![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
139 Cards in this Set
- Front
- Back
|
Actinobacillosis (woody tongue) - Aetiology
|
A - Actinobacillus lignieresi (gram -ive coccobacilli)
|
|
|
Actinobacillosis (woody tongue) - Basic Pathogenesis |
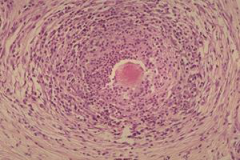
B - Trauma allows entry of organism which provokes pyogranulomatous inflammatory response centred on immune complexes ("club colonies") surrounding the bacteria
|
|
|
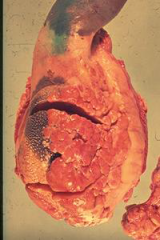
Actinobacillosis (woody tongue) - Clinical signs - Characteristic changes (gross and micro) |
C - excessive salivation, difficulty eating, visibly enlarged tongue that protrudes from the mouth. Tongue feels like wood due to extensive fibrosis
C - Grossly "sulfur granules", firm lesions |
|
|
Actinobacillosis (woody tongue) - Diagnosis - DDx |
D - culture and biopsy of the lesion
DDx - FMD, lumpy jaw (Actinomycosis) |
|
|
Actinobacillosis (woody tongue) - Species susceptible - Samples required - Possible sequelae |
Cattle (Sheep, Horses, Pigs, Dogs)
Pus from an abscess, biopsy
Lymphangitis and regional lyphadenitis
|
|
|
Severe Actinobacillosis (woody tongue) |
|
|
"Sulfur granules" from Actinobacillosis (woody tongue) |
|

|
Actinobacillosis (woody tongue) - facial swelling, lump on jaw - looks similar to lumpy jaw (Actinomycosis) |
|

|
Mild Actinobacillosis (woody tongue) |
|
|
Actimomycosis (lumpy jaw) - Aetiology |
Actinomyces bovis Gram +ive filamentous bacteria |
|
|
Actimomycosis (lumpy jaw) - Basic Pathogenesis |
Trauma allows entry into soft tissue of mouth Produces a pyogranulomatous mandibular and maxillary osteomyelitis |
|
|
Actimomycosis (lumpy jaw) - Clinical signs - Changes |
Lump on jaw, difficulty eating
"sulfur granules", extensive fibrosis, bone changes |
|
|
Actimomycosis (lumpy jaw) - Diagnosis - DDx |
Presumptive diagnosis often based on clinical signs, Gram stain of purulent material shows gram -ive "sulfur granules" (club-shaped rods and filaments)
FMD, woody tongue |
|
|
Actimomycosis (lumpy jaw) - Species - Samples - Sequelae |
Cattle
Purulent material
facial distortion, loose teeth, and dyspnea |
|

|
Actimomycosis (lumpy jaw) |
|
|
|
Actimomycosis (lumpy jaw) |
|
|
Adenovirus Enteritis - Species - Samples - Sequelae |
Cattle, pigs, horses (especially Arabians
Histology of SI epithelium
Weight loss, dehydration, death
|
|
|
Adenovirus Enteritis - Diagnosis - DDx |
Characteristic large nuclear inclusion bodies in endothelial cells
Other enteritis-causing diseases |
|
|
Adenovirus Enteritis - Aetiology |
Various Adenoviruses |
|
|
Adenovirus Enteritis - Basic Pathogenesis |
Endotheliotropic virus causes changes in epithelium of small intestines and sometimes rumen. |
|
|
Adenovirus Enteritis - Clinical signs - Changes |
Diarrhoea, weight loss, etc
Foci of necrotic rumenitis and locally extensive to diffuse pseudomembranous enteritis (espceially jejunum and ileum) seen in calves and feedlot cattle |
|
|
Bloat (rumenal tympany) - Aetiology |
Oesophageal obstruction; high legume consumption, oesophageal stenosis, vagal nerve damage |
|
|
Bloat (rumenal tympany) - Basic pathogenesis |
1° (frothy) bloat: legume proteins stabilise gas bubbles, producing a foam which is difficult to eructate and builds up.
2° (free gas) bloat: physical or functional defects in eructation cause buildup of gas.
Rumen pressure increases, mobility ceases and pressure on thoracic organs impairs cardiopulmonary function, leading to death |
|
|
Bloat (rumenal tympany) - Clinical signs - Changes |
Distended left paralumbar fossa, may be visible obstruction of throat, excess salivation
|
|
|
Bloat (rumenal tympany) - Diagnosis |
Ante mortem: Distended left paralumbar fossa, may be visible obstruction of throat, excess salivation, foam in rumen
Post mortem: distended rumen, foamy rumen contents, dark blood that clots poorly - anoxia, rupture of diaphragm, blanching of pleural viscera, "bloat line" on oesophagus, congestion of head and neck |
|
|
Bloat (rumenal tympany) - Species - Sequelae |
Ruminants
Death |
|

|
Bloat (rumenal tympany) Bloat line on oesophagus - where the congested cervical joins the pallid thoracic mucosa |
|
|
Bluetongue - Aetiology |
Bluetongue virus Arthropod-borne Orbivirus (Culicoides biting midges) |
|
|
Bluetongue - Basic pathogenesis |
Affects endothelial cells of small blood vessels causing microthrombi leading to ischaemic necrosis with ulceration of mouth cavity, oedema and haemorrhages. Cyanosis gives blue discolouration of tongue and mouth |
|
|
Bluetongue - Clinical signs - Changes |
Fever, lethargy, depression, oedema, cyanosis of mouth and tongue, oral ulceration, petechiae, lameness, tachypnoea, abortion or fetal abnormalities
vascular endothelial damage, resulting in changes to capillary permeability and subsequent intravascular coagulation. Edema, congestion, hemorrhage, inflammation, and necrosis
|
|
|
Bluetongue - Diagnosis - DDx |
Presumptive, especially in endemic areas (Africa, Middle East, parts of Asia, the USA, and recently, parts of Europe). Confirmed by haemorrhages in the wall of the base of the pulmonary artery and focal necrosis of papillary muscle of the left ventricle Virus isolation, PCR, ELISA, etc
Heartwater, pulpy kidney disease, Rift Valley fever
Not in NZ |
|
|
Bluetongue - Species - Samples - Sequelae |
Ruminants. Cattle and goats may be asymptomatic carriers
Blood in heparin flask, Serology
Death |
|

|
Bluetongue - Cyanosis and hyperemia of tongue - Petechiae of gingiva |
|

|
Bluetongue - Petechiae |
|

|
Bluetongue - Oral ulceration |
|

|
Bluetongue - Petechiae of coronary band and heel bulbs |
|

|
Bluetongue - Torticollis |
|
|
Bovine Papular Stomatitis - Aetiology |
Parapoxvirus related to pseudocowpox and milker's nodules |
|
|
Bovine Papular Stomatitis - Basic pathogenesis |
Disease of the nasolabium, oral cavity and
Proliferation of infected cells gives the characteristic papule which erodes to form circular ulcers. These may be surrounded by a zone of hyperaemia. |
|
|
Bovine Papular Stomatitis - Clinical signs - Changes |
Papules in oral cavity, nasolabium and oesophagus of calves, Ulceration
Proliferation of infected cells forming papules Hyperaemia Ulceration |
|
|
Bovine Papular Stomatitis - Diagnosis - DDx |
Clinical signs with laboratory confirmation
FMD, |
|
|
Bovine Papular Stomatitis - Species - Samples - Sequelae |
Cattle
Papules
Spontaneously resolve, although some may coalesce |
|
|
Bovine Viral Diarrhoea/Mucosal Disease - Aetiology |
Bovine viral diarrhea virus (BVDV) Pestivirus |
|
|
Bovine Viral Diarrhoea/Mucosal Disease - Basic pathogenesis |
PI animals reservoirs
Attacks epithelium, causing necrosis. As
Mutation of BVDV in PI animal causes mucosal disease. GI lesions more severe, |
|
|
Bovine Viral Diarrhoea/Mucosal Disease - Clinical signs - Changes |
BVD: Blunting of the conical papillae inside the lips and discrete erosions in the oral cavity and mucosa of the distal oesophagus. Ulceration, Enteritis, Diarrhoea
MD: Exudative skin lesions around perineum, base of the horns, interdigital skin and heels of the feet. GI lesions more severe, Death
|
|
|
Bovine Viral Diarrhoea/Mucosal Disease - Diagnosis - DDx |
Tentatively from disease history, clinical signs, and gross and microscopic lesions. Virus/antigen isolation by ELISA, IDEXX SNAP test on serum or ear-notch, necropsy
Rinderpest, MCF, FMD |
|
|
Bovine Viral Diarrhoea/Mucosal Disease - Species - Samples - Sequelae |
Cattle (lambs also)
Milk, blood, biopsy, nasal swab. At necropsy: spleen, lymph node, and ulcerated segments of the GI tract.
Persistent infection, Abortion, Decreased conception, Developmental defects, Immunosuppression, MD, Death |
|
|
Campylobacter Enteritis - Aetiology |
Campylobacter jejuni spiral, microaerobic gram-negative bacteria |
|
|
Campylobacter Enteritis - Basic pathogenesis |
Ingestion of contaminated food, etc Invades both epithelial cells and cells within the lamina propria causing enteritis |
|
|
Campylobacter Enteritis - Clinical signs - Changes |
Abdominal pain, fever, diarrhea, frank blood in feces, and inflammatory cells in feces
marked inflammation of the lamina propria, dominated by neutrophilic polymorphonuclear cells and mononuclear cells. Sloughing and ulceration of epithelium, oedema |
|
|
Campylobacter Enteritis - Diagnosis - DDx |
isolation of the organism on selective media under microaerophilic conditions
Other enteritis |
|
|
Campylobacter Enteritis - Species - Samples - Sequelae |
Dogs, cats, calves, sheep, pigs, ferrets, mink, monkeys, several species of laboratory animals, and people
Fresh fecal samples
Dehydration, death etc |
|
|
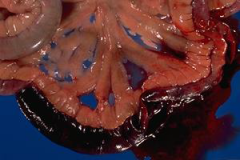
Clostridium spp. Enteritis - Aetiology |
Clostridium perfringens Type A - Colitis X of horses Type B & C - extensive haemorrhagic enteritis in lambs, calves and foals Type C - necrotic enteritis in piglets Type D - enterotoxaemia or pulpy-kidney disease in lambs |
|
|
Clostridium spp. Enteritis - Diagnosis - DDx |
Histopathology Isolation of Clostridium is only significant if clinical signs are present
Other enteritis |
|
|
Clostridium spp. Enteritis - Species - Samples - Sequelae |
Horses, lambs, calves, kids, foals, dogs
Histology
Death, dehydration etc |
|
|
Clostridium perfringens Enteritis in dogs - kennel dogs, highly sterile conditions - sudden death |
|
|
Coccidiosis - Aetiology |
Pigs, dogs, cats - Isospora spp Ruminants - Eimeria Cattle - E. zuernii, E bovis |
|
|
Coccidiosis - Clinical signs - Changes |
Diarrhoea, dehydration, acidosis
Enlarged mesenteric LNs, Enteritis Nodular proliferation of intestines, gametocytes in epithelial cells, ascites, oedema |
|
|
Coccidiosis - Diagnosis - DDx |
Oocysts in faeces
Other enteritis |
|
|
Coccidiosis - Basic pathogenesis |
E. zuernii - erosive to haemorrhagic typhlocolitis and proctitis E bovis - multifocal proliferative ileitis |
|
|
Contagious ecthyma (scabby mouth, orf) - Aetiology |
Parapoxvirus |
|
|
Contagious ecthyma (scabby mouth, orf) - Clinical signs - Changes |
proliferative, scabby lesions on the lips and face, with occasional extension to ulcerative lesions in the mouth
Intracytoplasmic, eosinophilic inclusion bodies |
|
|
Contagious ecthyma (scabby mouth, orf) - Diagnosis - DDx |
Intracytoplasmic, eosinophilic inclusion bodies or demonstration of virus by electronmicroscopy
FMD |
|
|
Coronavirus enteritis - Clinical signs - Changes |
Diarrhoea, dehydration, enteritis etc
necrosis of surface epithelium with severe atrophy of the villi. In dogs and cattle, crypts in the colon can also be affected |
|
|
Coronavirus enteritis - Important infections |
Transmissible gastroenteritis (TGE) in suckling pigs Porcine epidemic diarrhoea (PED) in piglets |
|
|
Coronavirus enteritis - Diagnosis |
ELISA test is available for testing for virus in faeces |
|
|
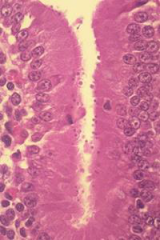
Cryptosporidium infections - Basic pathogenesis - Species |
Attach to the surface epithelial cells of the small intestinal villi to cause acute diarrhoea of varying severity in young calves, lambs, goat kids and foals. |
|
|
Cryptosporidium infection |
|

|
Cryptosporidium infection |
|
|
Distemper enteritis |
Morbillivirus
Enterorrhagia in puppies |
|
|
Enteritis |
Inflammation of intestines |
|
|
Typhlitis |
Inflammation of caecum |
|
|
Colitis |
Inflammation of colon |
|
|
Proctitis |
Inflammation of rectum |
|
|
Escherichia coli infection - Aetiology |
Important pathogenic strains are K99 (Ruminants) and K88 (pigs)
enterotoxigenic (ETEC), enteropathogenic (EPEC), enteroinvasive (EIEC), enterohaemorrhagic (EHEC), verotoxic (VTEC) |
|
|
Escherichia coli infection - Basic pathogenesis |
Enterotoxigenic (ETEC) - enteric colibacillosis in calves and piglets
Enteropathogenic (EPEC) - damage enterocytes and vascular endothelial cells
Enterohaemorrhagic (EHEC) - haemorrhagic enteritis in animals, haemolytic-uraemic syndrome in humans |
|
|
Escherichia coli infection - Changes |
Enterotoxigenic (ETEC) - mild - slight hyperaemia of the mucosa and watery contents
Enteropathogenic (EPEC) - characteristic histological lesion described as “attaching and effacing”, where large numbers of bacteria are seen to adhere to enterocytes |
|
|
Escherichia coli infection - Species - Sequelae |
Cattle, pigs - newborns
Secondary suppurative lesions (e.g. arthritis) elsewhere and/or septicaemia (colisepticaemia) and death. |
|
|
Foot-and-Mouth Disease - Aetiology |
Picornavirus |
|
|
Foot-and-Mouth Disease - Basic pathogenesis |
Viraemia, 4-5days vesicles develop in the mouth, interdigital skin, coronet, teats and vulva, and coalesce to form bullae which rupture to leave erosions and ulcers. Virus distributed through lymphatics to epithelium |
|
|
Foot-and-Mouth Disease - Clinical signs |
Anorexia, fever, Vesicles cause irritation In cattle young animals may die from myocarditis, mortality otherwise low. |
|
|
Foot-and-Mouth Disease - Diagnosis - DDx |
Inoculation onto susceptible tissue culture and ELISA
Clinically indistinguishable from Vesicular Stomatitis (cattle) and Vesicular Exanthema (pigs) Contagious ecthyma |
|
|
Foot-and-Mouth Disease - Species - Samples - Sequelae |
Cloven footed animals (pigs, cattle, sheep, goats)
Vesicular epithelium or fluid
Usually just loss of production, low mortality rate |
|
|
Conditions affecting the forestomachs - Foreign bodies |
Trichobezoars (hair balls) Phytobezoars (plant fibre balls) Miscellaneous foreign or plant materials associated with death from poisoning |
|
|
Conditions affecting the forestomachs - Rumenitis |
Kikuyu poisoning - superficial rumen necrosis, rumenitis, indigestion and death.
Grain overload syndrome - following the ingestion of large amounts of easily digestible carbohydrate to which the animal has not been accustomed. |
|
|
Vesicular Diseases - Differentials |
FMD - ruminants and pigs
Vesicular stomatitis - cattle, horses, pigs
Vesicular exanthema - pigs Swine vesicular disease - pigs
Furanocoumarin photodermatitis
Feline calicivirus - cats |
|
|
Thrush - Aetiology - Species |
Fungus Candida albicans, although probably not the primary pathogen
Often piglets |
|
|
Thrush - Basic pathogenesis |
Superficial inflammation of the oral and oesophageal stratified squamous epithelium. Build-up of excess epithelial debris, Prolonged antibiotic therapy may predispose
|
|
|
Thrush - Changes |
Whitish pseudomembrane on the affected areas made up of excessive, partly keratinised epithelium and exudate. Histologically epithelial hyperaemia and accumulation of dead or degenerate, partly keratinised cells superficially. Numerous hyphae may be seen within this |
|
|
Swine dysentery - Aetiology |
Brachyspira (Serpulina) hyodysenteriae Spirochaete bacteria |
|
|
Swine dysentery - Clinical signs - Changes/pathogenesis |
Diarrhoea, with mucus, blood or fibrin in
Bacteria invade the epithelial cells of the superficial colonic mucosa, causing necrosis and haemorrhage |
|
|
Swine dysentery - Diagnosis - Species |
Warthin-Starry silver staining is used in the histological diagnosis.
Weaned pigs |
|
|
Parapox infection in red deer |
proliferative / scabby, papular, erosive or ulcerative lesions in the oral cavity, on the lips, around the perineum and between the digits |
|
|
Parasitic gastroenteritis - Horses |
Draschia spp - focal granulomatous gastritis in horses
Bots (Gasterophilus) cause small areas of ulceration and granulomatous inflammation
Trichostrongylus axei - catarrhal gastritis, nodules, and ulceration when larvae emerge |
|
|
Parasitic gastroenteritis - Ruminants |
Haemonchus - anaemia and melaena
Ostertagia and Teladorsagia spp. - hyperplasia and metaplasia of the glandular epithelium |
|
|
Parasitic gastroenteritis - Pigs |
Ascarids not in stomach but in intestines - obstructive
Hyostrongylus rubidus - catarrhal gastritis, nodules, ulceration |
|
|
Parasitic gastroenteritis - cats |
Ollulanus tricuspis - unthriftiness, vomiting and gastritis in cats, pigs |
|
|
Oedema disease - Basic pathogenesis |
Endothelial damage results in oedema of the eyelids, nose, ears, larynx, greater curvature of the stomach and colonic wall, possible infarcts in the gastric wall, ascites with fibrin strands between abdominal viscera, as well as hydrothorax and hydropericardium with a fibrin clot. |
|
|
Oedema Disease - Clinical signs - Changes |
Nervous signs
Fibrinoid necrosis of small arteries is seen in Foci of encephalomalacia, frequently bilaterally symmetrical, are often present in the brain stem |
|
|
Oedema disease - Aetiology - Species |
cytotoxigenic (VTEC) E. coli
Pigs, recently weaned |
|
|
Rotavirus infection - Species
|
Wide range of mammals and birds with species specific subtypes
Tend to affect newborns |
|
|
Rotavirus infection - Changes - Diagnosis |
Necrosis of surface epithelium of the villi and consequent villus atrophy
Commonly complicated by coronavirus, cryptosporidia, enterotoxic E. coli, coccidiosis, etc.
Diagnosis is by an ELISA test on faeces. |
|
|
Parvovirus - Basic pathogenesis |
Viruses replicate in the rapidly proliferating cells of the small intestinal crypts causing necrosis. severe atrophy and near denudation of villi. |
|
|
Parvovirus - Changes |
Intestinal crypt cell necrosis and collapse of the mucosa with crypt “abscesses” create pathognomonic histological lesions. Necrosis of proliferating thymic and haemopoietic tissue in the bone marrow resulting in a panleukopenia, particularly in cats |
|
|
Parvovirus - Species - Samples - Sequelae |
Dogs and cats
Histo
Cerebellar hypoplasia in kittens infected in utero, Secondary infection, myocarditis |
|
|
Salmonella spp infections - Aetiology - Species |
Horses - S. Typhimurium (commonly nosocomial)
Cattle - S. Typhimurium and S. Hindmarsh
Sheep - S. Typhimurium, S. Hindmarsh and S. Brandenburg
Pigs - S. Typhimurium and S. Choleraesuis |
|
|
Salmonella spp infections - Basic pathogenesis |
Young animals are more likely to suffer generalised or septicaemic infections.
Fibrinonecrotic enterocolitis in horses, with pneumonia, polyarthritis, meningoencephalitis and terminal septicaemia
Enteritis and septicaemia in calves, older cattle more sporadic with lesions being fibrinonecrotic enteritis, typhlitis and colitis
Fibrinonecrotic enteritis and septicaemia in mature sheep
In pigs, acute or chronic enterocolitis, septicaemia and lesions of DIC |
|
|
Salmonella spp infections - Changes |
Depression, fever, anorexia, diarrhoea, abdominal pain
"button ulcers" in pigs Fibrinonecrotic lesions
Pneumonia, polyarthritis, meningoencephalitis, septicaemia in foals.
|
|
|
Salmonella spp infections - Diagnosis - Samples |
Difficult to diagnose, often need multiple samples
Based on clinical signs, severe neutropenia, and isolation of salmonellae from feces, blood, or tissues.
|
|
|
Traumatic Reticuloperitonitis - Aetiology - Basic pathogenesis |
Ingestion of nails, wire etc which get lodged in the cranial wall of the reticulum by contractile and gravitational forces, and may penetrate through.
|
|
|
Traumatic Reticuloperitonitis - Clinical signs - Changes |
Often no clinical signs until CHF occurs
Localised fibrinous, suppurative or granulomatous peritonitis. May be perforation, abscessation, haemorrhage, vagal nerve damage |
|
|
Traumatic Reticuloperitonitis - Species - Sequelae |
Cattle
Traumatic reticulopericarditis leading to restrictive CHF Pleurisy, pneumonia Vagal nerve damage leads to atony of rumen and reticulum |
|
|
Kikuyu Poisoning |
Superficial rumen necrosis, rumenitis, indigestion and death
Lesions of necrosis and inflammation of the wall of the forestomach may be seen microscopically
Cattle |
|
|
Grain Overload Syndrome - Aetiology |
Following the ingestion of large amounts of easily digestible carbohydrate to which the animal has not been accustomed - introduction to grain feeding - accidental access to grain, apples, kiwifruit etc |
|
|
Grain Overload Syndrome - Basic pathogenesis |
Initial increase in volatile fatty acids is followed by an increase in lactic acid as the flora changes from cellulytic to amylolytic. Rumen pH drops below pH5 (death of rumen protozoa).
This causes: - absorption of FA's and acidosis - increase in intraruminal osmotic pressure leading to loss of fluid, dehydration and haemoconcentration |
|
|
Grain Overload Syndrome - Diagnosis |
Depends on the amount of fermentable grain/apples/ etc. relative to the amount expected (in the case of accidental feeding) and rumen pH lower than pH5. Microscopic examination of rumen contents fails to show motile protozoa Histopathology retrospectively. |
|
|
Grain Overload Syndrome - Sequelae |
- frothy bloat
|
|
|
Hog Cholera (Classical Swine Fever) - Aetiology |
Pestivirus |
|
|
Hog Cholera (Classical Swine Fever) - Changes |
Haemorrhages, especially in the lymph nodes and kidneys (“turkey’s egg”) and elsewhere, are characteristic. Multiple splenic infarcts. In the intestinal tract, catarrhal, fibrinous or haemorrhagic inflammation. “button ulcers” in the caecum and proximal colon |
|
|
Hog Cholera (Classical Swine Fever) - DDx |
Salmonella Choleraesuis - "button ulcers" |
|
|
Salmonellosis - Changes |
Fibrin cast in intestines Catarrhal enteritis Fibrinonecrotic enteritis/typhlocolitis/abomasitis
Some cases have disseminate foci of necrosis in liver and spleen Splenomegaly |
|
|
Salmonellosis - DDx |
Enteric listeriosis in sheep
Hog Cholera - "button ulcers" |
|
|
Yersiniosis - Aetiology - Species |
Yersinia pseudotuberculosis - cattle, sheep, goats, deer
Yersinia enterocolitica - goats, sheep, pigs |
|
|
Yersiniosis - Basic pathogenesis |
Y. pseudotuberculosis - Cold, wet, wintery conditions. Gastroenterocolitis +/ abortion
Y. enterocolitica - Enterocolitis |
|
|
Yersiniosis - Clinical signs - Changes |
Often found dead with blood-stained faeces
Marked haemorrhagic gastroenteritis, particularly affecting the small intestine. Mesenteric lymph nodes may be congested and swollen. |
|
|
Yersiniosis - Diagnosis |
Histopathology - colonies of Gram-negative bacteria (dark blue) and aggregates of neutrophils are visible in the lamina propria of the superficial mucosa and on the surface of the necrotic debris |
|
|
Johne's Disease - Aetiology - Species |
Mycobacterium avium subspecies paratuberculosis
Mature cattle, sheep, goats; young deer |
|
|
Johne's Disease - Basic pathogenesis |
Long incubation period
|
|
|
Johne's Disease - Clinical signs - Changes |
Diarrhoea (often projectile) and wasting
Mainly ileum, also jejunum, caecum, proximal colon. Granulomatous infection - Enlarged ileocaecal lymph nodes, sometimes with focal necrosis in deer and goats |
|
|
Johne's Disease - Diagnosis - Samples |
Ziehl-Neelsen stain for acid-fast bacteria
Faecal smear, Histology |
|
|
Listeria enteritis - Aetiology - Species |
Listeria monocytogenes
Sheep, cattle |
|
|
Listeria enteritis - Basic pathogenesis |
Animals fed of mouldy baleage/silage Abomasitis, enteritis and typhlocolitis Meningoencephalitis, Septicaemia, abortion |
|
|
Listeria enteritis - Diagnosis - DDx |
Culture of bacteria
Salmonellosis |
|
|
Lawsonia intracellularis infection - General |
Porcine intestinal adenomatosis (PIA) complex
Cerebriform appearance of lower SI (ileum)
Controlled by feed additives
|
|
|
Lawsonia intracellularis infection - Forms |
Thickened, folded mucosa with adenomatous appearance
Necrotic ileitis
Proliferative haemorrhagic enteropathy |
|
|
Lawsonia intracellularis infection - Diagnosis |
Warthin-Starry silver stain on epithelium, showing intracellular comma-shaped bacteria |
|
|
Oral Necrobacillosis - Aetiology - Species |
Fusobacterium necrophorum Calf Diphtheria
|
|
|
Oral Necrobacillosis - Basic pathogenesis - Changes - Diagnosis |
Usually secondary to previous mucosal damage Predisposing factors include: trauma, IBR, BVD or papular stomatitis infection
Lesions are large well-demarcated, yellow-grey dry areas of coagulative necrosis surrounded by a zone of hyperaemia.
Gross lesions normally diagnostic, organism can be seen in smears. |
|
|
Rhodococcus equi colitis - Changes |
Multifocal pyogranulomatous pneumonia
Ulcerative typhlocolitis - necrosis of Peyer's patches and ulceration in foals Mesenteric lymph nodes may be oedematous with necrotic or purulent foci
Histologic lesions are characterised by pyogranulomatous |

