![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
227 Cards in this Set
- Front
- Back
|
the force that stretches the myocardium prior to contraction is called what?
|
preload
|
|
|
what is preload?
|
the force that stretches the myocardium prior to contraction
|
|
|
how does SV change with preload?
|
↑preload → ↑SV
|
|
|
what conceptually is an estimate of preload?
|
estimated by end-diastolic volume or end-diastolic pressure
|
|
|
the forces that oppose ventricular ejection are called what?
|
afterload
|
|
|
how does SV change with afterload?
|
↑afterload → ↓SV
|
|
|
how can afterload be modified pharmacologically?
|
by altering the PVR
|
|
|
what component of afterload can give you an estimate of the peripheral vascular resistance (PVR)
|
aortic pressure
|
|
|
the intrinsic, load-independent ability of cardiac muscle to shorten; or "the strength of the myocardium" is called what?
|
contractility
|
|
|
what is contractility?
|
the intrinsic, load-independent ability of cardiac muscle to shorten; or "the strength of the myocardium"
|
|
|
how does SV change with contractility?
|
↑contractility→ ↑SV
|
|
|
how do you calculate cardiac output?
|
CO = HR (bpm) x SV (vol/beat)
|
|
|
define heart failure
|
a syndrome of clinical signs that results from impaired emptying or filling of the heart
|
|
|
how does heart failure relate to heart disease?
|
heart disease can cause heart failure, but so can other things
|
|
|
what is the prognosis for heart failure?
|
heart failure is terminal unless the cause can be eliminated
|
|
|
what is the most common clinical sign of LV congestive heart failure?
|
pulmonary edema
|
|
|
what is the most common clinical sign of RV congestive heart failure?
|
ascites
|
|
|
what is a volume overload?
|
↑diastolic volume of the ventricle
|
|
|
what is contractile dysfunction?
|
a primary disorder of the myocardium that impairs the ability of the myocardium to generate systolic force
|
|
|
what is diastolic dysfunction?
|
impaired filling of the heart
|
|
|
in which animal is diastolic dysfunction most common?
|
cats
|
|
|
what are some clinical signs of left-sided and right-sided congestive heart failure?
|
- left-sided: cough, dyspnea, exercise intolerance (dogs & horses)
- right-sided: ascites, pleural effusion, peripheral edema |
|
|
why is heart enlargement thought to result in coughing?
|
bronchial compression
|
|
|
what is the only non-invasive means to make a diagnosis of left-sided CHF?
|
thoracic radiography
|
|
|
in dogs with an acquired heart disease, what clinical sign is usually present?
|
left atrial enlargement
|
|
|
in cats what is the most common form of acquired heart disease?
|
myocardial disease
|
|
|
what is a limitation of echocardiography with regards to diagnosing cardiac dysfunction?
|
does not provide information regarding the consequences of cardiac dysfunction – one cannot make a diagnosis of CHF based on echo alone
|
|
|
what is the best method to diagnose arrhythmias?
|
EKG
|
|
|
what are some limitations of EKG with regards to diagnosing cardiac dysfunction?
|
cannot determine cardiac enlargement, murmurs, valvular disorders, etc.
|
|
|
what cardiac diagnostic is indicated when an animal presents with clinical signs such as cough or dyspnea?
|
thoracic radiography
|
|
|
what cardiac diagnostic is indicated when the cause of an enlarged radiographic cardiac silhouette is unclear and/or when an definitive etiologic diagnosis of heart disease is important?
|
echo
|
|
|
what cardiac diagnostic is indicated when the heart rate is inappropriately high, inappropriately low or inappropriately irregular?
|
EKG
|
|
|
what is the definition of heart disease?
|
any structural/functional cardiac abnormality
|
|
|
comment on the prevalence of a cough in cats, dogs, and horses, as a clinical sign of heart disease
|
- cats: rare
- dogs and horses: common |
|
|
what is a normal heart rate for a
- canine? - feline? - equine? - bovine? |
- canine: 70 - 160
- feline: 160 - 240 - equine: 24 - 50 - bovine: 60 - 110 |
|
|
how does HR correlate to size in dogs?
|
it does not
|
|
|
what are the two important characteristics of an arterial pulse?
|
1. amplitude (strength) - clinically most important
2. quality - more subjective |
|
|
what are five physiological parameters that determine arterial pulse?
|
1. STROKE VOLUME
2. aortic distensibility 3. resistance to flow (rate at which blood leaves the arterioles) 4. EDV of the arteries 5. HR |
|
|
what is the most common cause of a weak (hypokinetic) arterial pulse?
|
most often reflects a small stroke volume associated with hypovolemia or sometimes, heart disease
|
|
|
what are two common causes of an absent arterial pulse?
|
1. thromboembolism
2. "artifact" |
|
|
what are four common causes of a bounding (hyperkinetic) arterial pulse?
|
1. anemia
2. hyperthyroidism 3. aortic insufficiency (low diastolic pressure) 4. PDA (low diastolic pressure) |
|
|
what determines the distension and height of a jugular pulse?
|
right atrial (and ventricular diastolic) pressure
|
|
|
central venous pulse:
- correct positioning of the animal - in the horse, if > 8 cm, what does this suggest? |
- standing (sternal)
- if > 8cm in the horse, suggests right heart failure, volume overload |
|
|
what are two causes of mucous membrane pallor?
|
1. anemia
2. vasoconstriction |
|
|
what causes cyanosis?
|
when [deoxyhemoglobin] ≥ 4 g/dL, independent of species or size of the animal
|
|
|
what are the two types of cyanosis and what causes them?
|
1. peripheral cyanosis - stasis of blood (low CO, thrombosis)
2. central cyanosis - lung disease, rarely heart defects (Tetralogy of Fallot) |
|
|
where is the PMI in a healthy individual?
|
over the left apex
|
|
|
what is a thrill?
|
a palpable vibration of the chest wall associated with a high intensity murmur
|
|
|
what is the origin of the four heart sounds?
|
- S1: AV valve closure
- S2: semilunar valve closure - S3: early diastolic filling - S4: atrial contraction |
|
|
what is "splitting" of heart sounds?
|
when aortic & pulmonic (or mitral & tricuspid) valve closures can be discerned from each other
|
|
|
what are four causes of splitting of S2?
|
(delayed semilunar valve closure caused by)
1. outflow tract stenosis 2. volume overload 3. bundle branch block / premature complexes 4. physiologic and associated with respiration |
|
|
what is a cause of splitting of S1
|
delayed AV valve closure due to a bundle branch block
|
|
|
what causes systolic "clicks?"
|
mitral valve prolapse
|
|
|
in who are systolic clicks most common and what does this say about their heart?
|
- common in older small-breed dogs
- a precursor to mitral valve regurgitation |
|
|
what is a "gallop" heart sound?
|
an audible S3 and/or S4
|
|
|
in small animals, when are gallop sounds most commonly heard?
|
when atrial pressures are high and the ventricle is close to its elastic limit
|
|
|
what is a murmur?
|
a prolonged series of vibrations that originates from the CV system
|
|
|
why can you hear a murmur?
|
because it results from turbulent blood flow
|
|
|
what are three determinants of blood flow character that can explain murmurs?
|
1. velocity - acceleration explains almost all murmurs
2. viscosity - anemia may explain a murmur when HCT < 17 3. diameter (rare) |
|
|
what are five characterizations of murmurs?
|
1. intensity
2. timing (relative to cardiac cycle) 3. PMI (4. configuration) (5. quality) |
|
|
what is a Grade 1/6 murmur?
|
very soft and focal
|
|
|
what is a Grade 2/6 murmur?
|
a soft murmur
|
|
|
what is a Grade 3/6 murmur?
|
a murmur of intermediate intensity
|
|
|
what is a Grade 4/6 murmur?
|
a loud murmur with no thrill or an intermittent thrill
|
|
|
what is a Grade 5/6 murmur?
|
a loud murmur with an associated thrill
|
|
|
what is a Grade 6/6 murmur?
|
a loud murmur with thrill and audible when stethoscope is lifted from chest
|
|
|
a murmur that is very soft and focal, is what grade?
|
Grade 1/6
|
|
|
a murmur that is a soft murmur, is what grade?
|
Grade 2/6
|
|
|
a murmur that is a murmur of intermediate intensity, is what grade?
|
Grade 3/6
|
|
|
a murmur that is a loud murmur with no thrill or an intermittent thrill, is what grade?
|
Grade 4/6
|
|
|
a murmur that is a loud murmur with an associated thrill, is what grade?
|
Grade 5/6
|
|
|
a murmur that is a loud murmur with thrill and audible when stethoscope is lifted from chest, is what grade?
|
Grade 6/6
|
|
|
what are the three timings of murmurs and what is their time interval with respect to the heart sounds?
|
1. systolic: S1-S2
2. diastolic: S2-S1 3. continuous: BEGINS DURING SYSTOLE AND PERSISTS AFTER S2 |
|
|
what is the most common cause of a continuous murmur?
|
PDA
|
|
|
what is a to-and-fro/bellows murmur?
|
a concurrent systolic and diastolic murmur. Not the same as a continuous murmur.
|
|
|
what are the two most common areas where a murmur PMI is heard and what valves are associated with them?
|
1. left heart base (aortic/pulmonic)
2. left apex (mitral) |
|
|
when auscultating a cat, where on the body are you mist likely to hear a murmur?
|
along the borders of the sternum
|
|
|
what are two important murmur configurations, where they occur in the heart cycle, and the shape of the waveform?
|
1. ejection murmur: mid-systolic and diamond-shaped
2. regurgitant: mid-systolic and plateau-shaped |
|
|
what are the three important characteristics of a murmur that an average vet should be able to describe?
|
1. intensity
2. timing 3. PMI |
|
|
Murmurs that occur in the absence of structural cardiac disease in animals that are otherwise normal are called what?
|
innocent murmurs
|
|
|
in which animals are innocent murmurs heard?
|
puppies and kittens are most common; sometimes in adult horses
|
|
|
what is a flow, or "functional" murmur?
|
a murmur that increases in intensity with increasing cardiac output (e.g. athleticism, fever, thyrotoxicosis)
|
|
|
what are the two main physiological parameters measured by EKG?
|
1. rate
2. rhythm |
|
|
what is the standard position of a dog or cat for EKG?
|
right lateral recumbency
|
|
|
where does the EKG lead II connect?
|
left leg
|
|
|
in the normal heart, in which direction does the heart depolarize in the sagittal, transverse, and dorsal planes?
|
- right → left
- cranial → caudal - dorsal → ventral |
|
|
what are the two types of EKG lead systems and how are they wired?
|
1. bipolar leads: negative and positive electrodes; leads I, II, III
2. augmented limb leads: positive (exploring) electrode and zero potential; aVR, aVL, aVF (Left, Right, Foot) |
|
|
the dominant direction of ventricular activation is called what?
|
mean electrical axis
|
|
|
when ventricular activation is occurring normally, though the specialized conduction system, what should the QRS look like?
|
NARROW (≈ 0.7 seconds), usually upright
|
|
|
what is a major cause of syncope?
|
arrhythmias
|
|
|
what are the two general ways in which arrhythmias develop?
|
1. disease of the conduction system prevents initiation or propagation of the wave front
2. disease of the myocardium causes spontaneous depolarization of working myocytes (e.g. tachyarrhythmias) |
|

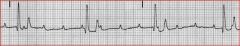
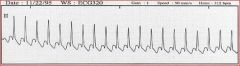
Name the arrhythmia.
|

2nd degree AV block
|
|

Name the arrhythmia.
|
3rd degree AV block
|
|
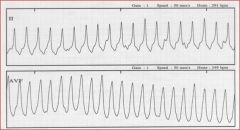
Name the arrhythmia.
|
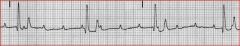
3rd degree AV block
|
|
Name the arrhythmia.
|
Atrial fibrillation (supraventricular tachycardia)
|
|
Name the arrhythmia.
|
atrial fibrillation (supraventricular tachycardia)
|
|
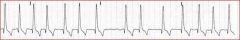
Name the arrhythmia.
|
supraventricular tachycardia
|
|
Name the arrhythmia.
|
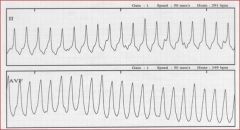
ventricular tachycardia
|
|
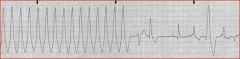
Name the arrhythmia.
|
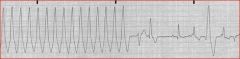
ventricular tachycardia followed by several ventricular premature complexes
|
|
|
what two general cardiac conditions are associated with the development of tachyarrhythmias?
|
1. structural cardiac disease
2. extra-cardiac disease |
|
|
what are three extra-cardiac conditions that may result in tachyarrhythmias?
|
1. electrolyte abnormalities
2. acid-base disturbances 3. "autonomic imbalance" |
|
|
what are two general causes of bradyarrhythmias?
|
1. disease (e.g., fibrosis) of the conduction system slows the rate of depolarization or "blocks" conduction
2. autonomic factors - high vagal tone (has the same functional effect as #1) |
|
|
in EKG, what are the three parameters that are most commonly assessed to diagnose an arrhythmia?
|
1. heart rate
2. rhythm (regular or irregular) 3. what is the association between atrial and ventricular activity |
|
|
what is required of a rhythm/arrhythmia associated with the sinus node?
|
a P wave of normal morphology preceding every QRS by a consistent and believable PR interval
|
|
|
a sinus arrhythmia depends on what extra-cardiac stimulus?
|
vagal discharge
|
|
|
sinus tachycardia is characterized by what heart rate in the
- dog? - cat? - horse? |
- dog: > 160 bpm
- cat: > 240 bpm - horse: > 50 bpm |
|
|
sinus bradycardia is characterized by what heart rate in the
- dog? - cat? - horse? |
- dog: < 70 bpm
- cat: < 140 bpm - horse: < 24 bpm |
|
|
an irregular, fast heart rate that is comprised of a normal PR interval and a normal QRS complex
|
supraventricular tachyarrhythmia
|
|
|
why is the QRS normal in a supraventricular tachyarrhythmia?
|
because the event occurs proximal to the bifurcation of the bundle of His
|
|
|
what diseases are associated with supraventricular tachyarrhythmias and why?
|
those that cause atrial distention (e.g. CVD, DCM, etc.) because they allow for a "critical mass" for a supraventricular ectopic event
|
|
|
what is supraventricular tachycardia?
|
three or more supraventricular tachyarrhythmia events in a row
|
|
|
disorganized electrical activity of the heart is called what?
|
fibrillation
|
|
|
what arrhythmia sounds like "bongo drums", "sneakers in a dryer", or "popcorn in a microwave"
|
atrial fibrillation
|
|
|
why does atrial fibrillation typically occur in horses and giant-breed dogs?
|
because you need the "critical mass" of heart muscle to support the arrhythmia
|
|
|
what type of arrhythmia is characterized by wide and bizarre QRS complexes? Why?
|
- ventricular premature complexes
- because the events are not occurring through the specialized conduction system |
|
|
what is the definition of ventricular tachycardia?
|
if there are three or more ventricular premature complexes in a row
|
|
|
what is the outcome of a degenerative ventricular tachycardia?
|
ventricular fibrillation → death
|
|
|
what are two breeds of dog predisposed to ventricular tachycardia due to severe myocardial dysfunction?
|
1. Doberman Pinscher
2. Boxer |
|
|
what are five extra-cardiac conditions that may result in ventricular tachyarrhythmias (and/or VTC)?
|
1. trauma (HBC)
2. GDV 3. splenic disease 4. neurologic disease 5. sepsis |
|
|
what are three general reasons why extracardiac disease can cause ventricular tachyarrhythmias?
|
1. autonomic factors
2. electrolyte disturbances 3. acid-base disturbances |
|
|
what is often characteristic of extra-cardiac ventricular tachyarrhythmias with respect to myocardial dysfunction?
|
they are often slow (< 160 bpm); "slow V-tach"; versus very high heart rates normally associated with V-tach
|
|
|
comment on the health implications of extra-cardiac "slow" ventricular tachycardia.
|
- well-tolerated by the patient
- electrically benign - resolve spontaneously |
|
|
define 1st, 2nd, and 3rd degree AV blocks.
|
- 1st Degree: PR prolongation
- 2nd degree: intermittent failure of AV conduction - 3rd degree: complete failure of AV conduction |
|
|
which AV blocks are associated with syncope?
|
2nd and 3rd degree AV blocks
|
|
|
what are three etiopathogenic causes of high 2nd degree or 3rd degree AV blocks?
|
1. idiopathic fibrosis (dogs)
2. myocardial disease 3. aortic valve endocarditis |
|
|
what are three common causes of hyperkalemia?
|
1. urethral obstruction
2. oliguric renal failure 3. Addison's disease |
|
|
what are three characteristics of hyperkalemia in an EKG?
|
1. wide QRS
2. P-waves of low amplitude or absent 3. peaked T-waves |
|
|
what are three indications for Holter monitoring (ambulatory electrocardiography)?
|
1. diagnosis of syncope
2. assessment of arrhythmias detected by resting EKG 3. evaluation of antiarrhythmic therapy |
|
|
how are tachyarrhythmias generally treated? Bradyarrhythmias?
|
- tachyarrhythmias: pharmacologically
- bradyarrhythmias: cardiac pacing |
|
|
what are the three echocardiographic modalities?
|
1. M-mode
2. 2D 3. Doppler |
|
|
what are the three standard images in M-mode echocardiography?
|
1. Left ventricle
2. mitral valve 3. Aorta / Left atrium |
|
|
name a pro and con for (1) M-mode and (2) 2D echocardiography
|
1. excellent temporal resolution, but poor spatial resolution
2. excellent spatial resolution, but discrete frame rate |
|
|
how is LV dilation / hypodynamic (hypokinetic) performance, for example, in dilated cardiomyopathy evaluated quantitatively with echocardiography? What are normal values for dogs?
|
- measured in %FS = (LVED-LVES)/LVED
- in most healthy dogs, 25 < %FS < 45 |
|
|
in echocardiography, how is LA size assessed and what are normal values?
|
- assessed by comparing left atrium to aorta diameter
- LA/Ao < 1.6 - 1.4 in dogs and cats (depending on mode and species) |
|
|
what are the two Doppler echocardiographic conventions?
|
1. spectral doppler - flow towards the transducer = positive velocities
2. color flow Doppler: BART - blue away, red toward |
|
|
what three pieces of information does Doppler echocardiography provide?
|
1. velocity of flow
2. direction of flow 3. character of flow |
|
|
what are the three Doppler echocardiographic modalities and what information do they provide?
|
1. pulsed wave Doppler: quantification of physiologic velocities
2. continuous wave Doppler: quantification of supraphysiologic velocities 3. color flow Doppler: detection of flow disturbances |
|
|
how can you determine change in pressure from one structure to another (e.g. left ventricle to aorta with a subaortic stenosis), if you know the velocities (from echocardiography) of blood flow at each site?
|
- use the simplified Bernoulli equation:
- ΔP = 4 (v2² - v1²) - where v = velocity |
|
|
almost all forms of congenital heart disease have what clinical sign?
|
murmur
|
|
|
if you find a murmur and diagnose congenital heart disease, but the patient has absolutely no clinical signs, what does that mean?
|
- most patients are healthy at time of detection
- lack of clinical signs does not imply good prognosis |
|
|
in which species has congenital heart disease found to be heritable?
|
dogs
|
|
|
characterize an "innocent" murmur.
|
- always systolic
- always soft |
|
|
what is the most appropriate treatment approach for congenital heart disease
|
mechanical means (i.e., surgery, interventional catheterization)
|
|
|
what are the three basic therapeutic approaches to treat congenital heart disease?
|
1. surgical (± pulmonary bypass: $$$)
2. interventional catheterization techniques 3. medical therapy |
|
|
what are two common types of interventional catheterization techniques to treat congenital heart disease?
|
1. balloon dilation of obstructions
2. occlusion of shunts |
|
|
PDA pathophysiology:
- direction of shunting - abnormal loads on the heart - three potential lesions to the heart if untreated or severe |
- shunt is from left → right
- volume load on LA and LV - myocardial dysfunction, mitral valve regurgitation, and CHF |
|
|
what breeds of dogs are most commonly afflicted with a PDA? Sex predisposition?
|
- small breed females
- German Shepherd - Sheltie |
|
|
what are two CV-based clinical signs of a PDA on routine physical exam and auscultation?
|
1. continuous murmur
2. bounding arterial pulses from diastolic bleedoff |
|
|
what are three important radiographic findings of a PDA?
|
1. dilation of aorta and main pulmonary artery
2. cardiomegaly due to LA/LV enlargement 3. pulmonary hyperperfusion |
|
|
what are four important echocardiographic findings of a PDA?
|
1. LA/LV enlargement
2. mitral valve regurgitation 3. continuous disturbed flow within the MPA 4. ductus visible in left cranial parasternal images |
|

what (type of) breed of dog is this?
|

brachycephalic (bulldog)
|
|

what defect does this dog have?
|

generalized cardiomegaly/pericardial effusion
|
|

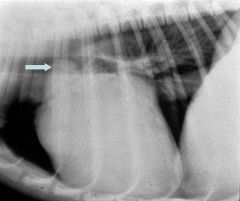
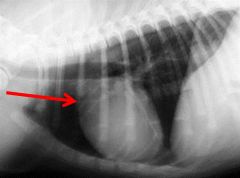
to what is the arrow pointing in this normal dog?
|

left auricle
|
|

what defect does this dog have?
|

left atrial enlargement
note: the "cowboy straddle" in the bronchi |
|

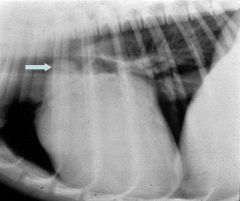
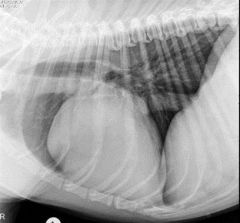
what defect does this dog have?
|

left atrial enlargement
note: bulge at 2:00-3:00 and "cowboy straddle" of the main stem bronchi |
|

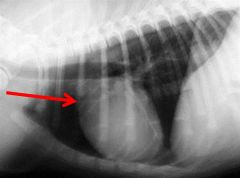
what defect does this dog have?
|

left ventricular enlargement
|
|

what defect does this dog have?
|

right heart enlargement due to heartworm disease
|
|

what defect does this dog have?
|

left heart enlargement with concurrent pulmonary edema
|
|
what defect does this dog have, as indicated by the arrow?
|
pulmonary trunk enlargement
|
|
to what is the arrow pointing in this normal dog?
|
aorta, right auricle, and pulmonary artery
|
|

to what is the arrow pointing in this normal dog?
|

left atrium
|
|

to what is the arrow pointing in this normal dog?
|

left ventricle
|
|

to what is the arrow pointing in this normal dog?
|

right ventricle
|
|

what position is this dog in?
|

left lateral recumbency
|
|

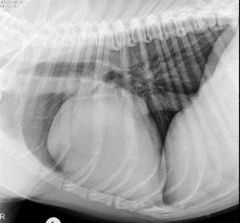
what defect does this dog have?
|

left atrial enlargement
NOTE: vertical caudal border, caudal and dorsal bulge, elevated carina, and split mainstem bronchi |
|

what defect does this dog have?
|

severe left atrial enlargement
|
|

what defect does this dog have?
|

pericardial peritoneal diaphragmatic hernia
|
|
what is the defect in this dog?
|
right heart enlargement due to tricuspid insufficiency
note the wide heart and increased sternal contact |
|

what defect does this dog have?
|

right heart enlargement due to pulmonic stenosis
note the "reverse-D" shape |
|

what view of the dog is this?
|

right lateral recumbency
|
|
|
which view, VD or DV, is a more accurate representation of the heart in radiography?
|
DV
|
|
|
how does the inspiration/expiration change the evaluation of the radiograph of the heart?
|
looks bigger on expiratory
|
|
|
what is the best lateral view for a radiograph of the heart?
|
right lateral recumbency
|
|
|
what are two big differences between a brachycephalic dog and a normal dog when assessing the heart radiographically?
|
1. the apex may point more exaggerated to the left
2. exaggerated right deviation of the trachea |
|
|
on a lateral view, what are four radiographic indications of right heart enlargement?
|
1. increased width
2. increased sternal contact 3. elevation of apex 4. elevation of trachea (if severe) |
|
|
on a DV view, what are three radiographic indications of right heart enlargement?
|
1. "Reversed-D" appearance
2. ↓ distance from right heart border to right chest wall 3. apex shift to the left |
|
|
on a lateral view, what are three radiographic indications of left heart enlargement?
|
1. enlargement of the caudodorsal border
2. dorsal deviation of the trachea (parallel to the spine) 3. may see caudal bronchi compression or separation of the bronchi |
|
|
on a lateral view, what are four radiographic indications of left atrial enlargement?
|
1. vertical caudal border of the heart
2. caudal and dorsal bulge 3. elevated carina 4. separation of left and right mainstem bronchi |
|
|
on a DV view, what are three radiographic indications of left atrial enlargement?
|
1. left auricle may bulge at 2:00 - 3:00
2. left atrium may produce increased opacity at the base of the heart 3. lateral "bow-legged cowboy" deviation of the stem bronchi |
|
|
on a lateral view, what are two radiographic indications of left ventricular enlargement?
|
1. caudal border is elongated and upright
2. elevation of trachea |
|
|
on a DV view, what are three radiographic indications of left ventricular enlargement?
|
1. rounding of left ventricular border
2. decreased space between left heart and left chest wall 3. increased length |
|
|
on a lateral view, how does a pulmonary trunk enlargement appear?
|
bulge in the craniodorsal heart, often superimposed over the trachea
|
|
|
on a DV view, how does a pulmonary trunk enlargement appear?
|
bulge at 1:00 - 2:00
|
|
|
on a lateral view, how does ascending aortic enlargement appear?
|
bulge in the craniodorsal heart border (cranially slanted heart)
|
|
|
on a DV view, how does ascending aortic enlargement appear?
|
bulge from 11:00 - 1:00
|
|
|
on a lateral view, how does descending aortic enlargement appear?
|
usually not visible
|
|
|
on a DV view, how does descending aortic enlargement appear?
|
bulge in descending aorta, just below area of pulmonary trunk
|
|
|
in a lateral view, how does left heart enlargement appear?
|
- increased length of heart
- "beer belly" |
|
|
what are two approaches to correct a PDA?
|
1. ligation following left thoracotomy
2. transcatheter ductal occlusion |
|
|
what is the pathophysiology of pulmonic stenosis?
|
- a pressure gradient develops across the obstruction
- pressure load on the right ventricle - right sided congestive heart failure (ascites) is a potential sequela |
|
|
what breeds of dogs are most predisposed to pulmonic stenosis?
|
1. terriers
2. English bulldogs |
|
|
what will you hear on auscultation of a pulmonic stenosis?
|
systolic murmur at the left heart base
|
|
|
describe the definitive diagnosis of pulmonic stenosis
|
- doppler echo required for definitive diagnosis and assessment of severity
- gradients > 80 mmHg constitute severe PS |
|
|
what are three ways to treat a pulmonic stenosis?
|
1. interventional catheterization via balloon valvuloplasty (preferred as the initial treatment when indicated)
2. patch graft following temporary venous occlusion 3. definitive repair under bypass |
|
|
balloon valvuloplasty to treat pulmonic stenosis:
- mortality - efficacy |
- relatively low mortality
- efficacy varies, but is favorable in dogs with a gradient > 80 mmHg, whether or not clinical signs present. |
|
|
if a pulmonic stenosis is left untreated, what generally occurs?
|
severe congestive heart failure in the first three years of life, or sudden death
|
|
|
what is the pathophysiology of subaortic stenosis?
|
- in order to maintain normal systemic pressures and flow, the LV must generate abnormally high systolic pressures
- a pressure gradient develops across the obstruction - pressure overload on the LV → concentric left ventricular hypertrophy |
|
|
what are the pressure gradients for mild, moderate, and severe subaortic stenosis?
|
- mild: < 40 mmHg
- moderate: 40-80 - severe: > 80 |
|
|
comment on the predisposition of subaortic stenosis in Newfoundland dogs?
|
it is inherited as a polygenic trait
|
|
|
what are four dog breeds predisposed to congenital subaortic stenosis?
|
1. Newfoundland
2. Golden Retriever 3. Rottweiler 4. Boxer |
|
|
what are two cardiovascular findings on physical exam, of subaortic stenosis?
|
1. systolic murmur over the left heart base
2. weak (hypokinetic) arterial pulse |
|
|
diagnosis of subaortic stenosis:
- what if it is mild? - what is the accepted screening method - when is Doppler echo indicated? |
- mild SAS has genetic implications
- auscultation is the screening method - Doppler is indicated when a murmur is detected |
|
|
comment on the treatment of subaortic shunts:
- definitive correction - prognosis - other palliative care |
- definitive correction requires bypass
- however, this correction does not affect survival - balloon dilation may be palliative - β-blockade (atenolol) may helpfully decrease HR and myocardial oxygen demand |
|
|
what role does subaortic stenosis play in congestive heart failure?
|
this is uncommon
|
|
|
what is the most common location for a ventricular septal defect?
|
in the membranous area "high" in the septum
|
|
|
describe the pathophysiology of a ventricular septal defect:
- shunting - load on the heart - clinical importance |
- left-to-right shunt (in the absence of other factors)
- imposes a volume load on the LV and LA - importance depends on size of the defect and presence of other defects |
|
|
comment on the prevalence of ventricular septal defects in the cat
|
they are relatively common
|
|
|
what are three dog breeds predisposed to ventricular septal defects?
|
1. bloodhound
2. English bulldog 3. Shiba Inu |
|
|
what findings on auscultation are associated with a ventricular septal defect that is large? Small?
|
- any size: systolic murmur
- small size: right apical thrill |
|
|
how is a ventricular septal defect definitively diagnosed?
|
echo
|
|
|
how are ventricular septal defects treated?
|
- most VSD in small animals are small and do not require therapy
- large/complex: bypass - medical therapy to lower BP and drugs like digoxin/pimobendan |
|
|
what are two common lesions in the heart that concur with ventricular septal defects?
|
1. aortic valve insufficiency
2. right ventricular outflow tract obstruction |
|
|
atrial septal defects:
- pathophysiology - if a murmur exists, where does it come from? - prevalence - treatment |
- ASD causes left → right shunting and imposes a volume load on the right atrium and ventricle
- murmurs result from a "functional pulmonary stenosis" - ASD are relatively uncommon - can be repaired per catheter or under bypass |
|
|
abnormal development of the mitral and/or tricuspid valve is called what?
|
AV valve dysplasia
|
|
|
that are two outcomes (seen by echocardiography) of AV valve dysplasia?
|
1. regurgitation
2. stenosis |
|
|
AV valve dysplasia:
- prevalence in cats - dog breed most predisposed - severity - how is it fixed? |
- relatively common in cats
- common in Labrador Retriever - variable severity - requires bypass to correct |
|
|
what is cyanotic heart disease?
|
right → left shunts that result in venous admixture
|
|
|
cyanotic heart disease requires a shunt and one of what three other conditions?
|
1. tricuspid stenosis
2. severe pulmonic stenosis 3. pulmonary hypertension with elevated vascular resistance |
|
|
what are two clinical signs of cyanotic heart disease?
|
1. exercise intolerance
2. complications of polycythemia |
|
|
shunt reversal due to increased pulmonary vascular resistance is called what?
|
Eisenmenger's Physiology
|
|
|
right-to-left PDA:
- age of animal - type of murmur - key clinical sign - treatment |
- shunt occurs early in life
- typically, no murmur - marked hind-limb exercise intolerance - phlebotomy is palliative |
|
|
what are the four conditions associated with Teratology of Fallot?
|
1. pulmonic stenosis
2. ventricular septal defect 3. right ventricular hypertrophy 4. aortic malposition |
|
|
how is Teratology of Fallot treated?
|
- definitively under bypass
- phlebotomy / β-blockade may be palliative |
|

to what is the arrow pointing in this normal dog?
|

Aorta
|
|

to what is the arrow pointing in this normal dog?
|

Left Venticle
|
|

to what is the arrow pointing in this normal dog?
|

Pulmonary Artery
|
|

to what is the arrow pointing in this normal dog?
|

Right Atrium
|

