![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
22 Cards in this Set
- Front
- Back
|
Dysplasia of cervix |
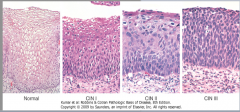
Disordered epithelial growth, begins @ basal layer of squamocolumnar junction (transition zone) and extends downward. Classified by CIN - CIN1,2,3 are all different grades of dysplasia and carcinoma in situ is SEVERE dysplasia |
|
|
part of cervix that is ENTIRELY STRATIFIED SQUAMOUS EPI |
ectocervix |
|
|
part of cervix that is simple columnar |
endocervix |
|
|
junction between uterus and cervical canal |
internal os |
|
|
junction between cervix and vagina |
external os - change from simple columnar to strat squam epithelium |
|
|
koilocytic change + disordered cellular maturation + nuclear atypia + increased mitotic activity within the cervical epithelium |
cervical intraepithelial neoplasia (CIN) |
|
|
<1/3 thickness of epithelium of cervix with dysplasia |
CIN1 |
|
|
>1/3 but <2/3 thickness of epithelium of cervix with dysplasia |
CIN2 |
|
|
>2/3 but slightly < full thickness of epithelium of cervix with dysplasia |
CIN3 |
|
|
ENTIRE THICKNESS OF EPITHELIUM INVOLVES with SEVERE DYSPLASIA |
carcinoma in situ CIN1 --> CIN2 --> CIN3 --> extensive dysplasia --> CIS --> invasive carcinoma...progression is NOT inevitable but occurs in this order |
|
|
With what serotypes of HPV are CIN associated? |
HPV 16,18 |
|
|
What do E6 and E7 proteins do? |
E6 - inhibits P53 E7 - inhibits Rb |
|
|
Symptoms of CIN? |
Usually asymptomatic. MAY present as abnormal vaginal bleeding (often postcoital) |
|
|
Risk factors for CIN |
Multiple sexual partners = #1 smoking, early sexual intercourse, HIV infection |
|
|
Describe cervical koilocytes? |
wrinkled, "raisinoid" nuclei which have clearing of a perinuclear halo |
|
|
INVASIVE CARCINOMA of the cervix: - What type of cancer most likely? - What is the purpose of pap smear? - Complications? |
often SCC (80%...but 15% is adenocarcinoma) . Pap smear can catch cervical dysplasia BEFORE it progresses to invasive carcinoma. LATERAL INVASION --> can block ureters, causing renal failure (hydronephrosis + post-renal failure) |
|
|
What is HPV? |
A sexually transmitted DNA virus that effects the LOWER GENITAL TRACT, esp. the cervix in the TRANSFORMATION ZONE. The infection is eradicated by ACUTE INFLAMMATION, however persistent infection leads to INCREASED RISK FOR CERVICAL DYSPLASIA (CIN). The risk of CIN however depends on SEROTYPE: high risk = 16,18, 31, and 33 as these produce E6 AND E7 proteins |
|
|
Where do you draw cells for a pap smear. What would abnormal cells look like. What confirms the diagnosis of CIN? |
From the transformation zone (squamocolumnar junction i.e. external os). Abnormal cells will have hyper chromatic nuclei with high N/C ratio. Confirmatory diagnosis requires culposcopy. |
|
|
What major serotypes does the HPV vaccine protect against? |
HPV 6, 11, 16, 18 |
|
|
Describe the development of the squamocolumnar junction? |
At birth - the squamocolumnar junction is similar to where it is as an adult - IE at the ectocervix. As a young adult, the columnar epithelium of the dnocervix grows out into the ectocervix, creating an "extropion" with exposed columnar epi. In an adult, the ectocervix is "restored" as the columnar epithelium undergoes PHYSIOLOGICAL (normal) metaplasia to become squamous epithelium ("transformation zone"). This restores the normal position of the squamocolumnar junction. |
|
|
What is LSIL? HSIL? Which is more likely to occur? Which is more likely to progress to carcinoma? |
LSIL = low grade squamous intraepithelial lesion. It includes CIN1 only. HSIL = high grade squamous intraepithelial lesion. It includes CIN2, CIN3, and carcinoma in situ (CIN3). LSIL is 10x more likely. HSIL is more likely to progress to carcinoma. 10% persist to carcinoma within 2-10 yrs |
|
|
different CINs |

