![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
314 Cards in this Set
- Front
- Back
|
Branches of the ECA include all of the following EXCEPT:
A) Occiptal
B) Basilar
C) Facial
D) Ascending pharyngeal |
B) Basilar |
|
|
The vessel that connects the left and right ACA's is the:
A) MCA
B) Basilar artery
C) Anterior communicating artery
D) Right and left posterior communicating arteries |
A) Anterior communicating artery |
|
|
All of the following are part of the Circle of Willis (COW) EXCEPT:
A) Anterior communicating artery
B) PCA
C) Anterior choroidal arteries
D) Posterior communicating arteries |
C) Anterior choroidal arteries??? |
|
|
One cause of right hemispheric infarction is:
A) Stenosis of the R ECA
B) Occlusion of the R ICA
C) Stenosis of the L ECA
D) Occlusion of the L ICA |
??? |
|
|
In a carotid duplex exam, all of the following are common causes for underestimating the degree of stenosis EXCEPT:
A) Improper placement of the sample volume
B) Low-level echoes from fresh thrombus
C) Tangent lesions
D) FMD |
D) FMD |
|
|
The following artery is NOT routinely evaluated in a TCD exam:
A) MCA
B) ACA
C) PCA
D) Posterior communicating |
D) Posterior communicating |
|
|
Angiography reveals a stenotic R ICA w/a residual lumen of 3mm. If the normal lumen is 9mm the diameter reduction (DR) is:
A) 33%
B) 50%
C) 67%
D) 78% |
D) 67 ??? |
|
|
In a TCD exam the normal direction of blood flow in the MCA is:
A) Bidirectional
B) Antegrade
C) Retrograde
D) Antegrade in dominant hemisphere, retrograde in non-dominant hemisphere |
B) Antegrade |
|
|
After passing into the skull, the ICA gives off the caroticotympanic branch and then its first major branch the ____________ at the ________, a significant curve of the ____________. |
- ophthalmic artery - carotid siphon - distal ICA |
|
|
The ICA gives off the ________ and ______ before it finally divides into the MCA and ACA.
Majority of blood flow in the CCA (70-80%) flows into the ____ to satisfy the high metabolic demands of the brain. |
- anterior choroidal - posterior communicating arteries
- ICA |
|
|
T or F:
The ECA distributes blood to the anterior brain, the eyes, the forehead, and the nose, w/the brain being a very high-resistance vascular bed. |
FALSE:
The ICA distributes blood to the anterior brain, the eyes, the forehead, and the nose, w/the brain being a very LOW-resistance vascular bed. |
|
|
T or F:
The ICA and ECA both originate from the CCA and give off branches extrancranially |
FALSE:
Both originate from CCA. ICA travels into the base of the skull BEFORE giving off any branches |
|
|
The ECA gives off ___ branches which supply blood to the neck, face and scalp, all of which are __________. |
- 8 - high-resistance vascular beds |
|
|
8 branches of ECA
S______ A_____ L_____ F_____ O____ P____ S_____ M____
|
- Superior thyroid artery - Ascending pharyngeal - Lingual artery - Facial artery - Occipital artery - Posterior auricular artery - Superficial temporal artery - Maxillary artery |
|
|
What is the first branch of the ECA?
which is most commonly seen on carotid duplex exams? |
- superior thyroid artery usually-- sometimes it originates from the distal CCA.
- superior thyroid artery |
|
|
The presence of the __________ is one method to determine if the insonated vessel is the ECA because the ICA normally has no branches in the neck.
Would retrograde flow in this artery be considered normal or abnormal? |
- superior thyroid artery
- Normal: Usually retrograde compared to the CCA because of the course of the superior thyroid artery |
|
|
Right & left vertebrals:
Originate from the ___________
Are _______ in size with the ___ usually smaller than the _________.
Unite to form the _____ after they ___________ thru the ___________. |
- subclavian arteries
- asymmetrical - right > left
- basilar artery - enter the skull - magnum foramen |
|
|
The Basilar artery:
Is formed by the confluence of the __________.
Divides into the ____________ to form part of the ___________.
Supplies blood to the _____________. |
- right & left verts
- Posterior Cerebral Arteries - Circle of Willis
- posterior structures of the cranial cavity |
|
|
Circle of Willis (COW):
An _________________ channel, approximately the size of a _________, which lies at the __________, connecting the ___________ & _______ systems.
|
- intracranial communication - 50 cent piece - base of the brain - anterior - posterior circulatory |
|
|
When the COW is complete (some are not), it provides an important ___________ that maintains blood flow to the brain in cases of __________ or ____. |
- collateral pathway - stenosis - occlusion |
|
|
The COW is a __________ arrangement of the distal ICA, anterior cerebral and posterior cerebral arteries. |
- hexagonal cow pic |
|
|
cow pic |
cow pic |
|
|
cow pic |
can be number of variations to this structure including vessel size and congenital anomalies |
|
|
T or F:
Although the distal ICA, anterior cerebral and posterior cerebral arteries are joined together by the anterior & posterior communicating arteries, blood flow through these communicators is frequently evident |
FALSE:
USUALLY EVIDENT ONLY when they serve as significant collateral channels secondary to a hemodynamically significant lesion of the extracranial carotid circulation. |
|
|
Anterior circulation is the _______________
Posterior circulation is the ________________ |
ANT: ICA & ECA
POST: R & L vertebrals, basilar artery, (circle of willis?) |
|
|
Periorbital circulation includes the ophthalmic artery and its 3 branches _____________ ____________ & _____________.
|
- supraorbital artery - frontal artery - nasal artery
|
|
|
The _____ arises from the ophthalmic artery and exits the orbit medially to supply the mid-forehead. It joins the ECA via branches of the superficial temporal artery.
The ____________ arises from the ophthalmic artery and travels anteriorly and superiorly to the globe. It joins the ECA via branches of the superficial temporal artery. |
- frontal artery
- supraorbital artery |
|
|
The nasal artery branches from the ____________ to supply the nose. It becomes the ________________ along the lateral border of the nose and joins the ECA via the ________________. |
- frontal artery
- angular artery
- facial artery |
|
|
What is the largest intraarterial connection?
|
- The Circle of Willis |
|
|
Intracranial-extracranial anastomoses:
ICA-ECA connections via the ____________, _______________, the meningohypophyseal branches, and the carticotympanic branch |
- ophthalmic & orbital arteries |
|
|
Intracranial-extracranial anastomoses:
The ____________ branch of the ECA w/the Atlantic branch of the ____________.
The ____________ across the midline. |
- occipital - vertebral artery
- ECA's |
|
|
Intracranial-extracranial anastomoses:
The deep cervical and ascending cervical branches of the ________ to the branches of the lower _____________, the Atlantic branch of the upper ___________, and the ____________ of the ECA. |
- subclavian
- vertebral artery
- vertebral
- occipital branch |
|
|
Small intraarterial communications:
Intricate network of transdural anastomoses across the subdural space from the _______________ to the arteries on the ____________.
Leptomeningeal collaterals form the meningeal border-zone network that connects the terminal ___________ of the _________ arteries. |
- dural arteries - surface of the brain
- cortical branches - cerebral |
|
|
The function of the artery is to carry blood ____ the heart, transport _______, nutrients, and other essential substances to tissues. Help to regulate blood flow by _____________ and ____________. |
- away from
- gases
- contracting - relaxing |
|
|
Which layer has a thin layer of fibrous connective tissue and some smooth muscle fibers and contains the 'vasa vasorum' ?
Which layer has a single layer of endothelial cells w/a base membrane and connective tissue?
Which layer consists of smooth muscles and collagenous fiber that is usually arranged in a circular fashion? |
- tunica adventitia
- tunica intima
- tunica media |
|
|
_____________ is known as the "vessels of vessels" and supply blood to the __________ of the _________. |
- vasa vasorum - walls - larger arteries |
|
|
The vasa vasorum transports ___________ and nutrients as well as remove _____________. |
- oxygen
- waste products |
|
|
T or F:
The vasa vasorum can also function as a collateral pathway to maintain patency of the ICA in the presence of a focal occlusion |
TRUE |
|
|
Bernouilli: total fluid energy along a streamline of fluid flow is _______ and that velocity energy and pressure energy are _____________.
Higher velocity = ____________ pressure Lower velocity = _____________pressure
|
- constant - inversely proportional
- lower - higher |
|
|
Pressure gradients develop as a result of changes in the ____________ and ___________ of the vessel whether or not there is intraluminal disease.
Pressure gradients also known as areas of flow separation are easily observed in systole as ________. Regions of ______________ are evident in diastole. |
- geometry - direction
- reversed flow - stagnation |
|
|
Pousille's:
Flow is directly proportional to ____________ and _____________.
Flow is inversely proportional to the ___________ and ___________ which are elements of ____________. |
- a pressure gradient - the size of the vessel
- viscosity of the blood - length of the vessel - resistance |
|
|
Pousille's:
Law of conservation of mass: Volume flow / ________. Considering that volume flow is ___________, radius is _______ to the velocity.
Compensatory mechanisms; increase in velocity work to ____________ across a lesion |
cross sectional area
- constant - inversely proportional
- equalize flow |
|
|
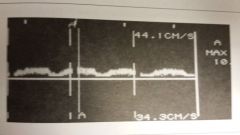
Laminar flow in normal artery is evident by ______ band of frequencies during systole leaving a ____________ beneath the envelope. |
- narrow - window |
|
|
Slight turbulence from a mild stenosis broadens the ______________. |
-frequency band |
|
|
Accelerated, turbulent flow caused by tight stenosis, note loss of ___________. |
- frequency window |
|
|
The blood must change direction as the flow steam ________ at the stenosis and ____________ as it exits the stenosis.
The resulting ______ currents, turbulence, and vortices produced by changes in the flow steam cause a ___________ loss through ____________. |
- narrows - enlarges
- energy - inertia |
|
|
Velocity increases through a stenosis because _______________ and ___________ are ______________.
This acceleration increases _____________. |
- velocity and area are inversely proportional.
- energy losses |
|
|
Acceleration is reflected as _____________ or ___________.
Turbulence is detected by _________ which is a wide range of very low to very high ____________.
This results in the loss of the _________ or ________. |
- increased frequency - increased velocity measurement
- spectral broadening - frequency shifts
- frequency - spectral window |
|
|
A VBI (vertebrobasilar insufficiency), CVA , TIA and RINF are symptoms of _________ ____________. |
- Transient ischemia |
|
|
TIA stands for ____________ ____________ ________. It is a fleeting neurologic dysfunction without _____________ ___________.
Symptoms usually last from a few _____________ to a few ____________ but never more than ___________. |
- Transient ischemic attack - lasting effects
- minutes - hours - 24 hours |
|
|
Depending on the cerebral territory involved, sxs may include ____________ or ___________ dysfunction of an arm or leg, speech ___________, or ______ ___________ disturbances.
The etiology of a TIA is usually ________ and the ________ or ________ is most often the source of the _______. |
- sensory or motor - impairment - monocular visual
- embolic - heart - carotid artery - emboli |
|
|
RIND stands for _____________
Which usually lasts longer a TIA or a RIND?
The deficit it creates _____________. Brain tissue is damaged but _____________. |
- Reversible Ischemic Neurologic Deficit
- A RIND - resolves in time - recovers completely |
|
|
VBI stands for _____________________
Usually causes __________ sxs of visual __________ or paresthesia and complaints of _____, ataxia, and _________ __________. |
- Vertebrobasilar insufficiency
- blurring - vertigo - drop attacks |
|
|
CVA stands for ___________, also known as a _____. This produces a ________ neurologic deficit.
What are the 3 classifications of strokes?
Which are considered unstable? |
- Cerebrovascular accident - stroke - permanent
1. Acute 2. Stroke in evolution 3. Completed stroke
- acute strokes and stroke in evolution are unstable |
|
|
Acute: sxs of ___________ ________, considered ____________.
Stroke in evolution: sxs _____________, considered __________.
Completed stroke: no _________ or ______ of sxs, considered __________. |
- sudden onset - unstable
- come and go - unstable
- progression - resolution - stable |
|
|
T or F:
The chronic complications of diabetes mellitus are primarily vascular |
TRUE:
Most common form of diabetes-- is a chronic systemic disease characterized by disorders of the metabolism of insulin, carbs, fat and protein |
|
|
HTN may be a causative factor in the development of _______ or it may enhance the development of the ___________ process.
It almost certainly helps to precipitate clinical events associated w/it such as ______ and ____. |
- atherosclerosis - atherosclerotic
- embolization - aneurysms |
|
|
Smoking is associated w/the __________ of the _______ of the blood vessels.
____________ because _______ are insoluble in water, an excessive amt of plasma _____ is closely associated w/the development of atherosclerosis.
|
- irriation - endothelial lining
- hyperlipidemia - lipids - lipids |
|
|
The 2 most common mechanisms of cerebrovascular insufficiency are ______ & ______.
|
- ischemia - hemorrhage |
|
|
The 3 leading causes of ischemic are: ___________ pathology, _______ pathology and ________ strokes.
|
- atherothrombotic - cardiogenic - lacunar |
|
|
T or F:
Atherothrombotic pathologies include alterations in perfusion primary to an atheromatous plaque, resulting in stenosis, occlusion, or a thromboembolic event. |
FALSE:
Atherothrombotic pathologies include alterations in perfusion SECONDARY to an atheromatous plaque, resulting in stenosis, occlusion, or a thromboembolic event. |
|
|
The cardiogenic pathologies usually responsible for CV ischemia are altered _______ and most often _______.
A lacunar infarction is a small circumscribed loss of _________ caused by __________ of one of the _____________ in the brain. |
- cardiac function - embolism
- brain tissue - occlusion - small penetrating arteries |
|
|
T or F:
The leading causes of hemorrhage are atherothrombotic pathologies, cardiogenic pathologies and lacunar strokes |
FALSE:
Those are the leading causes of ischemic |
|
|
Hemorrhage may be the result of _________, ruptured __________, or ___________ ex: subarachnoid hemorrhage |
- HTN
- aneurysm
- trauma |
|
|
Stenosis: Atherosclerosis is a common pathological condition in which the arteries ______, harden, and lose their ____________, creating a __________ that can reduce __________ blood flow and adversely affect ___________ _______. |
- thicken - elasticity - narrowing - distal - brain perfusion |
|
|
Atherosclerosis is a form of ______________ that is characterized by a localized accumulation of _____________ (atheroma), ___________ ________ cells, collagen, fibrin, and platelets that form w/in or the beneath the ____________ of the blood vessel.
This type of plaque usually occurs at the ________ of the vessel, ex: ____________ |
- arteriosclerosis - lipid-containing material - smooth muscle - intima surface
- origin - prox ICA |
|
|
Fatty streak is a thin layer of ______ on the _____ of the artery.
A ______________ is an accumulation of lipids that is covered by more lipid material, collagen, and elastic fiber deposits. |
- lipid material - intimal layer
-fibrous plaque |
|
|
A __________ _________ is a fibrous plaque that contains fibrous tissue, more collagen, calcium and cellular debris.
An ____________ __________ is characterized by the deterioration of the normally smooth surface of the fibrous cap. These are of particular importance because they may ______ that ________ distally.
|
- complicated lesion
- ulcerative lesion - shed debris - embolizes |
|
|
___________ _________ is evident on duplex as a sonolucent area w/in the plaque. This finding is also important as the plaque may be at higher risk for __________ resulting in ___________. |
- Intraplaque hemorrhage - rupture - distal embolization |
|
|
203
How would you describe this plaque?
- Fatty streak - fibrous plaque - heterogeneous plaque
|
- Fatty streak
The thin layer of lipid material on the arterial wall can be difficult to visualize because of its low level echoes. Color flow Doppler is helpful in determining that the vessel does not fill completely. |
|
How would you describe this plaque?
- Fatty streak - fibrous plaque - heterogeneous plaque
|
- Heterogeneous
The quality of this plaque is consistent w/the variety of cellular material it is composed of |
|
How would you describe this plaque?
- Fatty streak - fibrous plaque - heterogeneous plaque |
- fibrous plaque
The increased amt of collagen in this fibrous plaque makes it easily visible on BMode imaging |
|
How would you describe this plaque?
- Fatty streak - Fibrous plaque - A complicated lesion - ulcerative lesion |
- ulcerative lesion
Although it is very difficult to accurately determine surface characteristics w/B-mode this scan using power doppler clearly illustrates the crater-like formation of the arterial wall |
|
How would you describe this plaque?
- Fatty streak - Fibrous plaque - A complicated lesion - ulcerative lesion - Intraplaque hemorrhage |
- Intraplaque hemorrhage
The well-defined area of low-level echoes in the center of the lesion suggests instability and the risk of plaque rupture w/distal embolism |
|
|
What are the 5 mechanisms of disease? |
- Stenosis
- Embolism
- Thrombosis
- Aneurysm
- Nonatherosclerotic lesions |
|
|
An embolus is a ____ or piece of a ___ that moves through the circulatory system until it lodges in a ___________.
They may be _________, ______, ________ and may arise from the body or may enter from without.
What is the most frequent source of emboli?
Another common source? |
- foreign substance - thrombus - distant blood vessel
- solid, liquid, or gaseous
- The heart
- Atherosclerotic plaque -- can break off, travel distally and lodge in a small or stenotic vessel |
|
|
__________ ________ is a bright plaque in the vessels of the retina.
Detected by an __________.
These are actually atheromatous emboli that contain _____ _______ and may have originated from plaque in either the carotid artery or more proximal vessels. |
- Hollenhorst plaque
- Ophthalmologist
- cholesterol crystals |
|
|
Thrombosis: This aggregation of blood factors is composed primarily of _______ trapped w/in a network of _____. One of the most common causes of a __________, it alters cerebral perfusion secondary to a __________ or ________. |
- platelets - fibrin - stroke - stenosis - embolism |
|
|
T or F:
A stenosis, embolism, or thrombosis may exist individually but not in combination |
FALSE:
A stenosis, embolism, or thrombosis may exist individually or in combination |
|
|
An aneurysm is an abnormal, ________ dilatation of a blood vessel due to ________ ________ or ________________, which may be caused by ______, infection or __________.
Aneurysms ____ occur in the cervical carotid artery . |
- localized - congenital defects - weakness of the vessel wall
- trauma - atherosclerosis
- rarely |
|
|
19-6 |
19-6 |
|

Match the atherosclerotic change w/the image
A) stenosis B) stenosis w/surface platelets C) Embolic process D) Thrombosis |
D) Thrombosis |
|
Match the atherosclerotic change w/the image
A) stenosis B) stenosis w/surface platelets C) Embolic process D) Thrombosis |
B) stenosis w/surface platelets |
|
Match the atherosclerotic change w/the image
A) stenosis B) stenosis w/surface platelets C) Embolic process D) Thrombosis |
C) Embolic process |
|

Match the atherosclerotic change w/the image
A) stenosis B) stenosis w/surface platelets C) Embolic process D) Thrombosis |
A) stenosis |
|
|
7 nonatherosclerotic lesions:
A_____________ C ________________ D________________ C_______________ F_________________ N___________________ T_____________________ |
- Arteritis
- Carotid body tumor
- Dissection
- Collagen vascular connective tissue disorders
- Fibromuscular dysplasia
- Neointimal hyperplasia
- Trauma |
|
|
Arteritis is an ___________ of an artery or arteries.
What are the 2 types of arteritis?
|
- inflammation
- Takayasu's arteritis
- Temporal arteritis |
|
|
Takayasu's arteritis is a __________ inflammation that results in ________ of the arteries.
The resulting arterial occlusion or near-occlusion explains why Takayasu's is also known as __________.
|
- chronic - narrowing
- Pulseless disease |
|
|
Takayasu's arteritis:
Type I lesions involve the ________ and its branches
Type II involves the thoracic and _________ _______.
Type III includes the ___________, ________, _________ & ________.
Type IV is related to _______. |
- aortic arch
- abdominal aorta
- aortic arch, its branches, and the thoracic and abdominal aorta
- pulmonary vessels |
|
|
T or F:
Temporal arteritis is the inflammation of the proximal superficial temporal artery and/or its branches |
FALSE:
Temporal arteritis is the inflammation of the DISTAL superficial temporal artery and/or its branches
|
|
|
Temporal arteritis may cause a severe headache and/or sudden ____________ blindness |
unilateral |
|
|
The carotid body tumor is a small mass of _________ that adjoins the _________.
It functions as a ________ sensitive to changes in the __________ _________ of the blood and signals necessary changes in respiratory activity to maintain homeostasis.
Excision of the tumor may also require ligation of the ______ and/or _________ artery. |
-vascular tissue - carotid sinus
- chemoreceptor - oxygen tension
- ICA - ECA |
|
|
T or F:
Tumors are highly vascular structures that develop between the ICA and ECA, and they are usually fed by the ICA |
FALSE:
Tumors are highly vascular structures that develop between the ICA and ECA, and they are usually fed by the ECA |
|
|
Dissection is most commonly caused by ______ that results in a ___________ in the _______ _______.
This creates a _________ _____ which may gradually extend proximally or distally. |
- trauma - sudden tear - intimal wall
- false lumen |
|
|
Blood in the false lumen of a dissection may ______________.
Extension of the false lumen may result in ______ ______ to blood flow. |
- thrombose
- complete obstruction |
|
|
FMD is most commonly caused by _______ of the _________ along w/overgrowth of collagen.
This occurs in the _______ segments of vessels, unlike atherosclerosis which develops at the ____ of vessels.
Characteristic _________ appearance on angiography.
Seen more often in ____________. |
- dysplasia - media (dysplasia of the intima is less frequently seen)
- mid to distal - origin
- beadlike
- younger women |
|
|
Neointimal hyperplasia is when _________ results from rapid production of _________ _____ ____.
Hyperplasia is a response to _________ _____ which may be the result of _________ _______ EX: carotid endarterectomy |
- intimal thickening - smooth muscle cells
- vascular injury - vascular reconstruction |
|
|
Denuding the endothelium surgically leads to ________ __________, endothelial regeneration, and ___________ of smooth muscle cells.
A hemodynamically significant stenosis may develop w/in ___________ to _____ following CEA. |
- platelet accumulation - proliferation
6 - 24 months |
|
|
Trauma:
Traumatic damage to vessels and surrounding tissue can produce a variety of conditions: hemorrhage, __________, fistula, dissection, & ________. |
- occlusion
- pseduoaneurysm |
|

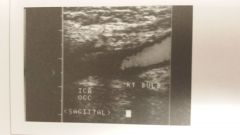
What is the image?
- FMD - Neointimal hyperplasia - Dissection - Carotid Body Tumor - Thrombosis - Aneurysm |
- FMD |
|

What is the image?
- FMD - Neointimal hyperplasia - Dissection - Carotid Body Tumor - Thrombosis - Aneurysm |
- Carotid Body Tumor |
|

What is the image?
- FMD - Neointimal hyperplasia - Dissection - Carotid Body Tumor - Thrombosis - Aneurysm |
- Aneurysm
Aneurysmal disease of the cervical carotid artery documenting focal dilatation of the distal CCA.
* Most pts evaluated for carotid aneurysms have very tortuous CCAs. |
|

What is the image?
- FMD - Neointimal hyperplasia - Dissection - Carotid Body Tumor - Thrombosis - Aneurysm |
- Dissection |
|
What is the image?
- FMD - Neointimal hyperplasia - Dissection - Carotid Body Tumor - Thrombosis - Aneurysm |
- Thrombosis |
|

What is the image?
- FMD - Neointimal hyperplasia - Dissection - Carotid Body Tumor - Thrombosis - Aneurysm |
- Neointimal hyperplasia |
|
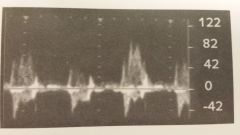
In which of these would you expect to see this type of flow?
- FMD - Neointimal hyperplasia - Dissection - Carotid Body Tumor - Thrombosis
|
- Dissection |
|
|
Name the 4 vessels of anterior circulation
What do they supply blood to? |
- ICA - ACA - MCA - Anterior communicating arteries
- brain's cerebral hemispheres |
|
|
The left hemisphere of the brain controls the ______.
The right hemisphere of the brain controls the ____________.
The term ______ may be used to indicate which side or hemisphere of the brain has been affected. |
- right side of the body
- left side of the body
- "lateralizing" |
|
|
T or F:
A left hemispheric stroke results in neurologic deficits to the left side of the face and body |
FALSE:
A left hemispheric stroke results in neurologic deficits to the RIGHT side of the face and body |
|
|
Left arm numbness is consistent w/decreased perfusion of the right hemisphere by the ____________.
"Nonlateralizing" sxs (ex: ataxia, vertigo) are usually associated w/problems of the ______ or the ___________. |
- anterior circulation
- brain stem - posterior circulation |
|
|
What is amarousis fugax?
|
- Temporary monocular blindness |
|
|
T or F:
A monocular vision problem is related to disease of the contralateral ICA |
FALSE:
A monocular vision problem is related to disease of the IPSILATERAL ICA |
|
|
Neurologic deficits of Ant Circulation:
____________ paresis _____________ paresthesia or anesthesia _____________ or ___________ ____________ abnormalities _____________ fugax Homonymous _____________ |
- unilateral
- unilateral
- dyphasia or aphasia
- behavioral
- amarousis
- hemianopia |
|
|
unilateral paresis: ______ or slight _____ on one side of the body.
Unilateral paresthesia or anesthesia: __________, ___ or lack of _________ on one side of the body. |
- weakness - paralysis
- numbness - tingling - feeling |
|
|
Dysphasia: _________ ______.
Aphasia: the ___________ to ________.
The left hemisphere is dominant for speech, ______ capabilities, verbal and _________ memory. |
- impaired speech
- inability - speak
- analytical - auditory |
|
|
A _______ handed person w/a lesion in the left MCA may cause dysphasia or aphasia.
The __________ hemisphere is dominant in a left-handed person. |
- right
- right |
|
|
Behavioral abnormalities frequently accompany ischemia of the _________ ____ and can be caused by ________ of the right ______. |
- temporal lobe
- infarction
- MCA |
|
|
Amarousis fugax is temporary ______ or _____ usually of only one eye.
Pts typically describe the visual loss as _____________.
|
- partial - total blindness
" a shade coming down over the eye"
|
|
|
T or F:
Because the ophthalmic artery arises from the ICA, the origin of the embolic process causing the temporary visual loss may be a lesion in the contralateral ICA. |
Because the ophthalmic artery arises from the ICA, the origin of the embolic process causing the temporary visual loss may be a lesion in the IPSILATERAL ICA. |
|
|
Homonymous hemianopia is blindness in the __________, _______ & _______ visual fields.
This loss of vision on ______ of the visual field of ______ eye(s) may be evident after a ________ affecting the _________ _____. |
- corresponding - right - left
- 1/2 - both - stroke - cerebral cortex |
|

T or F:
You would expect these signs/sxs w/hemispheric problems |
FALSE:
|
|

Which system would you expect to see the signs/sxs with for this? |
A: Hemispheric signs/sxs
|
|

Which system would you expect to see the signs/sxs with for this? |
B: Vertebrobasilar signs/sxs |
|
|
Posterior circulation is also referred to as ____________.
Name the 4 vessels of posterior circulation
They supply blood to the ______, ____ and _______ of the brain. |
- vertebrobasilar
- vertebrals - Basilar - PCAs - posterior communicating arteries
- brain stem - cerebellum - occipital lobes
|
|
|
Sxs of brain ischemia that may be caused by posterior circulation problem:
V __________ A _____ Bilateral ____________ __________ Bilateral _______ or ___________ _________ ______. |
- vertigo
- ataxia
- visual blurring
- diplopia (double vision)
- paresthesia or anesthesia
- drop attack |
|
|
Vertigo (difficult in _____ _____); a sensation of either moving around in space or having _______ around the person.
Ataxia (muscular _________), usually described as the inability to ______ _____ or to ________ an article w/the _________. |
- maintaining equilibrium - objects move
- incoordination - control gait - touch - hand |
|
|
Bilateral paresthesia: the sensation of _________ or _______ of the skin.
Bilateral anesthesia: loss of _____________.
Drop attack: falling to the ground _____ other sxs or ____________. |
- prickling - tingling
- sensation
- without - loss of consciousness |
|
|
Nonlocalizing sxs:
D_____________ S_____________ Difficulty w/___________ H______________ C_____________ |
- dizziness
- syncope
- speech
- headache
- confusion |
|
|
Dizziness is a sensation of whirling w/in one's head, ____ and a tendency to ___________.
Syncope is a transient loss of ___________. |
- lightheadedness - fall
- consciousness |
|
|
Infarction of the ____________ is the most common cause of a stroke. |
MCA |
|
|
Auscultation:
Normal flow patterns are evident when listening through ______________.
The normal lub-dub sound corresponds w/closure of the ______ valves followed by closure of the _________ and ____ valves. |
- stethoscope
- atrioventricular - aortic - pulmonic |
|
|
Bruits are abnormal sounds heard on auscultation caused by _____ blood flow patterns that set up a vibratory response in the tissue--as happens w/significant stenosis.
Because bruits may arise from lesions other than those at the carotid bifurcation and they may be absent in severe stenosis or occlusion, cervical bruits are a _________ sign of hemodynamically significant carotid artery disease. |
- turbulent
- nonspecific |
|
|
The absence of a bruit does not exclude ____________ because a ___________ may not produce a bruit.
A previously documented bruit that is no longer evident may indicate a lesion has progressed from < _____ to > _____ DR (preocclusive). |
- presence of a stenosis - preocclusive lesion
90 90 |
|
|
Common sites for bruit evaluation include to ___________ for the CCA, ___________ for the bifurcation and just above or below the __________ for the subclavian artery.
The __________ in the __________ is a commson site for ausculation when obtaining bilateral BP measurements.
Unqual measurements may be related to __________ or ___________ disease.
|
- low to mid neck - mid to distal neck - clavicle
- brachial artery - antecubital fossa
- subclavian - axillary |
|
|
The ________ strength is evaluated manually. The strength of it is graded and compared to other sites on the _____ as well as to the same site on the _____________.
What are the 5 common sites for this? |
- pulse - same side - contralateral side
- CCA - Superficial temporal - subclavian - axillary - brachial arteries |
|
|
ICA sxs:
___________ weakness p_____________ n_________ and/or s_______ ___________ ipsilateral __________ _________ and/or b___________ may have ___________ if dominant hemisphere occasionally altered _______ of ___________ |
- contralateral
- paralysis
- numbness - sensory changes - amarousis fugax - bruit - aphasia |
|
|
MCA signs/sxs:
A ________ or D ___________ Severe ___________ hemiparesis or h__________ that is more severe in the ________ and ______ rather than the ________ if upper division of MCA occluded d _________ __________ changes ________ state ________ _____ if lower division MCA occluded |
- aphasia or dysphasia
- contralateral - hemiplegia - face - arm - leg
- dysarthria
- behavioral
- confusional
- agitated delirium
|
|
|
ACA signs/sxs:
Contralateral ______ (especially in the _____) I_________ Loss of _____________ Impaired _______ and _______ functions |
- hemiparesis - leg
- incontinence
- coordination
- motor - sensory |
|
|
Vertebrobasilar signs/sxs:
___________ around lips & mouth D______ (double vision) poor __________ D________ v_______ A_______ A___________ |
- numbness
- diplopia
- coordination
- dysphagia
- veritgo
- amnesia
- ataxia |
|
|
Posterior cerebral signs/sxs:
D ___________ C_________ (paralysis usually absent) |
- dyslexia
- coma |
|
|
Post |
sxs |
|
|
The __________ can detect hemodynamically significant lesions of the ICA by evaluating flow to some of its terminal branches.
The patient is positioned _____ w/the head of the bed ____________ ________ and the pts head can ________________.
|
- periorbital Doppler examination
- supine - slightly elevated - rest on a pillow |
|
|
Limitations of periorbital Doppler exam:
It is only diagnostic in cases of ______ ____ ___________.
It cannot _____ an ___________ from an _______.
It requires considerable _________ |
- hemodynamically significant lesions
- differentiate - occlusion - tight stenosis
- skill |
|
|
When a sound wave is reflected from a moving target, the ____ of the ________ ______ differs from that of the ___________ ______.
This difference (___________ ______) occurs whenever there is relative motion between the ___________ and the ________ of the sound wave.
In evaluation of blood flow, the ___________ is the moving target and the ___________ is the stationary source and the __________ of the sound waves. |
- frequency - received wave - transmitted wave
- Doppler effect - source - receiver
- RBC's - transducer - receiver
|
|
|
Periorbital technique:
Patient is _______ w/________ _______.
Using an _________ Doppler, the examiner locates the ________ _____ at the inner __________ of the eye.
The _______ _____ is automatically calibrated when the equipment is turned on.
|
- supine - eyes closed
- 8-10 MHz - frontal artery - canthus
- analog recorder |
|
|
T or F:
Flow in the frontal artery should be retrograde |
FALSE:
Flow in the frontal artery should be ANTEGRADE.
* Probe must be positioned carefully so that antegrade flow is not misrepresented as retrograde flow |
|
|
A series of ___________ _______ are performed to detect the presence of or abnormal __________ _____ which suggest disease.
These are performed both ___________ and _____.
What 4 arteries are these performed on? |
- compression maneuvers - collateral channels
- ipsilaterally - contralaterally
- Facial artery - Superficial temporal artery - Infraorbital artery - CCA |
|
|
214
What artery is being compressed while obtaining arterial signals from the frontal artery?
Frontal artery is a branch of the ___________. |
- The temporal artery ( branch of ECA)
- ophthalamic artery |
|
|
T or F:
Under normal circumstances, compression of a distal branch of the ECA does result in flow reduction to a distal branch of the ICA. |
FALSE:
Under normal circumstances, compression of a distal branch of the ECA DOES NOT result in flow reduction to a distal branch of the ICA.
* The compression manuever maintains the signals or slightly augments the arterial Dopper signals |
|
|
The CCA must be compressed w/great care to avoid stimulating the _______ and thereby altering ______ and/or rhythm.
Compressions are usually done ________ in the neck to avoid the _________.
Other dangers include decreased __________ and distal __________ of __________ ________. |
- carotid sinus - heart rate
- low - bifurcation
- cerebral perfusion - embolization - dislodged plaque |
|
|
215
Normal or abnormal |
215 |
|
|
215
Normal or abnormal |
215 |
|
|
Normal:
_______ should be evident in the _______ artery.
Compression of the facial, superficial tem[oral and infraorbital arteries should ______ or _______.
_________ compression of the CCA should _______ flow in the _____ artery secondary to decreased flow to the brain.
Flow reversal may also be evident depending on __________ development. |
- Antegrade flow - Frontal
- not diminish - reverse flow
- Ipsilateral - diminish - frontal
- collateral |
|
|
T or F:
Retrograde flow in the frontal artery is consistent w/a hemodynamically significant lesion of the contralateral ICA |
FALSE:
Retrograde flow in the frontal artery is consistent w/a hemodynamically significant lesion of the IPSILATERAL ICA |
|
|
Diminished or reversed flow during compression of the facial, superficial temporal or infraorbital arteries suggests that flow into the ________ artery is being compressed rather than the ___________ ______________. |
- frontal - ipsilateral ICA |
|
|
Decreased or absent flow in the frontal artery w/compression of the superficial temporal artery signifies that flow in the ___________ is ____________.
The superficial temporal artery serves as a__________ to a hemodynamically significant lesion in the ____________ ___________. |
- frontal artery - abnormal
- collateral pathway - ipsilateral ICA |
|
|
T or F:
Oculopneumoplethysmography is a direct test that detects hemodynamically significant lesions of the ICA by evaluating flow in one of its terminal branches |
FALSE:
Oculopneumoplethysmography is an INDIRECT test that detects hemodynamically significant lesions of the ICA by evaluating flow in one of its terminal branches |
|
|
OPG-Gee also provides information about the development of ________ ____ that maintain ________ _________ _________ to the brain. |
- collateral channels - adequate blood flow |
|
|
Limitations of OPG-Gee:
Cannot ascertain the _____ _____ of a stenosis.
It is not diagnostic in cases of __________ or _____________.
It cannot differentiate ______ from a _______ ______.
It is not useful in documenting the _____________ of disease.
It may be incapable of determining the ocular systemic pressure (OSP) in pts w/ ___________ ______. |
- exact location (whichy may be at any point from the origin of the carotid artery to the ophthalmic)
- non-hemodynamically significant - well-collateralized lesions
- occlusion - tight stenosis
- progression
- severe HTN |
|
|
The pt is positioned __________ w/the head of the bed ________ ________ and the pts head can _____________.
|
- supine - slightly elevated - rest on a pillow |
|
|
Plethysmography is a technique that records changes in ____________. In this vascular application, fluctuations in __________ are related to changes in ___________ _______ during systole an diastole.
OPG-Gee measures __________ arterial pressure by applying a ________ to the eye. As it distorts the shape of the globe, intraocular pressure ______ to the point at which it ________ arterial inflow. |
- volume - volume - blood flow * EX: When arterial inflow exceeds venous outflow
- vacuum - increases - obliterates |
|
|
______ _____ recordings are made as the vacuum is slowly decreased.
The pulse waveforms reappears when the ophthalmic arterial pressure __________ the ____________ ____________.
Because the pressure in the ophthalmic artery reflects pressure in the __________ _______, the measurement of the ophthalmic arterial pressure can be useful in detecting ____________ _________ __________. |
- Strip chart
- exceeds - intraocular pressure
- distal ICA - hemodynamically significant lesions |
|
|
OPG-Gee technique:
Thorough pt hx must be obtained to rule out contraindications.
Allergies to ________ ___________.
__________ __________ w/in last 6 months.
A past spontaneous ___________ detachment.
Acute or unstable ____________.
|
- local anesthetics
- eye surgery
- retinal
- glaucoma |
|
|
T or F:
Other ophthalmic disorders that are contraindications are myopia or conjunctivitis |
FALSE:
Myopia and conjunctivitis are NOT considered contraindications to OPG-Gee |
|
|
OPG-Gee technique:
If there are no contraindications, the pt is supine, _______ ____ are applied, bilateral ________ ________ are obtained using a ___________, and the ________ _______ is applied to the eyes. |
- ECG leads - brachial pressures - stethoscope (noting the side of the higher pressure) - local anesthetic |
|
|
OPG-Gee technique:
Calibration or standardization is performed by pressing the _____________ button. Standardized deflections should have an amplitude of approximately ____ on the cart.
If not, examiner presses _____ and adjusts ______ controls for the eye channels, alternating pressing and releasing STD buttons until a ______ deflection is ___________. |
- STD 10 mm
- REC - GAIN 10 mm - evident |
|
|
OPG-Gee technique:
Calibration is critical to the usefulness of this plethysmographic technique since differences in ________ of the tracing are of diagnostic value.
Reduction in the _____ of the tracing should reflect a significant __________ in ___________ ________. |
- size
- size - reduction - blood volume |
|
|
OPG-Gee technique:
Eye cups are placed on the _______ ___________ (whiteness of the eye) not on the ________. After the pt has been informed that he/or she will experience a loss of vision for a few seconds a ______ switch is depressed to ___________ the vacuum.
The vacuum measured in ____________ increases ___________ pressure to obliterate arterial inflow. |
- lateral sclera - cornea - foot - activate
- mmHG - intraocular |
|
|
OPG-Gee technique:
A pt w/a systemic systolic pressure of < 140 mmHG may require only ________ mmHG to occlude inflow.
A pt w/a systemic systolic pressure of > 140 mmHG requires a ___________ volume of ________ mmHG to occlude inflow. |
300
- maximum 500 |
|
|
219
|
219 |
|
|
OPG-Gee technique:
After the vacuum is applied, the recording of _________ pulsations and ________ commences.
As the vacuum is released the ________ in intraocular pressure results in _______ inflow and the _____ of the waveforms.
When optimum waveforms are evident the vacuum is ________, the eye cups __________, and the _________ ______ measured again from the arm w/the __________ _________. |
- ocular - ECG
- decrease - increased - reappearance
- released - removed - brachial pressure - higher pressure |
|
|
If ocular pulsations are evident at the onset of the study using the 300 mmHG setting, blood flow was _____ __________.
The vacuum is deflated, examiner selects the ________ setting, reactivates the vacuum and repeats the study.
Interpretation may be impossible if the tracings are very ________ and suggest ___________. Examiner asks the pt to relax eye muscles as much as possible and repeats study.
When OPG-Gee is required to assess the adequacy of collateral channels, __________ __________ ______ are necessary. |
- not obliterated (EX: systolic pressure was not exceeded)
500 mmHG
- irregular - artifact
- carotid compression maneuvers |
|
|
The examiner must never ________ both CCA's _________.
compression is never performed in the area of the ________ ________ because its stimulation can alter HR and/or rhythm, decrease cerebral perfusion or cause distal embolization from dislodged plaque.
|
- compress - simultaneously
- carotid sinus
|
|
|
The first phase consists of ______ second compression while the OPG maintains an intraocular pressure of _________ MMHG.
The second phase--only performed if pulsations are noted ______ the _______ _______-- consists of a < or equal to _______ second compression while the OPG decreases intraocular pressure from _____ mmHG to the level at which pulsations reappear.
Carotid compression should be released __________ to prevent the sudden return of ________ blood flow. |
3-5 60
- during - first phase 110
- gradually - turbulent
|
|
|
Normal OPG-Gee:
Since the eye pulse should coincide w/the upstroke of the ___________ on the ECG, this is used to differentiate true eye pulses from artifact (blinking).
Identify the first significant _______ pulse. Ex: one followed by pulsations of ___________ _____.
Overlay the calibrated ruler on the right eye tracing, aligning the beginning of the ____ w/the appropriate ___ _________. Repeat w/left eye.
|
- T-wave
- eye - increasing amplitude
- upstroke - OSP reading |
|
|
Normal OPG-Gee:
Ophthalmic systolic pressures should not differ by ___________.
If the first significant eye pulse on the right appears at the identical OSP on the left, then these is ___ difference in OSPs.
A normal ratio of __________ to __________ pressure should exist.
OSP - 39 / brachial systolic pressure (BPS) > or equal to __________
A scoring grid w/values above the line demonstrates a ________ ratio. |
> or equal to 5 mmHG
< 5 mm
- ophthalmic to systemic
0.430
- normal |
|
|
If the OSPs are > 140 mmHG the examiner measures the amplitude of the _________ _______. The difference in amplitude of the tracings should be _________.
OSPs that differ by _________ and/or an abnormal ratio ophthalmic to systemic pressure:
OSP - 39 / BSP < or equal to ____________
Presence of a hemodynamically significant lesion is evidenced by either a difference in __________ _________ and/or abnormal _____ of _______________________. |
- first pulses < or equal to 2 mm
> or equal to 5 mm
0.429
OSPs > or equal to 5 mm - ratio - ophthalmic to systemic pressure |
|
|
222 |
222 |
|
|
222 |
222 |
|
|
If the OSPs exceed ________ the size of the first pulses are measured. A difference in amplitude of _______ is abnormal and the side w/the ________ __________ is considered positive.
|
140 mmHG > 2 mm - least amplitude |
|
|
Trouble-shooting OPG-Gee:
_______ _____ (very irregular deflections not associated w/the cardiac cycle) may be eliminated by reapplying __________ ________.
_____ ______ may make the identification of the first significant pulse difficult.
Very diminished _______ bilaterally may suggest significant cardiac ___________. |
- blink artifact - topical anesthetics
- cardiac arrhytthmias
- tracing - dysfunction (EX: cardiomyopathy) |
|
|
Duplex scanning (with or without color flow imaging) is an accurate way of localizing the _________ of __________ in the extracranial carotids.
In addition it can differentiate an ________ from a __________ w/a high degree of _______________. |
- presence - arterial disease
- occlusion - tight stenosis - accuracy |
|
|
Duplex scanning is capable of documenting and following the ________ of non-hemodynamically significant lesions.
It provides information about the _______ ___________ of plaque and may help to identify the source of ___________ phenomena.
It can be used to evaluate _______ ____ in the carotid or subclavian regions.
|
- progression
- surface characteristics (ex: smooth or irregular) - embolic
- pulsatile masses |
|
|
Duplex US may be adversely affected by:
The presence of _________, skin ___________, or ____________.
The _________ or _______ of the neck.
Patient _____________.
The __________ or _________ of the vessel.
Rapid ___________ pattern.
__________ _________ from calcification. |
- dressings - staples - sutures
- size - contour
- movement
- depth - course
- respiratory
- Acoustic shadowing |
|
|
T or F:
Duplex US may overestimate or underestimate disease when an inappropriate Doppler angle is used |
TRUE |
|
|
T or F:
Duplex US may underestimate disease when artifact is mistaken for plaque |
FALSE:
Duplex US may OVERESTIMATE disease when artifact is mistaken for plaque |
|
|
Duplex US may overestimate disease when _________ ________ is mistakenly attributed to a stenosis.
Other causes of ______ ________ measurements include increased _______ ________, vessel __________, __________ flow for ipsilateral or contralateral disease, hyperemia, and/or a _______ vessel. |
- accelerated flow
- increased velocity - cardiac output - tortuosity - hypoplastic |
|
|
T or F:
Duplex US may overstimate disease when artifact is mistaken for plaque and when a high bifurcation precludes thorough evaluation of the ICA |
FALSE:
Duplex US may overestimate disease when artifact is mistaken for plaque but will UNDERESTIMATE when a high bifurcation precludes thorough evaluation of the ICA |
|
|
Duplex US may underestimate disease when:
It fails to appreciate very ______ _____ echoes of _______ plaque.
The examiner does not carefully interrogate the vessel and misses _______ _______.
A ______, ______ plaque formation may not have the _______, _______ flow patterns usually associated w/a hemodynamically significant lesion. |
- low level - soft
- accelerated flow
- long - smooth - accelerated - turbulent |
|
|
Pt positioning:
Pt should be in a comfortable ___________ or _________ position w/the head slightly ______ and ________ slightly _________ from the side being interrogated. |
- reclining - supine - hyperextended - turned - away |
|
|
Physics:
Duplex US combines __________ information based on __________ ________ (spectral analysis) w/ the _______ information of real-time, high resolution, B-Mode (gray scale) ultrasonic imaging.
In addition to the info provided by conventional duplex US, color flow imaging evaluates the Doppler flow info for its _______ (__________ ______ or _______ from the _________, on which basis of color is __________), and its ________ content (which determines the _____ or _____ of the assigned color). |
- physiologic - Doppler-shifted frequencies - anatomic
- phase - direction - toward - away - transducer - assigned
- frequency - hue - shade |
|
|
CW Doppler uses ______ _________ crystals.
One to emit ultrasound ____________ and the other to ________ the __________ ______ ________.
This results in a fixed ________ ________ and no _______ ________ or ability to place the _______ _____ at a specific ___________.
Nor can continuous wave US create __________ _________. |
- two - piezoelectric
- continuously - receive - reflected waves continuously
- sample size - range resolution - sample volume - depth
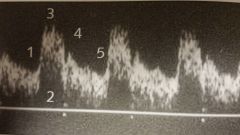
- anatomic images |
|
|
Continuous wave has ___________ use in carotid exams. It may provide a simple method to determine _______ of the carotid arteries and/or to provide limited ______ _____ characterization in very specific ___________, such as the operating room following a _______.
It may also be used when severely ________ ________ are evident.
In some cases, CW Doppler may be the _____ means available to accurately display these very ______ ______. |
- limited - patency - blood flow - settings - carotid endarterectomy
- elevated PSV's
- high velocities |
|
|
Pulsed Doppler does ___________ ________ transmit and receive US.
The ______ crystals in the pulsed Doppler transducer are excited in a ____ ________ producing US waves.
This ______ of transmission is followed by a " __________" period during which the crystals _______ the ________ _______. |
- not - continuously
- multiple
- quick - burst
- burst - listening - detect - reflected signals |
|
|
Signals from more superficial structures are received _______ ___________ after transmission.
Signals from deeper structures are detected after a _________ ___________ ________.
This feature of pulsed Doppler called _______ _______, allows signals only from ___ _____ to be processed, thereby controlling _______ ____ and ________ ___________.
|
- almost immediately
- longer listening period
- range resolution - specific depths - sample size - range resolution |
|
|
Range resolution allows two vessels located directly above one another to be evaluated _______ and vessels also can be followed as their __________ changes.
___ _____ w/spectral analysis is the primary tool utilized for the evaluation of blood flow.
It provides very accurate blood flow characterization in conjunction w/an _______ of the ___________.
This combination of __________ and anatomic information is the basis of duplex US. |
- separately - course
- Pulsed Doppler
- image - anatomy
physiologic (blood flow) |
|
|
Reproducible and consistent velocity measurements require an angle of ___________ degrees.
Although an angle of ____ provides the greatest Doppler shift is not used in clinical applications because most vessels of interest are ______ to the skin surface so this angle of insonation is not possible. And the criteria used in interpreting the significance of frequency or velocity measurements were established using a ______ degree angle. |
45-60
0 - parallel 60 |
|
|
A ________ is not always attainable.
Due to _________ _______ of the arteries or even under normal circumstances, the normal ___________ of the arteries.
In such cases the angle of insonation is more often less than _______ degrees and usually in the __________ range.
Measurement variability (error production) can occur w/angles ________ degrees more frequently than w/angles less than __________.
It is very important that each vascular center _______ validate their criteria for diagnosing carotid stenosis in order to determine their _____ _______. |
60 degree angle
- anatomic location - curvature
60 45-60
greater than 60 60 derees
- independently - overall accuracy |
|
|
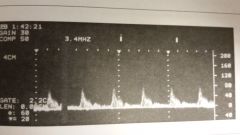
Spectral analysis is a method of displaying the variety of _________ of the flowing blood during _________ and ___________.
The scanner's built in FFT ( _______ _____ ______) technology automatically _______ and displays the individual ________ of the ________ signals, creating a velocity profile that consists of _______ on the horizontal axis, _______ on the vertical axis, and _______________ as brightness. |
- frequencies - systole - diastole
- fast fourier transform - analyzes - frequencies - returned - time - frequency shifts - amplitude (intensity of the signals) |
|
|
CW Doppler produces a very _____ spectrum because all of the layers of blood flow are displayed, from _______ flow near the wall to _______ flow in center stream.
With CW Doppler ________ _______ is an expected finding even w/laminar flow.
Pulsed Doppler produces a _________, _____ spectrum when a limited number of _______ or velocities are evident in laminar flow.
With Pulsed Doppler __________ _______ is often associated w/turbulent flow. |
- broad - slow - faster
- spectral broadening
- narrow - well-defined - frequencies
- spectral broadening
|
|
|
Color flow Doppler info is displayed on the image _________ it is evaluated for its ____ ________ (which determines the hue or shade of the color) and its _______ (direction toward or away from the probe).
The position of the ________ _________ as well as the flow direction depicted on the _______ ________ assist in determining whether the blood is moving toward or away from the US beam. |
- after - frequency content - phase
- color box - color bar
|
|
|
A _____, ___, or ___ MHz transducer is used.
The sample volume of the pulsed Doppler is usually kept as _______ as possible and placed in the _______ of the vessel and/or the flow channel.
Measurements of a stenosis in the ____ view can be very misleading since most plaque formations are not ________. Therefore, the size and shape of the plaque formation can vary according to the _____ of ________.
This problem can be solved by ensuring that _______ ______ are used when imaging the vessel.
In a transverse view, the total ___ of the vessel and plaque formation can be more accurately seen. |
5 7.5 10
- small (1-1.5mm) - center
- sagittal - symmetrical - angle - insonation
- multiple approaches - circumference |
|
|
Longitudinal view:
Vessels are followed from the clavicle to the mandible w/the ________, ______, _____ and ____ projections to identify and evaluate plaque formations.
Avoid pressing too hard as stimulation of carotid sinus can decrease ______ and alter _______ __________.
|
- anterior - oblique - lateral - posterior
- cardiac output - heart rhythm |
|
|
Longitudinal view:
When activated, spectral analysis of the CCA, ICA, and ECA is performed automatically by the scanner's computerized ____ algorithm.
Examiner places and maintains a ______ ___ _____ in midstream or w/in the flow jet in order to obtain the most diagnostic info.
________ must be properly controlled, too much can be misinterpreted as turbulent flow, too little may result in an image that is difficult to evaluate. |
- FFT
- small sample volume
- gain settings |
|
|
Comparison of flow characteristics from ______ ______ to the other and from _______ to ______ segments of the _______ carotid system is essential.
Comparing the level of the _____ is also important as increased flow in a collateralized ECA has been misinterpreted as a patent ICA in cases of ipsilateral ______ ____.
The ECA is mistaken for the _______ and a branch of the ECA is thought to be the __________. |
- one side - proximal - distal - ipsilateral
- bifurcation - ICA occlusion
- ICA - ECA |
|
|
Longitudinal view:
With a clear view of the CCA, the probe is slowly angled _________ to identify the vertebral artery.
The artery will have vertical _____ running through it from the ______ __________ of the vertebrae, giving it the appearance of ______.
Flow direction is routinely demonstrated, the ____ of the vertebral artery may also be evaluated for stenosis.
- Normal vertebral flow pattern is _____ ______. |
- posterolaterally
- shadowing - transverse processes - H's
- low resistance |
|
|
227
Is this normal or abnormal flow pattern for the vertebral artery? |
Normal low resistance |
|
What view is this of normal CCA, ICA and ECA |
sagittal |
|
|
Transverse view:
The vessels are followed from the clavicle to the mandible to identify and evaluate _____ _______.
The __________ _______ calculations are documented. |
- plaque formations
- percentage stenosis (Ex: diameter reduction) |
|
|
B-Mode normal:
A solid ______ should be evident between the walls of the vessel, indicating the ___________ of atheromatous material (plaque), whose density differs from that of flowing blood.
An _______ line separating the endothelium from the medial layer of the arterial wall should be evident.
This allows for measuring _______ __________ __________, a tool currently regarded as a ______ of cardiovascular disease. It can also be used to monitor the effects of risk factor modification and _________ agents such as lipid-lowering drugs. |
- color - absence
- anechoic
- intima-media thickness (IMT) - predictor - pharmacological |
|
|
Technique involves using multiple ____ views of the CCA and ICA. ________ measurements of the __________ CCA and _________ ICA are most widely used.
Measurements can be made manually w/ __ or w/software assisted analysis programs.
IMT normally _______ w/age.
An IMT < or equal to _____ is generally considered to be WNL for people older than 60. |
- sagittal - Far-wall - distal -proximal
- calipers
- varies
0.9 mm |
|
|
B-Mode abnormal:
Fatty streaks: ______ ____ echoes of similar appearance that can be found in persons of all ages.
Fibrous _____ plaque: ______ _________ level echoes of similar appearance.
Complex plaque: _____, ____, and ___ level echoes (______________) indicating soft and dense areas. |
- low level
- soft - low to medium
- low- - medium- -high |
|
Homogeneous or heterogeneous plaque?
Fatty streaks, fibrous soft plaque or complex plaque? |
- Homogeneous
- Fibrous soft plaque |
|

Homogeneous or heterogeneous plaque?
Fatty streaks, fibrous soft plaque or complex plaque? |
- heterogeneous
- complex plaque |
|
|
Calcification: very bright, ____ ____ echoes. The ________ __________ from the calcium deposit prevents a thorough evaluation of the vessel and may result in the calculation of an ________ percentage stenosis.
Because _______ _______ has the same echogenicity of flowing blood, careful interrogation w/Doppler is necessary to ensure that there is no hemodynamically significant lesion.
The _________ __________ of plaque may be described as smooth, slightly irregular, grossly irregular, or craterlike. |
- highly reflective - acoustic shadowing - erroneous
- fresh thrombus
- surface characteristics |
|
|
Stenosis: ideally plaque should be visible from at least ________ of the longitudinal or sagittal projections and in the transverse view.
Depending on the type of occlusive process, the vessel may be filled w/________ _____ material or be __________.
______ findings are essential to the dx of a probable occusion, some _______ characteristics are helpful.
A vessel may be completely filled w/_____ or moving in a ______ ________ motion. |
- two
- highly echogenic - anechoic
- Doppler - B-Mode
- echoes - horiztonal pistonlike |
|
|
Since standard duplex may not be able to detect a tiny residual lumen, a ______ _____ is important to utilize enhanced Doppler processing to display all flow patterns regardless of _____ or ________ of flow.
Referred to as Doppler _______ or ______ Doppler, the display of a solid color w/in the flow channel designates a _______ ___________; the absence of color suggests _________.
Caution is advised in dx a carotid occlusion based on ________ or ______ info alone.
|
- string sign - speed - direction
- energy - power - residual lumen - an occlusion
- B-Mode - color |
|
|
The ICA is slightly more _______ and _________ than the ECA. Since the brain is a _______ vascular bed, the flow in the ICA is less ________ w/__________ flow during ____________.
The waveform of the ICA has a ___________ upstroke, the downstroke has a high ______ component . A _______ ________ may not be clearly evident. |
- high-pitched - continuous - low resistance - pulsatile - increased - diastole
- rapid - diastolic - dicrotic notch |
|
|
T or F:
The terms triphasic, biphasic and monophasic are applied to the blood flow patterns of the cerebral vasculature as they are to those of the peripheral vasculature. |
FALSE:
The terms triphasic, biphasic and monphasic are NOT applied to the blood patterns of the cerebral vasculature as they are to those of the peripheral vasculature |
|
|
Since the ECA supplies blood to vascular beds that have a _____ peripheral resistance (EX: the face and scalp), he ECA signal is more _________ than the ICA.
It appears more similar to the signals from the _______ vessels.
The ECA has a __________ upstroke and downstroke w/a very _____ ________ component.
A __________ ________ is clearly seen, and tapping of the ______ _____ artery anterior to the ear causes __________ in the waveform. |
- higher - pulsatile
- peripheral (EX: CFA)
- rapid - low diastolic
- dicrotic notch - superficial temporal (STA) - oscillations |
|
|
The _________ has flow characteristics of both the ECA and ICA.
Because the sample volume of a pulsed Doppler can be more precisely placed in center stream, the signals will have a __________ band of frequencies in systole w/a _______ area, spectral window under that _______ _________.
The presence of these qualities is consistent w/_________ _________. |
- CCA
- narrow - "blank" - narrow band
- laminar flow
|
|
What are the 5 components of this waveform? |
1) systolic upstroke 2) frequency (spectral) window 3) peak systole 4) dicrotic notch 5) end diastole |
|
|
A CW Doppler is not able to regulate _____ ____ or _____ and so its frequency window is _____ as _________. |
- sample size - depth - not - apparent |
|
|
A stenosis is characterized by a ___________ _______ sound than normal, w/a very high-pitched ____________ or _______ type of signal evident ________ a significant stenosis.
The waveform of a stenotic vessel has ________ _______ that correspond w/the _______ _____ through the narrowing.
The signal has higher than normal velocities in ________ and ___________. |
- higher-pitched - hissing - squealing - at
- higher velocities - accelerated flow
- systole - diastole |
|
|
In spectral analysis, the band evident along the top of the waveform during _________ may ________ ____ the spectral window.
This ______ ___ is considered _______ _______ and is consistent w/multiple frequencies (ex: turbulent flow). |
- systole - fill in
- vertical thickening - spectral broadening |
|
|
233 CW or PW? |
CW or PW? |
|
|
CW or PW? |
CW or PW? |
|
|
CW or PW? |
CW or PW? |
|
|
CW or PW? |
CW or PW? |
|
|
CW or PW? |
CW or PW? |
|
|
CW or PW? |
CW or PW? |
|
|
233 |
233 |
|
|
233 |
233 |
|
|
As the stenosis progresses, systolic and diastolic frequencies _______________. The spectral band becomes very ______________ resulting in the complete ___________ of the __________.
Distal to a stenosis, disturbed flow patterns are evident such as _____________ and more _________ upstroke, _______ resistance flow, and poststenotic _____________ |
- increases - broad - loss - window
- dampened (decreased velocities) - rounded (increased acceleration time) - low (increased flow in diastole) - turbulence (spectral broadening observed, often times w/bidirectional flow) |
|
|
An absent signal may indicate occlusion a ______ ______ cannot be ruled out.
The flow stream may be extremely difficult to detect due to ________ _____ resulting in no _______ signal. |
- tight stenosis
- slow flow - audible |
|

What is suspected from this image? |
ICA occlusion |
|
|
The loss of a ________ component in the _________ CCA is usually consistent w/an __________ of the ICA.
Often in this situation the ___________ CCA & ICA serve as __________ _________ w/___________ systolic and diastolic flow in those vessels. |
- diastolic - ipsilateral - occlusion
- contralateral - collateral pathways - increased |
|
|
Disease at the carotid siphon occurs ______ compared to the extracranial system, it also must be considered when ______ _____ flow patterns are evident in the extracranial ICA.
Poor cardiac output or stroke volume may result in bilaterally __________ CCA flow velocities. If unilateral, suggests ____ disease
|
- infrequently - high resistance
- diminished - proximal (innominate or CCA occlusive disease
|
|
|
Increased __________ _________ or ____ ______ as seen in some young healthy individuals may result in elevated CCA velocities bilateral.
Antegrade flow in systole w/sustained reversal of flow during diastole may indicate _______ ___________ or _____________. |
- cardiac output - stroke volume
- aortic regurgitation - insufficiency |
|
The doppler signal obtained from the ICA is consistent w/a _______ ________ |
Distal obstruction
- waveform reflects high-resistance rather than expected low-resistance flow pattern
- blockage at carotid siphon |
|
The doppler signal obtained from the CCA are consistent w/ __________ ____________ |
- proximal disease
- Low velocities and increased acceleration time resulting in rounded waveform
- If bilateral, consider poor cardiac output, if unilateral consider proximal vessel |
|
|
What were the 2 important clinical trials evaluating efficacy of carotid endarterectomy that established therapeutic benefit for asymptomatic pts w/ > 60% DR of the ICA and the other for symptomatic pts w/ > 70% DR?
Which criteria uses a ratio?
Which criteria uses EDV? |
- ACAS (Asymptomatic Carotid Atherosclerosis Study)
- NASCET (North American Symptomatic Carotid Endarterectomy Trial)
ratio = NASCET EDV = ACAS |
|
|
ACAS: PSV _______ and EDV of _____________ is consistent w/a > or equal to 60% DR of ICA
NASCET: ________ / ________ ratio of ________ is consistent w/a > or equal to 70% DR of ICA |
ACAS: > or equal to 290 cm/s, > or equal to 80 cm/s
NASCET: ICA PSV/CCA PSV, > or equal to 4.0 |
|
|
T or F:
According to Strandness and UOW:
Normal - 49% stenosis should have a PSF (peak systolic frequency) of < 4 kHz and a PSV of < 125 cm/s |
TRUE |
|
|
According to Strandness and UOW:
A 50-79% stenosis should have _________ PSF, ___ EDF (end diastolic frequency), ______ PSV, and ________ EDV.
An 80-99% stenosis should have _________ PSF, ___ EDF (end diastolic frequency), ______ PSV, and ________ EDV. |
- PSF: > 4 kHz - EDF: < 4 kHz - PSV: > 125 cm/s - EDV: < 140 cm/s
- PSF: > 4 kHz - EDF: > 4 kHz - PSV: > 125 cm/s - EDV: > 140 cm/s
|
|
|
The ICA/CCA ratio is calculated by dividing the highest PSV of the _____ by the PSV of the ________ CCA at a standard distance from its _______ into the _________ & _______.
PSV's can vary in the CCA w/ _________ flow normally detected __________.
Velocity measurements should be obtained at a ________ location. |
- ICA - ipsilateral - bifurcation - ICA - ECA
- faster - proximally
- consistent (EX: approx 4 cm prox to bifurcation--making sure that this part of CCA is not bulbous. |
|
|
Guidlines established by Society of Radiologists in US Consensus Conference:
Doppler criteria cannot be used to predict a _____ ICA stenosis.
Doppler criteria cannot be used to predict ICA stenosis in _____ increments.
Doppler criteria are not accurate for ________ stenosis.
Doppler is not accuate for _________ < 50% stenosis |
- single-percent
10%
< 50%
- subcategorizing |
|
|
Criteria suggested by society of radiologists:
Normal to < 50% DR: ____ PSV, ___ EDV, ___ ICA/CCA ratio
50-69% DR: ______ PSV, ____ EDV, _____ ICA/CCA ratio
70-99% DR: ____ PSV, ____ EDV, ___ ICA/CCA ratio |
PSV: < 125 EDV: < 40 ICA/CCA ratio: < 2.0
PSV: 125-230 EDV: 40-100 ICA/CCA ratio: 2.0-4.0
PSV: > 230 EDV: > 100 ICA/CCA ratio: > 4.0 |
|
|
Doppler evaluation in dx a probable occlusion, findings may include:
The absence of a _____ _____ _____.
The absence of a ____ _____ w/in the flow channel w/ ______ or ______.
Very low or absent ______ component evident in the ipsilateral CCA.
W/ICA occlusion, _____ ____ may be evident as _________ flow in other vessels |
- Doppler arterial signal
- solid color - power Doppler - Doppler energy
- diastolic
- compensatory flow - increased * the ECA, contralateral ICA or either vertebral artery |
|
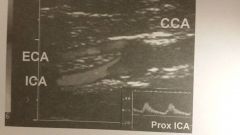
What does this image suggest (ECA is blue)?
|
Occluded CCA
- Retrograde flow in the ECA represents the collateral pathway that is maintaining blood flow to the ICA.
It illustrates how the B-Mode, color flow Doppler and PW Doppler findings can coincide. |
|
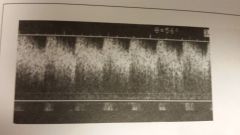
What is artifact is represented in this image?
Why does it occur?
Is true peak flow available?
How could you fix it? |
- Aliasing: Occurs because of the limitations of the equipment being used (EX: a low PRF)
- Maximum frequency is 1/2 the PRF, flow info greater than 1/2 the Nyquist limit cannot be displayed
- No, and waveform has a flat crew-cut appearance
- Change to a lower-frequency transducer, altering the angle of insonation to decrease the depth of the vessel, or using CW Doppler
|
|
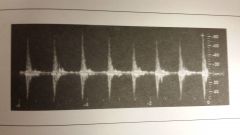
What artifact is represented in this image?
Why does it occur?
Normal helical, or nonaxial flow will also be displayed as some _________ and _____ flow as the blood travels in a spiral motion.
The asymmetrical flow patterns demonstrate the ________ _____ is not traveling _______ to the ________ of the _____ (axial) but rather in a _________ pattern (nonaxial). |
- Crosstalk: The presence of strong reflectors or an overly high gain setting. The Doppler shifts are duplicated above and below the baseline appear in the absence of flow disturbances.
- forward - reverse
- laminar flow - parallel - walls - vessel - corkscrew
- |
|
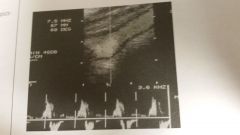
This Doppler spectra depicts _____ flow patterns |
- helical |
|
|
Intraoperative monitoring capabilities:
B-mode imaging can identify defects secondary to carotid __________, such as stricture of the suture line, _____ _____, areas of _______ ____ or residual plaque.
Doppler evaluates the hemodynamic significance of an ___________. |
- endarterectomy - intimal flaps - platelet aggregation
- irregularity |
|
|
Intraoperative monitoring technique:
Transducer is placed inside a ________ ___ after ____ ____ has been put into the sleeve.
The wound is filled w/_________ ______.
The examination proceeds according to the previously described technique.
Areas of _____ __________ identified w/color flow imaging require thorough evaluation of the vessel wall in ____ ____. B-mode US can identify subtle ____ that might be concealed by color flow imaging. |
- sterile sleeve/plastic bag - acoustic gel
- sterile saline
- flow disturbances - gray scale - defects |
|
|
TCD capabilities:
Capable of detecting intracranial ____ & ________.
Can assess _____ circulation in known cases of severe carotid _______ or ________.
Can evaluate the __________, ____ and time course of vasoconstriction caused by _________ __________.
Useful in evaluating intracranial ____ ________.
Can be used to assess pts w/suspected _________ ___________. |
- stenoses - occlusions
- collateral - stenosis - occlusion
- onset - severity - subarachnoid hemorrhage
- arteriovenous malformations
- brain death |
|
|
Limitations of TCD:
Recent _________ ____ may eliminate the transorbital approach.
Some pts have __________ of the temporal bone making adequate penetration of the US wave impossible.
If performed w/o imaging, vessels may be incorrectly identified because of the lack of ___________ ______________. |
- eye surgery
- hyperostosis
- anatomic landmarks |
|
|
Pt positioning TCD:
Pt assumes comfortable _______ position.
Pt should understand that they must lie _____ and avoid ______ during the exam. |
- supine
- quietly - speaking |
|
|
Physics principles of TCD:
A TCD system usually uses a _____ pulsed Doppler w/spectrum analyzer.
The assumed angle of insonation is ______ degrees.
What are the 3 acoustic "windows?" |
2 MHz
0
- Transtemporal - Transorbital - Transforamenal
|
|
|
The transtemporal approach allows for what 3 views?
The transforamenal approach may also be referred to as the __________ approach.
A 4th window, the __________ may be used to evaluate the intracranial carotid artery but it is not used as frequently as the others. |
- Anterior - Middle - Posterior
- suboccipital
- submandibular |
|
|
The standard method of quantifying velocity is __________ or more commonly _________ (TAMV).
PSV measurements __________ utilized in this application. |
- Time-averaged maximum of the mean velocity - Time-averaged mean velocity ( TAMV)
- are not |
|
|
TCD technique:
A routine study beings w/a unilateral ________ approach to identify the __________, ________, _____, and most distal _________.
The _________ ________ approach is used to evaluate the ophthalmic artery and carotid siphon.
The preceding two steps are completed ___________. |
- transtemporal - MCA - ACA - PCA - ICA
- ipsilateral transorbital
- contralaterally |
|
|
The foramen magnum approach is then used to evaluate the intracranial _____ and _____ arteries.
Before CCA compression/oscillatio maneuvers are performed, the status of the _________ _____ must be evaluated w/duplex US.
Oscillation maneuvers are contraindicated in cases of __________ ______, high-grade stenosis, r _________ of the ICA, and in the presence of ______ _____ _____ formation.
|
- vertebral - basilar
- carotid arteries
- low bifurcation - occlusion - complicated atheromatous plaque |
|
|
TCD Compression technique:
Palpate the ______.
Apply slow _________ pressure.
Hold the compression for _____ _____ _____ and then slowly release pressure.
Note any changes in blood flow during the ___________ ___________.
|
- CCA
- downward
2-4 cardiac cycles
- compression maneuver |
|
|
Oscillation technique TCD:
Palpate the ______________.
Apply ____ of short, ______, _____ compressions
Note any ______ _____ transmitted during the maneuever. |
- CCA
- series - rapid - incomplete - oscillatory patterns |
|
|
MCA:
Window _____________
Depth ________
Direction _________
Velocity _______________
Angle _________________ |
Transtemporal
30-60 mm
Antegrade
55 +/- 12
Anterior & Superior |
|
|
Terminal ICA:
Window _____________
Depth ________
Direction _________
Velocity _______________
Angle _________________ |
Transtemporal
55-65 mm
Bidirectional
55 +/-
Anterior & Superior |
|
|
ACA:
Window _____________
Depth ________
Direction _________
Velocity _______________
Angle _________________ |
Transtemporal
60-80 mm
Retrograde
50 +/- 11
Anterior & Superior |
|
|
PCA:
Window _____________
Depth ________
Direction _________
Velocity _______________
Angle _________________ |
Transtemporal
60-70 mm
Antegrade
39 +/- 10
Posterior |
|
|
ICA:
Window _____________
Depth ________
Direction _________
Velocity _______________
Angle _________________ |
Transorbital
60-80 mm
Parasellar: antegrade, supraclinoid: retrograde, genu: both
47 +/- 14
Varies |
|
|
Ophthalmic:
Window _____________
Depth ________
Direction _________
Velocity _______________
Angle _________________ |
Transorbital
40-60 mm
Antegrade
38 +/- 10
Medial |
|
|
VA:
Window _____________
Depth ________
Direction _________
Velocity _______________
Angle _________________ |
Transforamenal
60-90 mm
Retrograde
38 +/- 10
Right & left of midline
|
|
|
BA:
Window _____________
Depth ________
Direction _________
Velocity _______________
Angle _________________ |
Transforamenal
80-120 mm
Retrograde
41 +/- 10
Midline |
|
|
The interpretation criteria incorporate the flow characteristics evident on spectral analysis:
D _____________ V _______________ T ________________- P __________________ S _________________ H _____________ R_________ of middle cerebral artery/ICA. |
direction velocity turbulent flow pulsatility systolic upstroke hemispheric ratio |
|
|
Crossover collateralization occurs when _______ flow is evident in the __________ _________ ________ artery.
This abnormality can be attributed to flow from the _________ __________ __________ artery via the __________ ___________ artery.
Increased velocities (_________) in the _________ anterior cerebral artery are also seen. (compare contralateral ACA w/contralateral MCA) |
- antegrade - ipsilateral anterior cerebral
- contralateral anterior cerebral - anterior communicating
> 150% - contralateral |
|
|
T or F:
An additional finding that confirms crossover collateralization is ipsilateral MCA flow velocities that increase w/contralateral compression of the CCA and that respond positively to contralateral oscillation maneuvers of the CCA. |
FALSE:
An additional finding that confirms crossover collateralization is ipsilateral MCA flow velocities that DIMINISH w/contralateral compression of the CCA and that respond positively to contralateral oscillation maneuvers of the CCA. |
|
|
External to Internal collateralization is evident when there is _____ flow in the _________ _________ artery.
This abnormality can be attributed to flow from the _____ branches and can be confirmed by noting _____, _____ or _____ of the arterial flow w/compression of ipsilateral ECA branches.
Decreased _____ and increased _____ in the ipsilateral ophthalmic artery may also be evident. |
- retrograde - ipsilateral ophthalmic
- ECA - reduction - obliteration - reversal
-pulsatility - velocity |
|
|
Posterior to anterior collateralization is evident when flow velocities in the ___________ _________ _________ artery exceed those of the ______ _____ _____ artery.
EX: (_____)
Increased flow velocities in the _____ _____ artery w/ipsilateral compression of the CCA is an additional finding that confirms patency of the ___________ __________ artery. |
- ipsilateral posterior cerebral - ipsilateral middle cerebral
> 125%
- posterior cerebral - posterior communicating |
|
|
Other factors that may alter intracranial blood flow:
age, sex, _____, blood gases, & __________ ______. |
- hematocrit - metabolic demand |
|
|
Dx of an _________ is difficult because of the technical limitations of the study.
It is most accurate in suspect _____ of the ____ and _____.
Criteria similar to other vessels:
_______ of Doppler signal, Low ______ _____ in the arterial segment just _____ to suspected ______, and evidence of ___________. |
- occlusion
- occlusions - ICA - MCA
- absence - diastolic component - proximal - occlusion - collateralization |
|
|
Although vasospasm can occur in other cerebral vessels, the dx of vasospasm is most accurate in the ______________ ____________ _________.
Serial recordings of this vessel's flow are necessary to document the __________ in velocities associated w/vasospasm. |
- Middle Cerebral Artery
- increased |
|
|
Normal hemispheric velocities are _____ w/a hemispheric ratio of __________.
The hemispheric ratio is calculated by dividing the _______ _____ _____ ____ of the MCA by the TAMV of the __________ _________ __________.
|
< 120 cm/s < 3
- time-averaged maximum velocity - distal extracranial ICA |
|
|
In an AVM, the arteries supplying the malformation usually have ________ systolic and diastolic velocities w/very ________ pulsatility indices.
In addition, __________ of flow in adjacent arteries is usually evident. |
- increased - low
- reduction |
|
|
TCD findings appear to correlate well w/ __________ ___________ arrest.
Changes in flow characteristics seem to follow the ________ of ________ _____ as it progresses through 6 stages.
|
- cerebral circulatory
- deterioration - cerebral perfusion
|
|
|
Brain death;
Initially the diastolic velocity _____ and the pulsatility index ________.
This patter progresses to the point at which EDV reaches _____, followed by a _________ of diastolic flow.
In the later stages, ______ flow develops, followed by a ______ velocity ______-______ waveform.
________ of flow is the final step of cerebral circulatory arrest. |
- decreases - increases
0 - reversal
- reverberatory - low - spiked-systolic
- Absence |
|
|
Intraoperative monitoring capabilities:
TCD allows for the identification of _______ abnormalities during many cerebrovascular and cardiovascular procedures, including ____ _____ and ______ _________.
Technique:
Continuous monitoring of the _______ ______ ______ blood flow requires the standard equipment along w/a _______ to stabilize the Doppler probe at the ________ window.
A ____ ______ is not necessary as the window is not in the surgical field.
|
- flow - carotid endarterectomy - cardiopulmonary bypass
- MCA - headset - transtemporal
- probe cover |
|
|
Intraoperative monitoring interpretation:
Significant decrease in the MCA flow velocities during the cross-clamping portion of the carotid endarterectomy may signal the need for ________.
Auditory signals related to ______ may lead the surgeon to alter operative technique. |
- shunting
- microemboli
|
|
|
Subclavian steal is a condition in which blood destined for the ___________ is shunted away from the _______ circulation because the ________ or _______ artery has a ________ ________ __________ or total occlusion _________ to the take-off of the _________ artery.
Blood flows ______ down the _______ artery in order to provide blood flow to the ___________. |
- brain - cerebral - subclavian - innominate - high grade stenosis - proximal - vertebral
- retrograde - vertebral - arm |
|
|
Are pts usually symptomatic?
Is subclavian steal more frequent on the right or left side?
There is a brachial BP difference of ______ or greater from one side to the other.
|
- No usually asymptomatic
- More frequent on the left side than the right
15-20 mmHG |
|
|
T or F:
In subclavian steal, pulses in the affected arm are decreased and arm claudication is common |
FALSE:
In subclavian steal, pulses in the affected arm are decreased BUT arm claudication IS RARE |
|
|
What is the normal resistance of the vertebral artery?
How does this change w/subclavian steal?
Why? |
- Normally low resistance
- Flow resistance increases
- Because it is feeding a higher-resistance bed |
|
|
Surgical tx for subclavian steal may include a ______ or ________.
With subclavian stenosis rather than occlusion, the character of blood flow in the ______ vertebral artery may be altered. |
- bypass graft - endarterectomy
- ipsilateral |
|
|
Temporal arteritis is __________ of the ___________ segment of the ________ _________ artery or its frontal and/or parietal branches.
Patients are _________, complaining of ____, tenderness on palpation of the _____ _________ ___________ artery or its branches and possibly ipsilateral ___________.
A duplex study can assist in dx but requires an ____________ _________ ____ w/a record of high accuracy as confirmed w/biopsy findings. |
- inflammation - distal - superficial temporal
- symptomatic - headaches - distal superficial temporal - blindness
- experienced vascular technologist |
|
|
Temporal arteritis:
B-mode findings may include visualization of a _______ segment of the vessel wall and an _____ _______ around the vessel wall secondary to ________.
Spectral analysis may document ______ flow at the area of the narrowing.
Medical tx includes ______ _______.
|
- narrowed - anechoic halo - edema
- accelerated
- steroid therapy (ex: prednisone) |
|
|
When B-mode findings and Doppler flow characteristics are abnormal and consistent w/temporal arteritis, the pt may not have to undergo a _______ of the temporal artery.
However, abnormal duplex findings may not be evident in the pt who has started _________ ______. |
- biopsy
- steroid therapy |
|
|
248
What would you conclude from this image? |
- The early systolic deceleration is consistent w/a proximal stenosis of the subclavian artery |
|
|
248
What type of flow is this?
What does it suggest? |
- bidirectional flow (to-and-fro)
- Progression of disease--flow in the ipsilateral vertebral artery may exhibit to-and-fro flow and progress further to complete flow reversal |
|
|
249 This image shows the _________ __________ around the vessel wall caused by _______ that is associated w/__________ _________ |
- anechoic halo - edema - temporal arteritis |
|
|
Arteriography type:
____________ injection
Digital _______ angiography, arterial |
- intraarterial
- subtraction |
|
|
Intraarterial injection is usually performed according to the ___________ technique in which a very thin _______ is inserted into an artery, fed into the arterial tree, and positioned for the injection of _____ _______ to obtain a radiographic image of that vessel and the ______ arterial system.
The most commonly used arteries are the _________ w/the _______ or brachial cannulated if necessary. |
- Seldinger - catheter - radiopaque dye - distal
- Common femoral - axillary |
|
|
252
Normal or abnormal? |
Normal: contrast medium completely fills the vessels |
|
|
252
Normal or abnormal? |
Abnormal: filing defect in the ICA |
|
|
Digital subtraction angiography (DSA) uses _______ ____ ____ ______ processing to detect small amts of the contrast medium that has been injected into the artery.
A rapid ________ _______ technique is used to expose the films _________ as the contrast agent moves through the vessel.
|
- real time digital video
- film changer - sequentially |
|
|
Following the removal of the catheter, pressure is applied to the puncture site and the pt is positioned supine for _______.
A closure device may be used and/or a variety of methods to maintain pressure on the insertion site to avoid _____ and/or _________ formation. |
- 2 to 6 hours
- hemorrhage - pseudoaneurysm |
|
|
Normal anatomy should appear on the films as the contrast medium ____ _________ the vessel.
Any deviation from normal such as a ____ _____ is evidence of an arterial abnormality.
|
- completely fills
- filling defect |
|
|
253
Angiography of the aortic arch and extracranial cerebrovasculature demonstrates _______ disease in a pt admitted because of CVA. |
- multiple |
|
|
253 |
253 |
|
|
253 |
253 |
|
|
254
Angiogram from pt w/asymptomatic carotid bruit. What is the irregularity? |
The absence of contrast agent (filling defect) reveals the irregularity of the plaque in the bulb and ICA. |
|
|
254
What is the irregularity displayed in this image? |
ICA w/FMD of the distal portion
- beaded characteristic |
|
|
255
Angiogram depicting a ________ _____ in the carotid bulb. Doppler peak flow velocities are reduced because of the ______ ________ state of this ______ lesion.
Would you expect to hear a bruit? |
- "string sign" - low flow - preocclusive
No---because the disease is so severe |
|
|
Percentage stenosis calculation---diameter reduction: calculated on basis of vessel diameter
_____________ / __________ - ________ |
diameter of residual lumen / diameter of true lumen -1 X 100
[ 1-(d/D)] x 100 |
|
|
Percentage stenosis calculation--area reduction; calculated assuming that lesion is symmetrical __________ / ________ - ______ |
square of residual lumen diameter / square of true lumen diameter -1 x 100
[1-(d^2/D^2)] x 100 |
|
|
50% Diameter reduction = to __________ area reduction |
75% |

