![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
140 Cards in this Set
- Front
- Back
|
What are the 3 cardiomyopathies?
|
dilated, hypertrophic, restrictive
|
|
|
Dilated Cardiomyopathy Hallmarks
|
Enlarged, dilated chambers, systolic dysfunction (low ejection fraction)
|
|
|
Hypertrophic Cardiomyopathy Hallmarks
|
Stiff, thickened myocardium. The hypertrophy is deforming so that diastolic filling is incomplete (diastolic dysfunction).
|
|
|
Restrictive Cardiomyopathy Hallmarks
|
Rarest form. Stiff, noncompliant ventricle that fills incompletely in diastole (Diastolic dysfunction).
|
|
|
#1 cause of dilated cardiomyopathy. Who is most at risk?
|
Majority of cases IDIOPATHIC. 3X more prevalent among males and blacks.
|
|
|
Etiologies of dilated cardiomyopathy
|
* #1 is IDIOPATHIC
* Infectious (Acute Viral Myocarditis caused by Echovirus and Cox B)...Toxoplasmosis (Chaga's Disease), Fungal, Bacterial * Toxic (ALCOHOLIC CARDIOMYOPATHY) * Inherited (FAMILIAL CARDIOMYOPATHY) * PERIPARTUM * Also, Ischemic, Valvular, Hypertensive, Inflammatory (Infectious & Non infectious), metabolic, nutritional, neuromuscular) * STRESS CARDIOMYOPATHY (reversible, stress induced.) |
|
|
Pathophysiology of Dilated Cardiomyopathy
|
Systolic dysfunction leads to decrease cardiac output. Ventricular dilation results in decreased cardiac output. This leads to various neurohumoral compensatory activations:
* adrenergic nervous system (sympathetic response * renin-angiotensin-aldosterone increase systemic vascular resistance * Vasopressin (peripheral vascular constriction * Natriuretic peptides * Endothelin |
|
|
CP of Dilated Cardiomyopathy
|
* Common first symptom: exertional intolerance
* Decreased Systolic Function Characterized by Decrease in Ejection Fraction (>30% with severe symptoms) * Thinning of chamber walls and dilation of chamber size. * Viral form often preceded by viral respiratory infection followed by heart failure symptoms (dyspnea, weakness * Valvular regurgitation (mitral before tricuspid) * Left before right congestive symptoms. |
|
|
Evaluation of Dilated Cardiomyopathy
|
* Echocardiogram (for function, left ventricular size)
* Biomarkers (Troponin) * Cardiac MRI |
|
|
Treatment of Dilated Cardiomyopathy
|
* Angiotensin receptor Blocker (ARB)
* ACE inhibitor * Spironolactone |
|
|
Etiology of Hypertrophic Cardiomyopathy
|
* Familial in 55% of cases with Autosomal Dominant Transmission. (mutations in proteins of cardiac sarcomere)
* Also spontaneous mutations |
|
|
Pathophysiology of Hypertrophic Cardiomyopathy
|
Diastolic Dysfunction (lack of ventricular filling) resulting from hypertrophic ventricles.
|
|
|
CP & Eval of Hypertrophic Cadiomyopathy
|
CP: Left Ventricular Hypertrophy NOT due to pressure overload. Vigorous Systolic Function. Supranormal ejection fraction
Dyspnea on exertion is MOST COMMON. Chest Pain, Syncope, Harsh Murmur, Arrythmias. Bisferiens Carotid Pulse Eval: Echo (shows septal hypertrophy and enhanced contractility, EKG, Cardiac MRI confirms hypertrophy. Cardiac cath confirms diagnosis |
|
|
Tx of Hypertrophic Cardiomyopathy
|
* Treat Symptomatically. No therapy has been shown to improve mortality.
* Beta Blockers (initial drug) - This results in slower heart rates to assist with diastolic filling. * Calcium Channel Blockers * Anti-arrhythmics SURGICAL TREATMENTS: |
|
|
Restrictive Cardiomyopathy Etiology & Pathophysiology
|
* Least Common Cardiomyopathy
* Impaired ventricular filling due to an abnormally stiff & rigid ventricle * Normal Systolic function (early) * Intraventricular pressure rises precipitously disproprtionately with small increases in volume * Caused by infiltration of myocardium by abnormal substance fibrosis or scarring of endocardium * Causes diastolic dysfunction * Amyloidosis - deposits of amyloid throughout heart Sarcoidosis - Restriction, Conduction System Disease Hemochromatosis - Iron overload or iron storage disease. Endoymyocardial Fibrosis - Thickening of basal inferior wall. |
|
|
Restrictive Cardiomyopathy CP & Evaluation
|
CP: Right HF > Left HF
* Dyspnea * Orthopnea / Paroxysmal Nocturnal Dyspnea * Peripheral Edema * Ascites * Hepatomegaly * Decrease in exercise intolerance * MIMICS Constrictive Pericarditis |
|
|
Restrictive Cardiomyopathy Treatment
|
Treat underyling cause (diuretics for congestive symptoms, digoxin, anti-arrythmics, pacemaker for conduction system disease, anticoagulation for thrombus
|
|
|
Heart Failure Definition (old & new)
|
Old - Abnormality of cardiac function is responsible for failure of heart to pump blood at rate commensurate with requirement of metabolizing tissues or to do so at elevated filling pressures.
New - Complex clinical syndrome characterized by abnormality of LV function and neurohormonal regulation accompanies by effort intolerance, fluid retention, and reduced longevity |
|
|
Preload & Afterload Definitions.
How is preload measured? |
Preload - Also called filling pressure. It is the LVEDP (Left Ventric. End Diastolic Pressure). It is surrogately measured using PCWP (Pulmonary Capillary Wedge Pressure)
Afterload - Load after onset of contraction against which LV contracts. Systemic Vascular Resistance. |
|
|
Define cardiac contractility. How is it measured?
|
It's how well the heart contracts for any given heart rate, preload, and afterload. Measured using EF as surrogate. Normal EF is 60%.
|
|
|
What EF characterizes systolic dysfunction?
|
EF < 40-45%
|
|
|
What are factors that influence preload, afterload, and cardiac contractility?
|
Preload - Volume depletion decreases. Volume expansion increases.
Afterload - Sepsis & vasodilators/antihypertensives decreases. Hypertension increases. Contractility - Myocardial damage (MI, long HTN) decrease. Inotropic agents alter |
|
|
Systolic & Diastolic Dysfunction Definitions & Etiologies
|
Systolic - Decreased ability of ventricle to eject blood. Eti: #1 - CAD, #2 - HTN, #3 - Genetic, also Idiopathic, Endocrine, valvular, toxic (ETOH, Cocaine), Arrhythmia, SLE, Viral
Diastolic - Decreased ability of ventricle to accept blood. Eti: filling problem. Most common is LVH (commonly resulting from HTN) |
|
|
What is endothelin
|
Peptides released from endothelial cells. Most potent vasoconstricting hormones known
|
|
|
Manament of systolic vs diastolic dysfunction
|
Systolic: Defnite therapeutic recommendations...Diuretics + ACE-inhibitors to control RAAS Pathway (blunting the remodeling process) or use ARBs if ACE-intolerant, Beta-Blockers (only 3: Carvedilol, Bisoprolol, Metoprolol), Aldosterone Antagonist (Spironolactone). Treat residual symptoms with Digoxin. Also add Isosorbide Dinitrate/Hydralazine (Hyd/ISDN) in blacks.
Diastolic: Generalizations, poorly studies. Avoid tachycardia, treat ischemia, control BP |
|
|
Potential adverse effects with Spironolactone (Aldosterone Antagonist used in CHF)
|
Hyperkalemia -> renal failure. Monitor labs during treatment.
|
|
|
Natural History of Chronic Heart Failure
|
* Normal heart experiences an injury (e.g. MI). Leads to change in size, geometry, and function of heart. Results in cell death, ventricular wall thinning, hypertrophy, spherical instead of eliptical (Mavericks instead of Cowboys), and accumulation of collagen in cardiac interstitium.
* This is known as Cardiac Remodeling. A big reason it occurs is from neurohormonal activation (RAS, SNS, ET) resulting from decreased cardiac output. Positive feedback downward spiral ensues. |
|
|
Right Heart Failure Etiology, Pathophys, CP
|
Eti & Pathophys: RV failure. Most commonly results from LV failure. Can be from pulmonary disease (e.g. emphysema which can result in pulmonary hypertension, straining the RV. Results in increased pressure in systemic veins
CP: Edema, Ascites, Pleural effusion, increased JVP, Anorexia, Weight Change, cachexia, poor vitals, hepatomegaly, tricuspid regurg. JVP IS MOST IMPORTANT FINDING |
|
|
Left Heart Failure Etiology, Pathophys, CP
|
Eti & Pathophys: LV failure. systolic or diastolic dysfunction. Can be secondary to valvular abnormality. Increased pressure in pulmonary veins leads to pulmonary congestion/edema.
CP: Breathlessness (DOE, Orthop, PND), Fatigue, Cerebral (TIA, CVA, Syncope), Rales, lung effusion, S3 heart sound, triscuspid regurg |
|
|
Heart Failure Diagnostics
|
*B-Type Natriuretic Peptide! (Does not work in obese patients) - increased value is positive finding. Very important biomarker. Secreted from LV from myocyte stretch
*Chest X-Ray - Heart Size, pulmonary edema * Labs: Na (hyponatermia), LFT (rise in liver function) *Pulmonary Capillary Wedge Pressure |
|
|
Typical radiographic findings of a HF patient
|
Increased heart size, PVR/pulmonary edema.
(PVR - pulmonary vascular resistance?) |
|
|
Pharmacologic agents for treating HF
|
#1) ACE Inhibitor & Diuretics - 1st line Tx. Results in diuresis and salt excretion -> lower BP. Not sure how this helps CHF. Use an ARB if ACE-intolerant
#2) Beta Blockers - "Mechanism Unclear", but it's likely that chronic chatecholamines and SNS activity cause myocyte damage. Only 3 work: Bisoprolol, Metoprolol, Carvedilol #3) Aldosterone Antagonist - Spironolactone, Eplerenone. Carries Risk of Hyperkalemia -> renal failure. Monitor! #4) If black, then add Isosorbide Dinitrate/Hydralazine. #5) Add Digoxin if necessary to treat residual symptoms. |
|
|
General management principles of CHF, including nonpharmacologic management
|
* Use pharmaceuticals to control neurohormonal activation caused by HF. These neurohormonal chemicals (RAAS, SNS, ET) cause a) myocardial toxicity and b) peripheral vasoconstriction, exacerbating HF.
* In addition to pharmaceuticals, educate patients on SALT RESTRICTION, about implementing a "flexible diuretic regimen". Weigh oneself daily, adjust diuretics to minimize fluctuations in body fluid weight. And of course, EXERCISE * DEVICE THERAPY: CRT +/- ICD. Cardiac Resynchronization Therapy if symptoms persist and if patient has IVCD (interventricular conduction defect) -> poor ventricular coordination. The EKG sign is a WIDE QRS. Can add an ICD if risk of arrythmias. |
|
|
Precipitating causes which may lead to decompensation of chronic heart failure
|
* Noncompliance of diet and medication
* HTN * Arrythmia * Iatrogenic * Infection * MI/Ischemia * Endocrine/anemia * Pulmonary Embolism |
|
|
Indicators for hospitalization for patients with chronic CHF
|
* Deterioration of symptoms not responsive to oral medications
* Concern for ischemia/MI in ischemic cardiomyopathy * Altered lab results: Cr, K, INR * Syncope * Thromboembolic Event * Arrhythmia: VT/VF, new atrial fib |
|
|
NYHA Classes of CHF
|
Class 1 - Asymptomatic
Class 2 - "Mild Limitations". Some symptoms Class 3 - "Moderate Limitation". Walk 1-2 blocks on level or 1 flight of stairs Class 4 - "Severe Limitation". SOB @ rest, dressing, or showering. |
|
|
ACC/AHA Stages of HF
|
Stage A - High risk for HF, but no structural hear disease of symptoms
Stage B - Structural heart disease but no symptoms Stage C - Structural heart disease with prior or current HF symptoms Stage D - Refractory HF requiring specialized interventions. Stage A & Stage B = NYHA Class 1 Stage C = NYHA Class 2 & 3 Stage D = NYHA Class 4 |
|
|
Aortic Stenosis (Eti, Pathophys, CP, Diagnostics, Tx, Natural Hx)
|
Eti: 3 causes-
degenerative - most common, from atherosclerotic deposits and calcium in cusps, along commisures, older patients (70-80) congential - calcified commissures, age 40-50 (usually bicuspid) rheumatic - fibrosis & calcification of leaflets and commissues, Starts w mitral valve, then aortic. Inflammatory autoimmune rxn. Pathophys: As diameter decreases, velocity increases to maintain flow. Leads to LV hypertrophy, leads to diastolic dysfunction and eventually systolic dysfunction. BP maintained by SNS. CP: Mid-Systolic Ejection Murmur (maybe with Ej Click). A2 may be decreased/delayed (paradoxical splitting). S4 common. Carotid a bit thready/weak, delayed. When Pt is symptomatic, 3 cardinal signs: ANGINA, SYNCOPE, CHF. Diagnostics: TTE (assess valves and chambers), Cath Tx: Valve Job when SYMPTOMATIC. Follow up until then. Natural Hx: Gradual progression over many years. Asymptomatic until moderate to severe. Poor prognosis when symptomatic |
|
|
Mitral Stenosis (Eti, Pathophys, CP, Diagnostics, Tx, Natural Hx)
|
**Eti:
1) Rheumatic Heart Disease - Progressive destruction, fibrosis and calcification, fusion of commisures. Symptomatic 10-30 years after acute rheumatic fever 2) Rare causes - mitral annular calcification in eldery. congenital mitral stenosis **Pathophys: Increase in LA pressure -> "Bagging out" & Dilation -> Pulmonary Vessel hypertension. Increases Afib tendencies. LV Function normal **Natural Hx: Mild stenosis is asymptomatic at rest, may have symptoms on exertion. Moderate to severe has elevated LA pressure at rest, pulmonary hypertension & congestion, fatigue due to low cardiac output. Atrial Fib common. Risk of LA thrombus formation and stroke **CP: Atrial Fib, Exertional SOB & fatigue, Loud S1, Opening Snap, Diastolic Murmur (rumble), signs of pulmonary hypertension **Diagnostics: Echoto determine severity & pressure gradient **Tx: RELIEF OF SYMPTOMS & PREVENTION OF STROKE. Heart rate control to control symptoms (B Blockers, Maintain sinus rhythm) -> keep diastole long to allow for LV filling. Diuretics for pulmonary congestion. Anticoagulation for all patients with Afib, Dilated LA, or prior embolic event. Surgeries: Balloon valvuloplasty to crack calcified commisures OR valve replacement |
|
|
Pulmonic Stenosis (Eti, Pathophys, CP, Diagnostics, Tx, Natural Hx)
|
**Eti: Not very Common. Usually congenital. VERY RARELY RHEUMATIC HD, Cardinoid, Tumors.
**Pathophys: Pressure gradient develops between RV and pulm.art. **CP: Mild = no symptoms. Moderate-Severe = exertional fatigue, dyspnea, syncope. Harsh Mid-Systolic ejection murmur. THRILL. Tx: Intervention when symptomatic. Balloon valvuoplasty. |
|
|
Triscuspid Stenosis (Eti, Pathophys, CP, Diagnostics, Tx, Natural Hx)
|
**Eti: Biggest valve in heart -> Hard to get Stenotic. RARE. Almost always secondary to Rheumatic Mitral Stenosis.
**Pathophys: Pressure graident develops e/ RA and RV -> elevated RA pressure, systemic venous congestion, low CO **CP: Signs of elevated neck veins. Edema, Hepatomegaly. Cardiac findings often obscured by Mitral stenosis findings. Diastolic murmur, Opening Snap. Tx: Good outcomes in asymptom. patients. Treat if symptomatic. |
|
|
Aortic Regurg. (Eti, Pathophys, CP, Diagnostics, Tx, Natural Hx)
|
**Eti: Either leaflet problems (endocarditis holes, rheumatic, trauma, myxomatous) OR annulus problems (aortic annulus dilation)
**Pathophys: Backflow increase LV diastolic pressure -> increase in pulmonary venous pressure. LV dilates of time. Coronary flow during diastole may be compromised due to lack of aortic pressure. CP: 2 Flavors: CHRONIC & ACUTE. tachycardia, hypotension, soft diastolic murmur. Emergency! CHRONIC: long asymptomatic period, diastolic murmur, wide pulse pressure, peripheral pulse changes (head bobbing, etc) Diagnostics: Start with Echo, Cardiac Cath **Natural Hx: Mortality very low in asymptomatics. *Tx: No proven therapies. Surgery if symptomatic AND if LV dilation is progressive OR ejection fraction deteriorates. "Rule of 55" Operate before LVEF < 55% or LV end-systolic dimension > 5.5cm |
|
|
Mitral Regurg (Eti, Pathophys, CP, Diagnostics, Tx,
|
*Eti: Leaflet Problem, Chordae tendinae problem, Changes in LV geometry, annual problem, Myxomatous
*Pathophys: TWO FLAVORS ACUTE: tachycardia, hypotension, PE. Low forward stroke volume. Emergency! CHRONIC: Long asymptomatic period. CP: ACUTE: tachy, hypotension, PE CHRONIC: SOB, fatigue, weakness, displaced PMI, holosystolic murmur radiates to axilla, Tx: REPAIR INSTEAD OF REPLACE. Surgery indicated if symptomatic or decline in LV function |
|
|
Indications for surgical repair of valvular heart disease
|
MITRAL REGURGITATION seems to be the main disease to repair since mortality is lower.
|
|
|
Pulmonic Regurg (Eti, Pathophys, CP, Diagnostics, Tx, Natural Hx)
|
*Eti: pulmonary hypertension, endocarditis, CONGENITAL
*Pathophys: Causes RV volume overload. But WELL TOLERATED and not a huge deal. *CP: Diastolic decrescendo murmur at LUSB, increased w inspiration Tx: Surgery Rarely Required. |
|
|
Tricuspid Regurgitation (Eti, Pathophys, CP, Diagnostic, Tx, Natural Hx)
|
Eti: Usually secondary to RV dilation and/or pulmonary hypertension.
Pathophys: Causes RV volume overload. WELL TOLERATED CP: Neck vein distension, Holosystolic murmur. Tx: Surgery occasionally required. |
|
|
Mitral Valve Prolapse (Eti, Pathophys, CP, Diagnostic, Tx, Natural Hx)
|
Eti: Cause often unknown. Associated with diseases of connective tissue
CP: Most imporant is mid-systolic click Tx: Beta blockers sometimes relieve chest pain and palpataions. Mitral valve repair if symptomatic from mitral regurg. |
|
|
Types of valve repairs/replacements
|
*Mechanical prosthetic valve (excellent longetivity, require lifelong anticoag
*Biologic/tissue valve - porcine, bovine, human. No anticoag required, limited lifespan. |
|
|
Mechanisms that control BP
|
*CARDIAC OUTPUT: Heart Rate & Stroke Volume
*PERIPHERAL RESISTANCE: Arteriolar Vascular Tone, Neurological, Hormonal |
|
|
Incidence and prevalence of hypertension in US
|
* 90-95% is primary (essential). 5-10% is secondary (e.g. renal arterial sclerosis -> hyperaldosterone).
* 50 million individuals in US (1 in 5). * Blacks more than whites. |
|
|
Classification of HTN
|
Normal <120 and <80
Prehypertension 120-139, 80-89 Stage 1 HTN 140-159, 90-99 Stage 2 HTN >160, >100 |
|
|
Genetic Dyslipidemia Syndromes & it's CP
|
*Familial Hypercholesterolemia - Liver doesn't recognize LDL in blood and makes more and more. Tendinous Xanthomas, xanthelasma is a sign. LDL > 190 (>160 in kids), and a family Hx of CAD.
*Familial Hyperchylomicronemia - Abnormality of the enzyme that enables peripheral tissues to take up triglyceride from chylomicrons and VLDL. -> Marked hypertriglyceridema with recurrent pancreatitis and hepatosplenomegaly in childhood |
|
|
Secondary Causes of Dyslipediams
|
DM, alcoholism, nephrotic syndrome, smoking, diet, thiazide diuretics, beta blockers, hyper/hypothyroidism
|
|
|
Risk Factors for Dyslipidemia
|
*Cigarette smoking
*HTN *HDL < 40mg *Family Hx of premature CHD Age > 45 male. Age > 55 female |
|
|
LDL Physiology
|
Cholesterol is carried to the arteries by LDL's. LDL's are produced by the liver. They're a small protein-coated droplet of cholesterol, fat, and other lipids.
|
|
|
Lifestyle modifications to improve blood lipid disorders
|
*Diet (decrease fat, increase plants & fiber)
*Physical Activity *Weight Loss *Eliminate Smoking |
|
|
Lipid Management Guidlines & Steps
|
1) Bring LDL-C into check (via lifestyle then statins)
2) Bring Non-HDL Cholesterol under raps. Non-HDL goal is LDL goal + 30. Try lifestyle changes. Or add fibrate or niacin 3) Consider treating HDL after above goals are met. |
|
|
Laboratory evaluation of dyslipidemias to include
1) Total Cholesterol 2) LDL 3) HDL 4) Triglycerides |
LDL is Total Cholesterol - HDL. Has to be fasting for accurate TG and LDL.
1) Total < 200 2) LDL <100 (or 70) 3) Above 40 4) Above 1000 puts you at risk for pancreatitis |
|
|
Why are lipids deposited into the cells of arteries?
|
Unknown!
|
|
|
When do you refer a patient with lipid disorders?
|
* Known Genetic lipid disorders
* Striking family Hx of hyperlipidemia or premature atherosclerosis * Extremely high LDL & triglycerides or extremely low HDL |
|
|
BP Goals for uncomplicated HTN, DM, CKD
|
HTN - 140/90
DM & CKD - 130/80 |
|
|
CHD Equivalents on Calculating Framingham Risks & LDL Goals
|
* DM
* PVD (peripheral vascular disease) * Cerebrovascular Disease * AAA * Symptomatic Carotid Artery Disease * Chronic Renal Failure |
|
|
Framingham Major Risk Factors
|
* Cigarette Smoking
* HTN >140/90 and/or taking antihypertensive meds * HDL < 40 * Family Hx of premature CHD - Male < 55 - Female < 65 * Age - Male > 45 - Female > 55 |
|
|
NCEP/Framingham Guidelines
|
1) CHD/Risk Equivalent?
*YES, go to GOAL CHART *NO, go to next step 2) Add Major Risk Factors *0-1 = go to GOAL CHART *2+ = calculate Framingham score 3) Determine LDL Goal from Framingham score |
|
|
Alternative supplements to improve blood lipid levels
|
*Niacin - reduced VLDL production with secondary reduction in LDL. Increase IN HDL
* Fish Oil - Decrease TG * Plant Sterol Esters - Cholesterol Lowering * Red Rice Yeast |
|
|
Measurement and use of lipoprotein a (LPa), homocysteine, and C-reactive protein in evaluation and management of dyslipidemias
|
These are additional risk factors that have been studied with hopes to better predict CHD events.
(Info in Current limited to this) |
|
|
Dietary guidelines for lowering blood cholesterol and triglycerides
|
* Eat low fat/cholesterol foods.
* Mediterannean Diet - lowers LDL, raises HDL * Fiber reduced LDL * Garlic, soy protein, vitamin C, pecans, plant sterols reduce LDL * Foods rich in antioxidants (plants & vegetables) kill oxidized LDL |
|
|
Creatine Kinase (CK) as a Cardiac Enzyme
|
* Found in all striated muscle, but useful in detecting acute MI.
|
|
|
CK-MB isoenzyme as a Cardiac Enzyme
|
* It is specific to heart muscle
* There is a delay however. It will be negative until 4 hours in. * Peaks at 18 hours * Normal in 24-48 hours |
|
|
*Troponin I & T as Cardiac Enzymes
|
* Contractile protein of muscle cells
* Marker of choice for R/I of acute MI * It increases in 4-6 hours and returns to normal in 4-10 days * Troponin I = most common * Tropnon T = research? |
|
|
Progression of Markers through time for Acute MI
|
* Myoglobin is first marker (Not specific to MI however)
* CK is next * Troponin is last * Check them serially (every 3 hours) |
|
|
P Wave on EKG
|
Atrial Contraction
|
|
|
PR interval
|
AV node delay to allow atria to finish contractions
|
|
|
QRS
|
Bundle of His -> Bundle Branches -> Purkinje Fibers. Ventricular Contraction
|
|
|
Clinical Usefulness of an EKG
|
* Graphic tracings of heart's electrical activity
* Acute cardiac events: MI, Arrythmias * Hypertrophy & chamber enlargement * Conduction abnormalities * Other conditions: hypertension, COPD, electrolyte abnormalities, drug effects |
|
|
Brain Natriuretic Peptide (BNP) Usefulness
|
* Used to evaluate for CHF
* Called "brain" because they originally thought it came from the brain * Increased in heart failure with increased filling pressures |
|
|
Different cardiac imaging techniques
|
* Chest X-Ray
* Echocardiogram * Cardiac catheterization * MRI/CT |
|
|
Chest X-Ray of Heart Usefullness
|
* Overall heart size
* Pericardial effusion * Size & location of aortic arch & pulmonary vessels * Calcifications in aorta walls * Heart Failure * Heart shouldn't take up more than 50% of thoracic cavity |
|
|
Echocardiography usefulness
|
* Images of moving heart chambers, valves
* Doppler assesses direction & velocity of blood flow within heart & vessels * Get: cardiac chamber sizes and dimensions, pressures, pericardial effusions, masses, ischemia during stress testing |
|
|
Echocardiography advantages & limitations
|
Advantages:
Little discomfort, info about both heart structure & function, no radiation Limitations: Chest wall abnormalities, COPD, movement, user error |
|
|
Cardiac catheterization Usefulness
|
* Both diagnostic & therapeutic
* Contrast material provides direct info of CAD and severity * Gets pressure information of vessels and chambers |
|
|
Indications for Cardiac Cath
|
*Acute MI, angina, high risk, coronary artery dz, cardiomyopathy
|
|
|
Contraindications for Cardiac Cath
|
* Reaction to contrast material
* Renal failure * GI bleeding * Severe anemia * Recent Stroke * Advanced noncardiac dz |
|
|
Cardiac Cath Potential Complications
|
* Stroke
* MI * Dissection of vessel wall * Hemorrhage * Acute renal failure |
|
|
MRI
|
* "Useful in looking at zebras"
* Aortic dissection, thrombi, masses, pericardial dz, etc * Limitations: $$$, stents (metal), availability, |
|
|
Electron Beam CT Scan
|
* DETECTS CALCIUM DEPOSITS IN ARTERY WALLS
* CALCIUM SCORE GOOD ESTIMATE OF PLAQUE BURDEN -> early indicator of atherosclerosis * Very sensitive.(but not very specific) --> negative predictive value high. -> If you test negative, you probably don't have it. But if you test positive, it's not very specific so it could be other things. |
|
|
Cardiac CTA Usefullness
|
* This is a CT scan of cardiac arteries. Problem is you can't do anything about problems since you would have to go in and cath anyways.
* High radiation exposure. |
|
|
Exercise Tolerance (stress) Testing
|
* Patient stressed by exercise (tradmill, bicycle) to 85% of max HR
* 12 lead EKG monitored for ischemic changes (ST depression) * Useful to diagnose ischemia, antianginal therapy efficacy, stage valve replacement |
|
|
Explain "pretest probability" for exercise testing in cardiac disease evaluation
|
* Helps determine if exercise testing will be a useful screening tool for a particular patient.
* High pretest probability in population with risk factors, older patients, with anginal symptoms * Low probability in young, ASx patients |
|
|
Contraindications for Exercise Tolerance Testing
|
* Acute phase of MI
* Unstable angina * Heart failure * Serious arrhythmias * Symptomatic Aortic valve disease * Severe HTN (200/120) * Severe cardiomyopathy * R or L bundle branch block * Hypo/hyperkalemia |
|
|
Pharmacologic Stress Echo Usefullness in cardiology studies
|
positive inotropic and chronotropic drugs instead of actually excercising. Treadmill is always better.
|
|
|
MUGA (Multigated Acquisition Scan) Usefullness in cardiologic studies
|
* This has largely been replaced by echo.
* But it is the GOLD STANDARD for looking at EjFraction. * It is an exercise and rest radionuclide scan (nuclear medicine) * It tells LV and RV function |
|
|
Holter Monitor in arrhythmia evaluations
|
* An ambulatory recording of EKG over 24 hour period
* Indications: palpatations or syncope, evalute efficacy of antiarrhythmic drug therapy, identify painless ischemia |
|
|
Event Monitor in arrhythmia evaluations
|
* Saves several minutes of rhythm when activated by patient while experiencing Sx.
* Smaller than Holter, less cumbersome. Can be worn longer. Can send results over phone! |
|
|
Electrophysiology Study clinical Usefulness
|
*Sort of an EKG via heart cath.
*Indications: -Confirmed arrhythmias or abnormal ECG -Persistent arrhythmias symptoms -Severe cardiomyopathy for AICD implant -Abnormal ambulatory monitoring. |
|
|
Tilt-Table Testing Usefulness
|
*To check BP problems
*Lay down, measure BP & HR. Stand up |
|
|
C-reative protein clinical usefulness
|
Marker of inflammation
|
|
|
Homocysteine clinical usefulness
|
Predictive of dyslipidemia atherosclerotic disease.
|
|
|
Criteria to be in and LDL Goals for:
Very High Risk High Risk Moderately High Risk Moderate Risk Lower Risk |
*VHR - ACS, CHD w/DM, CRF <70
*HR - CHD or CHD risk equivalents, or 10-year risk>20%...<100 (<70) *MHR - 2+ risk factors, 10-year risk=10-20, <100 *MR - 2+ risk factors, 10-year risk <10...<130 LR - 0-1 risk factors, <160 |
|
|
T Wave
|
Ventricular Repolarization
|
|
|
P Wave
|
Atrial Depolarization
|
|
|
QRS Complex
|
Ventricular depolarization
|
|
|
PR Interval
|
From start of atrial depolarization to start of ventricular depolarization. Pause in the AV node
|
|
|
Axes on EKG tracing
|
Horiz - time
Vert - voltage (mV) |
|
|
ST Segment
|
The plateau phase of the cardiac action potential
|
|
|
QT interval
|
Reresents to start of ventricular depolarization to end of repolarization
|
|
|
Anterior Leads of Heart
|
V1-4
|
|
|
Lateral Leads of Heart
|
I, AVL, V5-6
|
|
|
Inferior Leads of Heart
|
II, III, AVF
|
|
|
Describe normal sinus rhythm (NSR) criteria
|
*Normal rhythm of heart
*SA -> AV -> Bundle of His -> Purkinje Fibers * 60-100bpm Sinus bradycardia < 60 Sinus tach > 100 * "Sinus" because its from the SA Node |
|
|
Premature Atrial Contractions
|
* Early beet from ectopic pacemaker
* May be normal, stress, drugs, disease CP: asympt. or palpatations |
|
|
Supraventricular Tach
|
* "racetrack short circuit" "trashcan diagnosis".
* ectopic atrial focus. overrides SA Node * rhythm strip implies that all iimpulses get through AV node and have ventricular influence, unlike a flutter. * Eti: stress, hypoxemia, drugs, atrial septal defect CP: palpatations, lightheadedness, syncope |
|
|
Atrial Flutter
|
*Atrial impulses stuck in "short circuit"
*AV Node can not conduct all impulses * Atrial rate 280-340 *Eti: CAD, MI, Pulm Embolism, lots more heart problems. CP: Palpatations, SOB, Syncope, CVA/TIA |
|
|
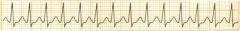
Supraventricular Tach
|
|
|
atrial fib
|
* Random chaotic atrial activity. Unlike A flutter which seems not random but regular.
*"bag of worms" *Simultaneous discharge of multiple atrial foci *Etiology: CAD, valve disease, CO poisoning, lots lots more *CP: Palpatations, fatigue, dizziness, asymp , CHD, etc...... |
|
|
classic sawtooth pattern
|
atrial flutter
|
|
|
complications of Atrial fibrilation
|
*Low cardiac output from loss of cardiac kick
*cardiomyopathy with "RVR" * CVA |
|
|
Treatment of Atrial Fibrilation (and also Atrial Flutter)
|
*Treatment goals include rate vs rhythm control:
RATE: control ventricular rate to allow ventricular filling. Beta Blockers, CaChannel Blockers, Digoxin. Use Coumadin to avoid clots. RHYTHM: anti-arrythmics. Studies show RATE control is better. * Goals include abolishing precipitants, reducing symptoms, reducing complications, lengthen survival. |
|
|
Premature ventricular tach
|
*Ectopic beat from ventricular
*Eti: idiopathic, stimulants, the same same stuff.. CP: Palpatations, nothing... No P Wave since it's ventricular in origin. Then a forceful beat from Frank-Starling concept. People are aware of that beat. Wide QRS since its not on main conduction system |
|
|
Ventricular Tachycardia
|
*Serious rhythm underlying heart Dz
*Irritable focus in ventricle. *Kind of like AFlutter of ventricles *Etiology: Ischemic CAD, S/p MI, cardiomyopathy CP: Syncope, Palpatations, Sudden Cardiac Death |
|
|
Ventricular Tach Tx
|
Stable: Antiarrhythmics, treat underlying etiology
Unstable: ACLS (shock, antiarrthymics, CPR) |
|
|
Arrhythmogenic right ventricular cardiomyopathy
|
* GENETIC condition of localized scarred areas with fibrofatty replacement
*New tissue is very electrogenic (creates its own impulses) *Tx: AICD, Beta Blockers, famil screening |
|
|
QT Prolongation
|
*GENETIC or secondary to medication
*Can lead to lethal arrhythmia since the delay makes heart more vulnerable to outside impulses |
|
|
Ramano Ward & Andersen Brugada syndromes
|
These are congenital causes of long QT syndrome
|
|
|
Most common cause of Native Valve Non-IV Drug User Endocarditis
|
Viridans streptococci
|
|
|
Most common cause of Native Valve IV Drug User Endocarditis
|
Staph aureus
|
|
|
Most common cause of Prosthetic Valve Endocarditis
(EARLY & LATE) |
Early - Staph aureus
Late - Viridans streptococci |
|
|
What is definitive test for valvular disease?
|
*Echo if the cause can be clearly suspected and elucidated (Mitral stenosis if Hx of rheumatic fever. Aortic stenosis if elderly
*Cath with valvular biopsy/culture if you can't suspect cause. |
|
|
Ischemia (cell injury) can be seen how on an EKG Tracing?
|
ST Elevation or ST Depression
|
|
|
Thiazides are not recommended in which hypertensive patients?
|
In DM patients since they raise blood sugar levels.
|
|
|
Eti & Clinical presentations of long QT syndromes
|
Eti: Congenital. Ramano Ward, Andersen Brugada
CP: Normal QT should be less than 50% of R-R length. *Syncope, chest pain, palpitations. "R on T". Associated with a trigger (lound sound, etc) |
|
|
Vtentricular Fibrillation
|
* Multiple irritable foci in the ventricles
*Chaotic rhythm, irregular * EMERGENCY! Most common cause of sudden cardiac death. *Tx: Defib, Drugs, CPR, ACLS |
|
|
Idioventricular Rhythms
|
*Think slow VTach.
*"Ventricular Escape Rhythm" Tx: Pacemaker, Atropine, Domapine |
|
|
First Degree Heart Block
|
* Prolonged PR interval > 0.2 seconds
* Takes longer for impulse to get to ventricles. CP: Usually assymptomatic. |
|
|
2nd Degree Heart Block, Type I
|
Progressive lengthening of PR interval until QRS dropped. Block occurs at AV Node
Eti: vagal stimulation, degenerative, ischemic heart disease, drugs (BB, CCB, digitalis), MI CP: Usually asymp. Irreg pulse w dropped beats |
|
|
2nd Degree Heart Block, Type II
|
*Sudden interruption of AV conduction w/o prior prolongation
*Periodic non-conducted P wave *Rate and more serious *Eti:Degenerative, MI, Calcified aortic stenosis |
|
|
Source of Second Degree heart blocks (Type I & II)
|
AV Node!
Type 1 - progressive prolongation Type 2 - Sudden, periodic interruption. Rare and more serious |
|
|
2nd Degree Heart Block Type II CP & Treatments
|
CP: irregular pulse with occasional dropped beats, sudden LOC
Tx: Pacing, +/- atropine |
|
|
Third Degree Heart Block
|
Complete disassociation between atria & ventricles
Eti: Lyme Disease, Degenerative, MI, other usuals CP: Dizziness, palpataions, Stokes-Adams syncope, CHF-SOB, angina Tx: Treat cause, pacing. |
|
|
Most common cause of secondary hypertension
|
Renal Artery Stenosis
|

