to Hb |
|
|
Hemoglobin |
Most of the oxygen in blood is bound to hemoglobin. -4 polypeptide globinsand 4 iron-containing hemes----(Why our blood is red)
-Each hemoglobin can carry 4 molecules O2. -248 million hemoglobin/RBC |
|
|
Forms of Hemoglobin (ppg 559,560) |
Oxyhemoglobin/reduced hemoglobin Carbaminohemoglobin Methemoglobin Carboxyhemoglobin |
|
|
% Oxyhemoglobin Saturation |
% oxyhemoglobinto total hemoglobin
Measured to assess how well lungs have oxygenated the blood
Normal is 97%
Measured with a pulse oximeteror blood–gas machine |
|
|
Hemoglobin Concentration |
Oxygen-carrying capacity of blood is measured by its hemoglobin concentration. -Anemia: below-normal hemoglobin levels, normal PO2 but total O2low in blood -Polycythemia: above-normal hemoglobin levels; may occur due to high altitudes (rare)
Erythropoietin made in the kidneys stimulates hemoglobin/RBC production when O2levels are low. |
|
|
Loading and Unloading of hemoglobin |
Loading: when hemoglobin binds to oxygen in the lungs Unloading: when oxyhemoglobin drops off oxygen in the tissues deoxyhemoglobin+ O2 <-----> oxyhemoglobin (direction depends on particle pressure)
Direction of reaction depends on PO2of the environment and affinity for O2. -High PO2 favors loading |
|
|
Oxygen Unloading |
Systemic arteries have a PO2 of 100 mmHg. -This makes enough oxygen binding to get 97% oxyhemoglobin. -20 ml O2/100 ml blood
Systemic veins have a PO2 of 40 mmHg.This makes enough oxygen binding to get 75% oxyhemoglobin. -15.5 ml O2/100 ml blood •22% oxygen is unloaded in tissues
Why is this a good thing? why is it hanging on to 75%... reserves (body wants to be able to regulate & reserve)(basic strategy for robustness) |
|
|
PO2 and % Oxyhemoglobin |
S-shaped or Sigmoidal curve In steep part of curve, small changes in P02cause big changes in % saturation or unloading
table 16.7, see graph on slide 41 |
|
|
Physiological Problem |
If hemoglobin is so great at picking up oxygen from the lungs so that it can be delivered to the tissues then how does it finally “let go” of the oxygen once it arrives at the tissues? -the oxygen dissociation curve -The Bohr effect is what allows Hb to effectively unload oxygen where it is needed most.
|
|
|
Oxygen Dissociation Curve |
Oxygen remaining in veins serves as an oxygen reserve. Oxygen unloading during exercise is even greater: 22% at rest 39% light exercise 80% heavy exercise
Why would this happen?
|
|
|
Physiological Regulation of Oxyhemoglobin Dissociation Curve |
Conditions that shift the curve to the left would cause more affinity and less unloading
Conditions that shift the curve to the right would cause low affinity and more unloading Ex: ↑ CO2 ↑ [H+] Bohr effect ↑ Temperature ↑ 2,3-DPG (chemical) Fever |
|
|
2,3-DPG |
2,3-Diphosphoglyceric acid (2,3-DPG): Allosteric effector. Causes more oxygen to be released from Hb. High concentrations seen in people at high altitude and anemic people.
-(product of gylcolsis) |
|
|
Effect of pH and Temperature on Oxygen Transport |
pH and temperature change the affinity of hemoglobin for O2. -This ensures that muscles get more O2 when exercising. -Affinity decreases at lower pH and increases at higher pH = Bohr effect. -More unloading occurs at lower pH. -Increased metabolism = more CO2= lower pH
lower pH, increasing temp. |
|
|
Factors That Affect O2 and Hb affinity (HEP) |
table 16.9
-the oxygen dissociation curve
|
|
|
Fetal Hemoglobin |
Adult hemoglobin (hemoglobin A) can bind to 2,3-DPG, but fetal hemoglobin (hemoglobin F) cannot.
-Fetal hemoglobin therefore has a higher affinity for O2 than the mother, so oxygen is transferred to the fetus. |
|
|
Inherited Hemoglobin Defects: Sickle-cell anemia |
Sickle-cell anemia: found in 8−11% of African Americans -The affected person has hemoglobin S with a single amino acid difference. -Deoxygenated hemoglobin S polymerizes into long fibers, creating a sickle-shaped RBC. -This hinders flexibility and the ability to pass through small vessels.
Gene is 438 base-pairs long (146 amino acids). One error leads to a glutamate turning into a valine. |
|
|
Myoglobin |
Red pigment found in skeletal and cardiac muscles Similar to hemoglobin, but with 1 heme, so it can only carry 1 oxygen molecule -Higher affinity to oxygen; oxygen is only released when PO2is very low -Stores oxygen and serves as go-between in transferring oxygen from blood to mitochondria |
|
|
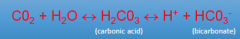
Carbon Dioxide in the Blood (Equation) (HEP) |
|
|
|
Carbon Dioxide in the Blood |
Carried in the blood in three forms: 1. Dissolved in plasma (10%) 2. As carbaminohemoglobin attached to an amino acid in hemoglobin (20%) 3.As bicarbonate ions (70%!) |
|
|
Chloride Shift –A clever way to regulate CO2 |
Carbon dioxide is released from tissues due to oxidative respiration •CO2 needs to be removed from tissues due to disruptive nature of carbon dioxide (Acidifies blood)
|
|
|
Chloride Shift |
CO2 diffuses out of cell: -Some stays in plasma -Some binds to Hb(O2 now gone) -Lots in RBC, where there is the enzyme carbonic anhydrase C02+ H2O →H2C03 -H2C03 spontaneously turns to H++ HC03- -HC03-gradient causes it to move out of cell, in exchange Cl-ions move in -This causes CO2→H++HCO3- reaction to keep going -Important for picking up the rest of the CO2 in tissues and for making more bicarbonate for blood buffering |
|
|
Chloride Shift (process) |
1. High H+& HC03-levels in RBCs 2. H+is buffered by proteins 3. HC03-diffuses down concentration & charge gradient into plasma and in exchange Cl-ions move inotherwise RBC to become too positively (+) charged 4. So Cl-moves into RBC (chloride shift) to balance the charge 5. HCO3-acts as a major buffer in plasma and reaction continues to favor the loading of RBCs with CO2 |
|
|
Reverse Chloride Shift |
getting rid of all that nasty CO2
C02+ H2O ←H2C03←H++ HC03- |
|
|
Acid-Base Balance in Blood |
Blood pH is maintained within narrow pH range by lungs & kidneys (normal = 7.4)
Most important buffer in blood is bicarbonate H20 + C02 ↔H2C03 ↔H++ HC03- Excess H+ is buffered by HC03-
Kidney's role is to excrete excess H+ into urine |
|
|
Ventilation and Acid-Base Balance (buffer!) |
The normal pH of blood is between 7.35 and 7.45. A major buffer which regulates this pH is HCO3-. This bicarbonate ion traps H+if the pH gets too low or releases H+if the pH is too high, thus buffering the system.
If there is a decrease in [H+] (or pH increase), then H2 CO3 ➔ H++ HCO3- If there is an increase in [H+] (a pH decrease), then HCO3- + H+ ➔ H2 CO3 the bicarbonate ion thus functions as a major buffer in blood |
|
|
Acid-Base Balance in Blood (2 major acids in the body:) |
2 major classes of acids in body: 1. A volatile acid can be converted to a gas Ex: C02 in bicarbonate buffer system can be breathed out (H20 + C02 ↔H2C03 ↔H++ HC03-) All other acids are nonvolatile & cannot leave blood Ex: lactic acid, fatty acids, ketone bodies -Bicarbonate buffering system keeps pH in check |
|
|
Blood pH: Acidosis |
Acidosis: when blood pH falls below 7.35
-Respiratory acidosis: hypoventilation
-Metabolic acidosis: excessive production of acids, loss of bicarbonate (diarrhea) |
|
|
Blood pH: Alkalosis |
Alkalosis: when blood pH rises above 7.45 -Respiratory alkalosis: hyperventilation -Metabolic alkalosis: inadequate production of acids or overproduction of bicarbonates, loss of digestive acids from vomiting |
|
|
Hypoventilation:
Hyperventilation:
|
Ventilation controls the respiratory component of acid-base balance.
Hypoventilation: Ventilation is insufficient to “blow off” CO2. PCO2 is high, carbonic acid is high, and respiratory acidosis occurs.
Hyperventilation: Rate of ventilation is faster than CO2 production. Less carbonic acid forms, PCO2 is low, and respiratory alkalosis occurs. |
|
|
acidosis alkalosis and ventilation |
A person with metabolic acidosis will hyperventilate.
A person with metabolic alkalosis will hypoventilate. |
|
|
Brain Stem Respiratory Centers |
Automatic breathing is generated by a rhythmicity center in medulla oblongata
Consists of inspiratory neurons that drive inspiration & expiratory neurons that inhibit inspiratory neurons -Their activity varies in a reciprocal way & may be due to pacemaker neurons |
|
|
Activities of medullary rhythmicity center is influenced by: |
Pons -Apneustic center: promotes inspiration by stimulating inspiratory neurons in medulla -Pneumotaxic center: antagonizes apneusticcenter, inhibiting inspiration |
|
|
Chemoreceptors |
Automatic control of breathing is influenced by feedback from chemoreceptors, which monitor pH of fluids in the brain and pH, PCO2and PO2of the blood. -Central chemoreceptors in medulla -Peripheral chemoreceptors in carotid and aorta arteries
Aortic body sends feedback to medulla along vagus nerve.
Carotid body sends feedback to medulla along glossopharyngeal nerve. |
|
|
Effects of pH and PCO2 on Ventilation |
When ventilation is inadequate, CO2levels rise and pH falls. (carbon dioxide + water = carbonic acid)
In hyperventilation, CO2 levels fall and pH rises. •Oxygen levels do not change as rapidly because of oxygen reserves in hemoglobin, so O2 levels are not a good index for control of breathing. |
|
|
Effects of PCO2 on Ventilation |
Ventilation is controlled to maintain constant levels of CO2 in the blood. Oxygen levels naturally follow. |

