![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
27 Cards in this Set
- Front
- Back
- 3rd side (hint)
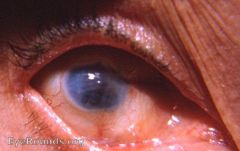
What is a shrunken, non-functional eye that results from severe ocular disease, inflammation, or injury
|
Phthisis bulbi
|
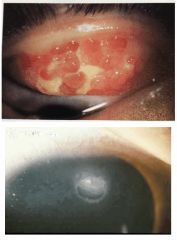
Pt presented with a ton of corneal clouding and edema. It was a corneal transplant with micro punture
|
|
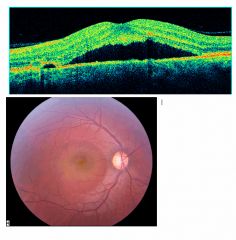
This condition appears to occur when fluid leaks from the choroid into the subretinal space through a defect in the RPE. This results in localized elevation and detachment of the retina. As the macular is involved in more than two-thirds of cases, central vision is usually affected
Symptoms: Blurred vision, micropsia and metamorphopsia DDx? Tx? |
Central serous chorioretinopathy
DDx: AMD, optic nereve head pit (with retinal detachment), rhegmatogenous RD, choroidal neo, choroidal tumors Tx: Fluorescein angiography (smokestack pattern). Condition is usually self limiting and most pts will recover to near-normal acuity in 3 mos. Laser can also be used in Tx when: serous detachment persisting for longer than 3 mos or recurance |
Pt was a young guy who saw perfect out of his left eye but had severe central vision loss out of his right.
|
|
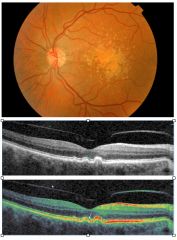
What is subretinal pale yellow deposits located mainly in the posterior pole area?
DDx? Tx? |
AMD - Dry
DDx: Stargardt disease Tx: There are no available therapies for AMD that restore VA's. Ways to reduce progression: Pts should be encouraged consume fruit on a daily basis and give up smoking. Also taking AREDS (Ocuvite) also helps. F/U annually, but pts are encouraged to areturn immediately if signs of reduced vision or distortion are noted. Give pts an Amsler grid for home use and self assessment |
|
|
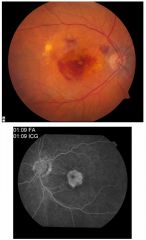
CNV, other exudative maculopathy, or geographic atrophic maculopathy in one or both eyes, sudden ,severe, central vision loss
DDx? Tx? |
AMD - Wet
DDx: Vascular occlusive disease or DR Tx: There are no available therapies for AMD that are proben to restore the pts visual acuity. Advise the pt to consume more fruit, quit smoking and take Ocuvite Fluorescein angiography is used to diagnose CNV and to direct tx The two established tx that may satbilize vision and limit severe visual loss in pts with CNV are argon later photocoagulation and, PDT with visudine Can also tx exudative AMD with Lucentis or Avastin |
|
|

A unilateral red eye, no discharge or ocular pain and vision is unaffected.
Signs: clear ring around the limbus and able to locate the posterior limit to the hemorrhage. May be associated eyelid bruising DDx? Tx? |
Sub-Conjunctival Hemorrhage (ecchymosis)
DDx: Conjunctivitis; preseptal cellulitis; AACG; iritis; uveitis Tx: Benign condition requiring no tx. The condition should resolve in 1 to 2 weeks. Discourage use of aspirin unless on medical instruction Tx symptoms. Cold compress for 24 hrs to reduce bleeding then hot compresses for 3 to 5 day to assist resolution. AT if there is ocular irritation. Pt told to RTC if not substantial resolution within 2 weeks |
|
|

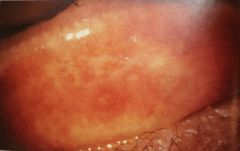
Symptoms are non-specific with ocular surface irritation and FB sensation, photophobia, and slight blurring of vision. Possible increased lacrimation or even a mucus discharge. Signs occur at three sights: marginal superior tarsal conj, superior bulbar conj and superior cornea and limbus. The marginal superior tarsal conj is inflamed with a 2-3 mm strip of velvety papillary reaction parallel to the lid margin. Superficial epithelial punctate staining with lissamine green at all three sites.
Is a rare inflammatory condition usually affecting middle-aged women. DDx? Tx? |
Superior Limbic Keratoconjunctivits (SLK)
DDx: Terrien's marginal degerneration; trachoma Tx: Pts with SLK should be examined for thyroid dysfunction with T3, T4, and TSH. Condition could also be due to mechanical rubbing of the superior bulbar and lid. AT, Soft steroid qid for several weeks |
|
|

Due to a deposition of a substance (usually a drug) from the tear film or limbal vasculature into the corneal epithelium.
Pt is usually asymptomatic. You will usually see a summetrical, bilateral, grayish, or golden corneal deposit in a swiriling pattern DDx? Tx? |
Vortex keratopathy
DDx: Corneal dystrophies, degenerations and depositions; Iron lines (Fleischer ring, Stocker's line, Hudson-Stahli line, Hemosiderosis); chlorpromazine drug Tx: routine fundus exam may detect retinal changes, especially pigmentary. Modify the level of meds if symptoms or signs require it, and if the management of the systemic condition allows it. With hydroxychloroquine, any retinal changes or the appearance of scotoma, night blindness, or similar requires immeditae discontinuation of the drug on the advice of the prescribing clinician. These pts should not subsequently receive any pharmacologically similar drug. |
|
|
Its a potentially severe ocular surface allergic condition seen exclusively in children and young adults, more common in boys.
Symptoms: Intense bilateral itch, intermittent redness, increased lacrimation, and FB sensation. Mucous strands are common in inferior fornix. Slight ptosis may develop Signs: Diffuse hyperemia with a velvety, papillary conjunctivitis. Large papillae with a cobblestone appearance in superior palpebral conj. In the active form Tranta's dots (small chalky white accumulations of eosinophils) may be seen. An ulcer may be present that stains intensely, DDx? Tx? |
Vernal Keratoconjunctivitis (VKC)
DDx: Atopic keratoconjunctivitis (AKC); GPC Tx: Need to primarily tx the corneal disease (ulcer), not the conjunctivitis. It is not necessary to fully settle any conjunctival inflammation, as to do so may involve the excessive use of topical steroids Allergen avoidance is an important tx in VKC Use mast-cell stabilizers are the mainstay of tx. They also need to be taken prophylactically 3-4 times a day on a regular basis, especially during allergy season |
|
|
Its a serious sight-threatening bilateral allergic disease that eventually leads to extensive conj scarring. Associated with eczema, asthma, and hay fever.
Symptoms: Itch, blurry vision, and a mucoid discharge Signs: Lids are thickened, macerated, and fissured as well as bleph. The conj is variably affected with anything from a hyperemic, flattened velvety appearance with papillae. DDx? Tx? |
Atopic Keratoconjunctivitis (AKC)
The loss of sight comes from the scarring through liberation of pro0inflammatory cellular products that have a directly toxic effect. There may be associated signs of keratoconus that possibly develops secondary to the extensive eye rubbing DDx: VKC and trachoma Tx: Allergen avoidance. Therapeutics include antihistamine/mast-cell stabilizers (used throughout the year), NSAIDS (Acular), steroids for acute flare ups. Advise pts to avoid eye rubbing |
|
|
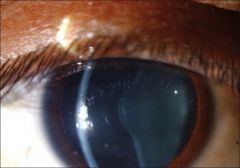
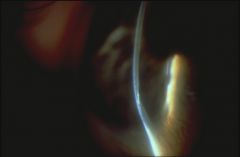
What syndrome can cause this? What should you get run if you see this in a pt?
|
Alport syndrome (genetic nephritis)-Lenticonus
Have pt sent in for a kidney evaluation |
|
|

It is caused by an infection of V1 with the herpes vericella zoster virus (VZV).
Symptoms: the onset of the rash is often preceded by a viral prodrome and a burning or tingling sensation affecting the skin around the eye and forehead. Photophobia, blurring of vision , and increased lacrimation may occur to a varying degree. Following resolution of the rash, post-herpetic neuralgia frequently occurs. Signs: Rash that respects the midline of the face and affects V1 and sometimes V2. Corneal sensitivity if reduced. Early signs of ocular involvement include aqueous cell and flare, corneal microdendrites and conjunctivitis. DDx? Tx? |
Herpes Zoster Ophthalmicus (HZO)
DDx: HSK Tx: HZO is contagious during the vesicular stage. Pts should be warned about contact with others who have not had chicken pox or have not been immunized Acute Tx: Tx with oral antiviral agents (valaciclovir-1g PO tds for 7 days or farmciclovir-250 mg for 7 days ... no longer acyclovir due to its short half-lives) if the pt presents within 72 hrs of the onset of the rash Long-Term Tx: Topical corticosteroids, tear supplements, and anti-glaucoma meds are all used in the management of long-term complications |
|
|
This has precipitations from the tear film which leads to a subepithelial, and anterior corneal stromal opacity,
Symptoms: Blurred vision, glare, surface irritation. May be asymptomatic initally Signs: A diffuse peripheral interpalpebral, subepithelial, gray opacity that starts near the lumbus. It progresses across the inferior cornea being narrowest centrally. DDx? Tx? |
Band Keratopathy
DDx: Rarely confused with anything else Tx: AT and/or BCL Surgery: indicated for improvement in vision, or ocular comfort. Large chips of calcium and be removed via forcepts. The rest can be removed either by a combination of debridement and chelation or with excimer laser phtotherapeutic keartectomy PTK |
|
|
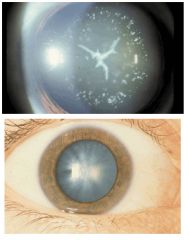
What causes these cataracts?
|
DM
|
|
|
|
This affects the corneal epithelium leading to characteristic cystic and whorl-like opacities.
Signs: epithelial changes bilateral Symptoms: Symptom-free usually but 10% of pts will have corneal erosions DDx? Tx? |
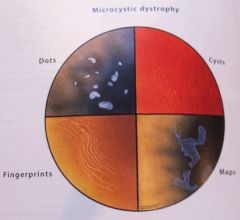
Epithelial basement membrane dystrophy (EBMD)
Four epithelial changes that occur in this condition-Microcycsts, dots, maps, and fingerprints DDx: Meesmann's dystrophy; Reis-Buckler's dystrophy; corneal epithelial microcystic edema; corneal scarring Tx: Topical lubricants, BCL with a prophylactic topical antibiotic, debridement of the visual axis, superficial micropuncture, PTK |
|
|
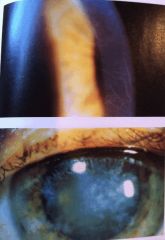
This condition refers to an active inflammatory process within the corneal stroma. The causes are bacteria, HSV and HZV, and Cogan's syndrome
Signs: Active form: Stromal inflammation with edema, corneal opacitites and frequently stromal vascularization Resolve/inactive: corneal opacification, thinning, and "ghost vessels" Both acquired and congenital syphillis can lead to an acute episode of this condition bilaterally. There is associated iris atrophy with a typical flattened featureless iris characteristic Argyll-Robinson pupil. Symptoms: Photophobia, blurring vision, ocular ache, and increased lacrimation. Condition is usually bilateral. DDx? Tx? |
Interstitial keratitis (IK)
DDx: Old corneal injury; chemical burn; old stromal necrotic HSK; trachoma Tx: Urgent: Cogan's syndrome can rapidly lead to permanent hearing loss and even death from large vessel vascular disease so send pt to an ear, nose, and throat specialist and a physician Active IK pts should be investigated extensively for an underlying cause of the disease - VDRL, FTA-ABS, ESR, Lyme disease, CXR, Mantousx test, TB Tx with a topical corticosteroid (Pred Forte) |
|
|

This condition presents with swelling of the anterior portion of the optic nerve in association with visual disturbance, and may relate to occlusion of the short posterior ciliary arteries. Occurs mostly in pt >45 yrs old
Symptoms: Sudden, painless unilateral loss of vision with no preceding visual symptoms Signs: VA loss, RAPD, inferior VF is affected, segmental or generalized pale disc swelling with peripapillary flame-shaped hemorrhages DDx? Tx? |
Non-arteritic ischemic optic neuropathy (NAION)
DDx: AION; optic neuritis (papillitis); CRVO, optic nerve tumor; HR Tx: Urgent: Immediate ESR and CRP to r/o GCA FA may be helpful when the diagnosis is unclear Baby asprin can be taken long-term to protect against involvement of the second eye Approx 20-30% of pts experience mild improvement in vision |
|
|

This condition is the most common vasculitis in humans. It occurs due to granulomatous inflammation with disruption of the internal elastic lamina.
Signs: RAPD, VF defects usually altitudinal or central. The optic disc first becomes pale and swollen, often with flam-shaped hemorrhages at the margin. There may also be signs of a CRAO with a cherry red spot at the foveola. At first the optic disc first becomes pale and swollen. Symptoms: Sudden painless, monocular and severe visual loss. Systemic symptoms often precede ocular symptoms, and include anorexia, fever and lowered mood. Scalp tenderness and headache are common. DDx? Tx? |
Arteritic Ischemic Optic Neuropathy (AION, GCA, temporal arteritis)
DDx: NAION, Optic neuritis, CRAO, CRVO Tx: Urgent: CGA is a medical emergency Blood Tests: Urgent ESR and CRP Meds: IV corticosteroid Surgery: Temporal artery biopsy |
|
|

This condition is a superficial corneal inflammatory condition of unknown etiology. It usually affects young adults and typically follows a relapsing course affecting both eyes
Symptoms: Pt complains of recurrent episodes of ocular surface irritation and burning that fluctuates over time. Also pt complains of photophobia. Signs:Multiple, grouped, raised epithelial lesions, probably infliltrates. Have a stuck on appearance and are scattered across the whole of the epithelium. They have a typical central dense area surrounded by a less dense area termed an "areola". The disease is usually bilateral with no A/C reaction, and the eye is usually white and quiet. DDx? Tx? |
Thygeson's superficial punctate keratopathy
DDx: Other causes of SPK, including DE< bleph, toxicity, and Molluscum contagiosum, epidemic keratoconjunctivitis, adult inclusion conjunctivitis (Chlamydial conjunctivitis) Tx: AT Therapeutics: Moderate-strength topical steroid for an acute attack followed by maintenance therapy with a weak topical steroid |
|
|

This condition is a rare and frequently misdiagnosed condition capable of leading to significant upper eyelid laxity and conjunctival and cornela damage. If is highly associated with sleep apnea and typically affects obese middle-aged men.
Symptoms: The affected eye is gritty and sore along with blurring vision and associated increased lacrimation. Symptoms are usually chronic and fluctuate over time. Signs: Lash ptosis. The upper lid usually displays marked horizontal laxity especially affecting the medial canthal tendon. Cornela complications include: superior SPK, filamentary keratopathy, and peripheral pannus formation. DDx? Tx? |
Floppy eyelid syndrome
DDx: Rosacea keratitis, DES, chronic canaliculitis, crhonic Dacryocystitis, Toxic epithelipathy Tx: The floppy eyelid syndrome should be brought under good control prior to corneal graft sx if there is associated keratoconus Sleep laboratory investigations Non-Drug Tx: Tx with nasal continuous positive airway pressure (CPAP). Weight loss, shield at night to prevent rubbing and eversion of the lid, lubricant ointments and taping the lids at night. Sx: If tx is insufficient, a horizontal lid-shortening procedure prevents spontaneous eyelid eversion. You need to tx the underlying cause... Sleep apnea |
|
|
This condition is a rare peripheral corneal thinning of unknown etiology. The thinning leads to corneal stromal relaxation, resulting in induced irregular astigmatism. Common in men >30.
Symptoms: Pts complain of slowly deteriorating vision or the need to progressively change their spectacles with increasing astigmatic correction. Both eyes are usually affected. Signs: Signs are usually slowly progressive over years. Thinning usually occurs superiorly first and sometimes also inferiorly. The initial lesions are fine, white, subepithelial, and paralimbal. These coalesce over time, and the affected cornea begins to thin. A superficial pannus forms, with a whitish, sclerotic area on the central edge of the involved cornea. This involvement then spreads around the limbus. At this stage pseudopterygia often develop. As the process progresses the degree of astigmatism increases (10-15 diopters). DDx? Tx? |
Terrien's marginal degeneration
DDx: Pellucid, SLK, limbal HSK, senile peripheral cornea furrow, peripheral ulcerative keratitis Tx: Get a topography Can fit pt with rigid gas-permeable Can tx recurrent attacks of minor inflammation Sx: if the induced astigmatism is sufficiently marked such that spectacle and contact lens correction is unsuccessful, surgical intervention is required- peripheral, crescentic, inlay lamellar corneal or corneoscleral graft |
|
|

This condition is a conjunctival and corneal inflammatory disease that predominantly affects children. The etiology is thought to be a hypersensitivity reaction to bacterial antigens. The two main conditions associated with this disease are staph blepharitis and TB.
Symptoms: Photophobia and increased lacrimation. This vision is often slightly blurred from the increased tearing and secondary blepharospasm may occur. Signs: It develops at the limbus or on the paralimbal conj. It's a small, rased pink-white nodule surrounded by hyperemic conj. Over time these nodules may migrate centrall onto the corneal. DDx? Tx? |
Phlyctenulosis
DDx: Marginal keratitis. microbial keratitis, pyogenic granuloma, pingueculum Tx: If concern that the phlycten is caused by TB referral for a CXR, Mantoux test, and sputum cultures. Theraputics: Topical corticosteroids and a broad-spectrum antibiotic with good staph coverage. These are administered qid for 2-4 weeks |
|
|
|
This condition primarily affects women and begins usually after menopause. It is an autoimmune rheumatic disease. It is associated with increased levels in cerebrospinal fluid and interleukin 1 antagonists.
Symptoms/Signs: General dryness (mouth, rheumatoid arthritis, eyes, skin, nose etc). Blood tests to run? Other ophthalmic tests to run? Tx? |
Sjogren's Syndrome
ANA and rh - Schirmer's test (production of tears - less than 5 mm is indicative of Sjorgren's) - SLE of ocular surface Tx is generally symptomatic and supportive since there is no know cure. AT and punctal plugs, Restasis or a mild steroid |
|
|
|
This condition usually occurs at work or by accident.
Symptoms/Signs: Immediate pain, redness, epiphora, and blurring of vision. Usually the damage is worse inferiorly due to gravity and protective nature of the upper lid Grading Scale? Tx? |
Chemical Burn
Grading: Grade 1: clear corneal stroma and no limbal ischemia Grade 2: Corneal haze but less then 1/3 limbal ischemia Grade 3: Corneal haze blurring iris detail with 1/3 to 1/2 limbal ischemia Grade 4: Opaque cornea with more than 1/2 limbal ischemia Tx: Initial Tx- Grades 1 and 2 use a topical steroid and broad-spectrum antibiotic (chloramphenicol qid) until the epithelium heals Grade 3 and 4: Medical emergency (early tx is essential) Tx - qh with - topical unpreserved - corticosteroids - homatropine 2% bid - chloramphenicol tds - sodium citrate 10 % q2hs - sodium ascorbate 10% q2hs Taper drops as the epithelium begins to heal Long term Tx: Corneal grafts, amniotic membrane transplants, tarsorhaphies, and limbal stem cell transplants have been tried with varying success. |
|
|
|
What is a condition that is an occurrence of chronic bronchitis or emphysema in which the airways become narrowed? Triggers can be things such as noxious particles or gas, most commonly from tobacco smoke which triggers an abnormal inflammatory response in the lung
|
COPD
|
|
|
|
What is a type of cancer of the blood or bone marrow characterized by an abnormal increase of immature white blood cells?
|
Leukemia
|
|
|
|
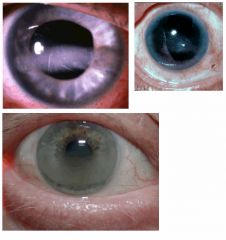
What is a condition that refers to the prescence of blood within the anterior chamber. Usually occurs secondary to blunt trauma or following recent iris surgery but can also occur spontaneously in pts with rubeosis iridis?
This condition is usually associated with acute glaucoma, damage to other intraocular and periocular structures. Symptoms: Blurred vision usually worse upon wakening. If there is associated rise in IOP there may be a dull ache in and around the eye. Signs: The AC blood is usually both circulating within the aqueous humor and settled. Irregular or dilated pupil, and signs of sphincter rupture with a tear at the pupil margin. Angle recession Tx? |
Hyphema
Tx: Pts with a hyphema involving less than one-half the AC should be reviewed in several days to check the IOP. Pts with a hyphema involving greater than one half the AC need to be reviewed daily intil the hyphema has substantiall resolved.Pts should be advised to present immediately if they have symptoms of a rebleed with decreased vision or ocular ache. Asprin and other NSAIDS should be avoided. Test blacks for sicle cell You can tx the pt with homatropine tid or with atropine to prevent excessive iris movement. Tx any pressure rise with topical anti glaucoma meds. |
|
|
|
This condition is a proliferation of predominantly collagenous tissue on the ILM. It varies widely in severity and appearance and form part of a continuum of conditions such as vitreomacular traction syndrome and macular holes. Found usually in people over 50.
Symptoms: Mild-to-moderate blurring of vision Signs: May glisten if thin. Is easier to see with a red free illumination. If thicker wil have a yellow-white or grey appearance. If severe it is usually associated with macular pathology such as CME, disturbance of the RPE or local retinal detachment DDx? Tx? |
Epiretinal membrane (macular pucker, cellohane maculopathy)
DDx: Macular edema, macular hole, PVD, vireomacular traction syndrome Tx: If pt is asymptomatic then they should be followed and warned to present if they note any change in their visual status. You can give a them an amsler grid. Perform an OCT to assess changes. If the condition is too rough then you can do a macular peel. |
|

