![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
19 Cards in this Set
- Front
- Back
|
CHF: Definition, Causes, Factors causing decompansation.
|
Is the inability of the heart to produce a cardiac output sufficient for the metabolic needs of organs. Can be defined as systollic or diastollic heart failure. Systolic is LVEF <50%, and diastolic is defined as >50%LVEF. Causes are vast, important to discren between ischemic vs non ischemic. HTN, drug, myocarditiis, high output (anemia, hyperthyroidism, pregnancy, stress, infection). Factors that complicate CHF include ischemia, arrythmia, CV stress (infection, anemia, pregnancy), PE, medical noncompliance, dietary.
|
|
|
CHF: Diagnosis (HandP,)
|
Hx: Decrease exercise tolerance, orthopnea, PND, SOB, weight gain, edema, RUQ tenderness. Low output fatigue, malaise, decreased appeptite. Physical includes right sided (elevated JVP, hepatojugular reflux, ascities, peripheral edema, enlarged liver). Left sided rales tachypena, S3.
|
|
|
CHF: Diagnosis (Labs)
|
Chem 7, CBC< TSH, FT4, FT3, LFT, Lipid panel, Urinalysis, trop, CIP. BNP (<100 effectively ruled out)
12 lead EKG, CXR. Echo. |
|
|
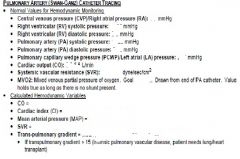
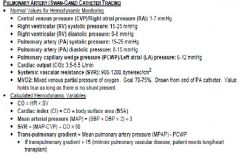
CHF: Indications for Swanz Ganz in CHF
|
Hypoperfusion with narrow pulse pressure, AMS, declining function despite normal volume status. Congestion with angina, baseline renal insufficency. Persistant congestion despite salt and fluid restriction.
|
|
|
CHF: Goals of Swanz-Ganz
|
RA<7mmHg, PCWP <15mmHg, SVR <1200 and SBP >80mg.
If elevated filling pressures (PCWP >20 or RA >10) diurese with lasix until PCWP is low as possible with SBP above 80. If SVR elevated above 1300 bein afterload reduction with nitroprusside 20mcg/min. Low Cardiac Index <1.2 condiser dobutamine, or dopamine first then dobutamine. DC once optimal for 4-8 hrs |
|
|
|
|
|
CHF: Managment Sub acute
|
-Ace Inibitor: Captopril 50mg PO TID, Enalapril 10mg PO BID, Benazepril 40mg PO QD, Lisinopril 40mg PO Dialy. If BP remains to high ad Hydralizine up 100mg PO QIDc
-Beta blocker: Carvediol 3.125mg PO BID titrate up to target PO BID. Toprol XL 12.5 daily. -Spirnolactone (Class III-IV or ischemic): 12.5mg goal 25mg PO QD. Adjust K and loop diuretic, check chem panel in 7days. (CI Male Cr > 2.5, female >2 |
|
|
CHF: Managment of Volume Excess
|
Lasik (can add metolazone). Morphine, Nitrates, Oxygen, Position (head up)
|
|
|
CHF: Early Pacemaker Complications
|
Pneumothorax (CXR)
Hematoma formation (especially if on anticoagulation) Lead perforation of RA or RV Lead dislodgment |
|
|
Chronic Valve: Aortic Stenosis
|
Symptoms: Asymptomatic. Symptomatic poor prognosis Angina 5 years, Syncope 3 years, Heart Failure 3 years. Treated based on symptoms
Signs: Murmur at right upper sternal border, Paradoxical splitting of S2, narrow pulse pressure, pulses et tardus. Imaging: Normal Valve area 3-4cm, Mild 1.5cm <25mmHg, Moderate 25-50mmHg 1.0-1.5cm, Severe >50mmHg <1.0, Critical 80mmHg <0.7cm |
|
|
Chronic Valve: Aortic Regurgitation Symptoms and SIgns
|
Signs; Diastolic blowing murmur in the LUSB, wide pulse pressure, water hammer, Quincke's sign (capillary pulsations at fingertips, De Musset's sign (bobbing head), Muller's sign (pulsing uvula).
|
|
|
Chronic Valve: Aoritic Regurgitation Surgery Indications
|
NYHA functional class III or IV. Severe LV dilatation >75mm end diastolic or >55mm end systolic. LV dysfunction <50%. Concomitant angina or severe AR. Progressive LV dilatation, declining LVEF or exercise tolerance.
|
|
|
Chronic Valve: Mitral Stenosis
|
Low rumbling diastolic murmur heard best at apex. Opening snap may be heard.
On echo severity Mild < 5mmHg >1.5cm2, Moderat 5-10mmHg, 1-1.5cm2, Severe >10mmHg <1cm2. Indication for surgery include NYHA Class III-IV symptoms, moderate or severe mitral stenosis. |
|
|
Chronic Valve: Mitral Regurgitaion
|
Clinical Signs: Loud holosystolic high pitched heard best at apex and transmitted to axillia, soft S1.
Surgical indication: NYHA Class III or IV, LV end systolic dimension >45mm, LV end systolic volume index >50ml/M2, LVEF <60% and progressing. |
|

|
|
|
|
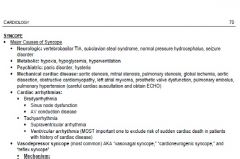
Syncope: Vasovagal Mechanisms
|
Stimulation of vasodepressor region of the brain stem results in overactivation of parasympathetic leading to bradycardia and vasodiltation. Occurs via gastrointestinal and genitourinary mechanoreceptors, cerbral (panic, fright, pain, noxius stimuli), Cardiopulmonary barorecptor (carotid sinus, tussive) Cardiac C fibers (valsalva, upright tilt, jacuzzi, weight lifting, trumpet, post exercise, volume depletion, SVT).
Diagnosed by tilt table. Treated by : Beta blocker (stops initial sympathetic tone increase) |
|
|
Syncope: Risk Stratification High Risk
|
Anyone with Brady <40, Pauses >3 sec, Trifaciular block, Afib/flutter, NSVT, EKG ST abnorm or long QT, Dysfunctional pacer, Sx/signs of CHF, Ischemic chest pain, severe valvular disease, GI blood loss.
To CCU |
|
|
Syncope: Risk Stratification Moderate
|
Age >60, Hx CAD, CHF, Old LBBB, Family Hx Sudden death, Pacer/defib functioning, Persistent BP<100, Symptoms no consistent with vaso-vagal event.
|
|
|
Syncope: Risk stratification Low Risk
|
Age <50. No cardiac History. Symptoms consistent with vasovagal. No orthostatic BP drop
|

