![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
51 Cards in this Set
- Front
- Back
- 3rd side (hint)
|
What is cervical intraepithelial neoplasia (CIN)? |
is the potentially premalignant transformation and abnormal growth (dysplasia) of squamous cells on the surface of the cervix. CIN is not cancer, and is usually curable. |
|
|
|
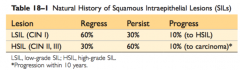
What is CIN I, CIN II, and CIN III? |
|
|
|
|
Carcinoma in situ? |
group of abnormal cells, not necessarily cancerous |
|
|
|
koilocytosis? |
a squamous epithelial cell that has undergone a number of structural changes, which occur as a result of HPV infection aka LSIL |
|
|
|
what is LSIL |
low squamous intraepithelial lesion |
|
|
|
what is HSIL |
high squamous intraepithelial lesion |
|
|
|
what is the transformation zone in the cervix |
this zone consists of metaplastic squamous cells, found between the new squamocolumnar junction (SCJ) and the original SCJ |
|
|
|
what are the risk factors assoc with cervical cancer? |
- HPV infections - cigarette smoking -immunodeficiency - no screening |
|
|
|
What is HPV? |
Human Papilloma Virus |
|
|
|
What does HPV do? |
- >200 types; 40 types affect genital tract - infects epithelial cells of the anogenital tract - also assoc with anal (85%), perianal, vulvlar and penile carcinoma (50%), oropharyngeal cancer (30%) |
|
|
|
what are the low risk types of HPV and what are there outcomes? |
6 and 11 (+ 42, 44 etc)
-genital warts- rarely progress to malignancy |
|
|
|
what are the high risk types of HPV and what are there outcomes? |
16 and 18 (+31,45 etc)
-pre-invasive lesions and invasive carcinomas |
|
|
|
Natural history HPV infection? |
-sexually transmitted, assoc with early sexual activity; multiple sexual partners - infection is quite common - mostly clear up within 9-15 months IF NOT - CIN/SIL - persistant infection with high risk HPV is necessary for development and maintenance of CIN III |
|
|
|
What if E6? |
Protein binds to the protein product of p53 tumour suppressor gene and inactivated it
CELLS W/ MUTATIONS AVOID APOPTOSIS |
|
|
|
What does E6 do? |
binds and inactivates to p53 tumour suppressor gene
CELLS W/ MUTATIONS AVOID APOPTOSIS |
|
|
|
What Does E7 do? |
binds and inactivates to Rb tumour suppressor gene
CELLS PROLIFERATE MORE RAPIDLY |
|
|
|
what are E6 and E7 genes integrated into in carcinomas? |
DNA |
|
|
|
What is E6 and E7? |
Oncoproteins |
|
|
|
What is E6 and E7? |
Oncoproteins |
|
|
|
What is p53? |
Tumour suppressor gene
Transcription factor |
|
|
|
What is Rb gene? |
Tumour suppressor gene
In cell cycle, Rb can leave temporarily/permanently and complete mitosis |
|
|
|
What is E6 and E7? |
Oncoproteins |
|
|
|
What is p53? |
Tumour suppressor gene
Transcription factor |
|
|
|
What is Rb gene? |
Tumour suppressor gene
In cell cycle, Rb can leave temporarily/permanently and complete mitosis |
|
|
|
HPV infects __________ squamous cells in the ________________ zone |
Immature
Transformation |
|
|
|
HPV infects __________ squamous cells and _______ cells in the ________________ zone |
Immature
Basal
Transformation |
|
|
|
Histology: Cytology = __________:____________ |
CIN - cervical intrepid helical neoplasia
SIL - squamous intraepithelial lesion |
|
|
|
Diagnostic technique used to look at cervix |
colposcopy |
Looks likes a microscope |
|
|
Clinical manifestation of cervical cancer |
-vaginal discharge, abnormal bleeding - painful coitus and post coitus bleeding -loss of appetite, weight loss, fatigue -pelvic, back or leg pain, urinary/faecal incontinence |
|
|
|
What is coitus? |
Sexual intercourse |
|
|
|
Where can cervical cancer spread? |
Local invasion - peritoneum - bladder - ureters- renal failure (most common cause of death) - rectum - vagina |
|
|
|
Treatment options for cervical cancer? |
- wire loop excision ( local anaesthetic) - cone biopsy (general anaesthetic) - laser - diathermy ( removal of cells using heat- general anaesthetic required) |
|
|
|
Cervical cancer prognosis? |
5 yr survival
Stage 1: 95% Stage 2: 75% Stage 3: <50% Stage 4: death due to local extension of tumour rather than metastatic disease |
|
|
|
HPV infects __________ squamous cells and _______ cells in the ________________ zone |
Immature
Basal
Transformation |
|
|
|
Histology: Cytology = __________:____________ |
CIN - cervical intrepid helical neoplasia
SIL - squamous intraepithelial lesion |
|
|
|
Diagnostic technique used to look at cervix |
colposcopy |
Looks likes a microscope |
|
|
Clinical manifestation of cervical cancer |
-vaginal discharge, abnormal bleeding - painful coitus and post coitus bleeding -loss of appetite, weight loss, fatigue -pelvic, back or leg pain, urinary/faecal incontinence |
|
|
|
What is coitus? |
Sexual intercourse |
|
|
|
Where can cervical cancer spread? |
Local invasion - peritoneum - bladder - ureters- renal failure (most common cause of death) - rectum - vagina |
|
|
|
Treatment options for cervical cancer? |
- wire loop excision ( local anaesthetic) - cone biopsy (general anaesthetic) - laser - diathermy ( removal of cells using heat- general anaesthetic required) |
|
|
|
Cervical cancer prognosis? |
5 yr survival
Stage 1: 95% Stage 2: 75% Stage 3: <50% Stage 4: death due to local extension of tumour rather than metastatic disease |
|
|
|
How can you prevent HPV? |
Gardasil - effect in HPV 6,11,16,18 - provides protection against 70% of HPV related cervical carcinoma -cost effective intervention for general warts and anal cancer for men (9-26yo) |
Vaccination: G________l |
|
|
HPV infects __________ squamous cells and _______ cells in the ________________ zone |
Immature
Basal
Transformation |
|
|
|
Histology: Cytology = __________:____________ |
CIN - cervical intrepid helical neoplasia
SIL - squamous intraepithelial lesion |
|
|
|
Diagnostic technique used to look at cervix |
colposcopy |
Looks likes a microscope |
|
|
Clinical manifestation of cervical cancer |
-vaginal discharge, abnormal bleeding - painful coitus and post coitus bleeding -loss of appetite, weight loss, fatigue -pelvic, back or leg pain, urinary/faecal incontinence |
|
|
|
What is coitus? |
Sexual intercourse |
|
|
|
Where can cervical cancer spread? |
Local invasion - peritoneum - bladder - ureters- renal failure (most common cause of death) - rectum - vagina |
|
|
|
Treatment options for cervical cancer? |
- wire loop excision ( local anaesthetic) - cone biopsy (general anaesthetic) - laser - diathermy ( removal of cells using heat- general anaesthetic required) |
|
|
|
Cervical cancer prognosis? |
5 yr survival
Stage 1: 95% Stage 2: 75% Stage 3: <50% Stage 4: death due to local extension of tumour rather than metastatic disease |
|
|
|
How can you prevent HPV? |
Gardasil - effect in HPV 6,11,16,18 - provides protection against 70% of HPV related cervical carcinoma -cost effective intervention for general warts and anal cancer for men (9-26yo) |
Vaccination: G________l |

