![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
115 Cards in this Set
- Front
- Back
|
WHat percent of people with HTN are under control?
|
34%
|
|
|
Name the classic two Thiazide diuretic
|
HCTZ
metolazone |
|
|
Name the four classic Loop diuretics.
|
furosemide
bumetanide torsemide ethacrynic acid |
|
|
Name the classic two thiazide-like duiretics
|
chlorthalidone
indapamide |
|
|
Name the classic 4 K+ sparing diuretics
|
triamterene
amiloride spironolactone eplerenone |
|
|
ending for ACE inhibitors
|
-pril
eg. lisonopril |
|
|
ending for ARBs
|
-sartan
|
|
|
1) ending for Ca++ channl antagonists
2) two exceptions to this nomenclature |
1) -ipine
eg. nifedipine 2) diltiazem, verapamil |
|
|
Two classic vasodilators
|
hydralazine
minoxidil |
|
|
ending for Alpha1 antagonists
|
-osin
i.e. prazocin |
|
|
Two common alpha2 agonists
|
clonidine
methylodpa |
|
|
ending for Beta Blockers
|
-lol
i.e. porpranolol, metoprolol |
|
|
Two classic sympatholytics
|
Reserpine
Guanethidine |
|
|
1)How do Diuretics change the pressure-natriuresis curve?
2) how does this effect systemic vascular tone? |
1) shift to the left
2) long term vasodialtion |
|
|
Thiazide Diuretics:
1) inhibit what? 2) Where? |
1) Na/Cl cotansporter
2) DCT |
|
|
Loop Diuretics:
1) inhibit what? 2) Where? |
1) Na/K/2Cl co transporter
2) TALH |
|
|
K+ Sparing diuretics:
1) What does Amiloride inhibit? 2) Where? 3) How does spironolactone act? 4) Where? |
1) ENaC channels
2) DCT 3) Competitive inhibitor of aldosterone, preventing insertion of aldo-sensitive Na+ Channels 4) DCT |
|
|
Actions of Aldosterone on:
1)Na+ 2) volume 3) vascular compliance 4) Endothelium 5)Pressor Responses of AII 6) Vasc. Smooth Muscle Cells 7)Kidneys, heart, vasculature 8) Coagulation 9) Effect on AII signalling 10) growth 11)ROIs 12) Hypertrophy of? 13)blood lipids 14) ___kalemia 15) ____Magnesemia |
1) Retention
2) Volume expansion 3) Reduction in vascular compliance 4)Endothelial Dysfunction 5) Potentiation of Pressor Responses from AII 6) Increase SM Na|+ influx 7) kidney, heart, vessel fibrosis 8) actiate plasminogen activator INHIBITOR (pro-thrombotic) 9) Upregulate AII receptors 10) stim. TGF-B1 11) increase ROIs 12) Hypertrophy of VSMC and myocardium 13) increased blood lipids 14) Hypokalemia 15) HypoMagnesemia |
|
|
1) what does renin do?
2) What blocks this directly? |
1) converts Angiotensiogen to angiotensin
2) Renin receptor blockers |
|
|
1) What does ACE do?
2)What blocks this directly 3) What alternate pathwat can circumvent this blockage |
1) Convert AI to AII
2) ACE inhibitors 3) Non-ACE conversion with CAGE, chymase, Cathepsin G |
|
|
1)What does AII bind?
2)What blocks this? 3What are the three downstream events of this binding event? |
1) AT1 receptor
2) ARBS 3) Vasoconstriction, Aldosterone secretion, sympathetic activation |
|
|
ACE inhibitors:
1) Cause lowered BP how? |
1) Decreased AII- vasodialtion
Decreased Aldo- Natriuresis Less sympathetic activation Decreas endothelin and inmprove endothelial function |
|
|
terminal elimination phase of ACE-inhibitors
|
renal or renal/hepatic
|
|
|
ACE-inhibitor dosing
|
multiple regimens with variable trough to peak ratios
|
|
|
Racial variation of ACE-inhibitor actvity
1) doesnt work as well in... 2) Why? 3) solution? |
1) blacks
2) Low renin levels 3) use a higher dose |
|
|
ACE-inhibitor with a short half live
|
Captopril
|
|
|
Indication for an ACE-inhibitor?
|
Diabetic Nephropathy
|
|
|
1)A pt. with diabetic nephropathy and HTN should get what class?
2) why? |
1)ACE-inhibitor (-pril)
2) Dilated efferent arteiole which drops GFR (increase creatinine by less than 30%) |
|
|
Contraindications to ACE-inhibitors as a class
|
1) Angioedema
2) 2nd or 3rd trimester (teratogenic?) 3) Renal Artery Stenosis of stenosis in a solitary kidney (concerned if Creatinine goes up more than 30%) Baseline serum creatinine elevation is NOT a contraindication |
|
|
One side effect of ACE-inihibitors eliminate a large age group from ever getting this drug, which group and why?
|
Teens, because ACE-inhibitors are teratogens and teens will not tell you if they are pregnant.
|
|
|
A pt. has baseline serum creatinine elevation, but no renal artery stenosis. Can this pt. have ACE inhibitors?
|
Yes
|
|
|
ACE- inhibitors:
6 side effects that are class effects: 1) BP 2) Respiratory 3) Immune 4) Renal 5) ___ Kalemia 6) Blood |
1) First does hypotension if volume depleted
2) COUGH 3) Angioedema 4) Functional Renal insufficiency 5) Hyperkalemia 6) Anemia due to erythropoetin chnages |
|
|
ACE- inhibitors:
Two side effect specific to captopril |
Taste disturbnces and Rash
|
|
|
ACE-inhibitors:
1) If your patient develops a cough on this drug,what ca you switch them to? 2) Why did they develop this cough? 3) If a pt. on this drug develops functional renal insufficiency what do you do? |
1) ARB
2) Increased Bradykinin metabolism to cough inducing compounds 3) stop temporarily |
|
|
Effects of AII:
1) Kidney 2)CNS 3) adrenal 4) Vascular |
1) renal vasocnstriction; Increased Na and H20 reabsorption; Inhibits Renin secretion
2) Sympatheic ouflow: ADH Secretion 3) Increases Aldo synthesis and secretion 4) Vasoconstriciton, Decreases NE reuptake |
|
|
Mechanism of ARB action:
Decreases three parameters which all sum to lower BP. Name them. |
Decreases Aldo secretion
Decreases Vasoconstriction Decreaed Sympathetic activation |
|
|
How do the AT1 and AT2 receptors differ?
1) expression 2) Absorbtion of sodium 3) Vascular tone 4) cell growth regulation |
1) AT1 Always expressed, T2 only expresed during stress or injury
2) AT1 increases, AT2 decreases 3) AT1- vasoconstrict; AT2- vasodilate 4) AT1- activate AT2- inhibit |
|
|
Limitation of ARB usage?
|
Price
|
|
|
1) Alliskerin (Tekturna) is what kind of drug?
2) Why is it not widely used yet? |
1) Direct Renin Inhibitor
2) very new, not much outsomes data out yet |
|
|
Vasopeptidase inhibitors:
1) Upside? 2) downside? |
1) VERY effective
2) Large rate of angioedema especilly in AAs |
|
|
1) What kind of Ca++ channels doe Ca++ channel blockers work at?
2) What normally activates these channels? 3) What substrates can cause Ca++ influx in other types of ligand gated channels? |
1) L-type
2)Voltage 3) endothelin, AII, NE |
|
|
There are three classes of Ca++ blockers. Two of them only contain one drug that is relevant, and the last one is a larger class. Name all of them and give an example.
|
1) Phenylalkylamines: verapamil
2) Benzothiazeprines; Diltiazem 3)dihydropyridines; -ipine ending |
|
|
What is a major effect of the non DHP (verapamil, diltiazem) Ca++ channel blockers that is not present in the DHP drugs?
2) Which one does this more? |
1) Negative Inotropy
2) Verapamil |
|
|
Mechanism of Ca++ channel blocker action:
|
Decreased Ca++ entry
Negative inotropy (non-DHP) Dec. PVR Natriuresis Interference with AII, alpha1, and alpha2 mediated vasoconstriction |
|
|
How does the mechanism of Ca++ channel blockers intersect with the RAAS system and sympthetic nervous system
|
Interference with AII, alpha1, and alpha2 mediated vasoconstriction
|
|
|
Indications for Ca++ channel blocker usage (any class):
|
All forms of hypertension
Salt sensitive hypertension |
|
|
Indications for Ca++ channel blocker usage (Non-DHP):
|
HTN with diastolic dysfunction ( poor relaxation) will benefit from the negative inotropy of the non-DHPs
|
|
|
Indications for Ca++ channel blocker usage (DHP specifically):
|
To prolong half-life of cyclosporine
|
|
|
One Absolute Contrandication for Ca++ channel blocker usage (non-DHP):
|
1) Partial AV nodal block because of negative inotropy, could put then in complete heart block
|
|
|
One relative contraindication for Ca++ channel blocker usage (non-DHP):
|
Comcomitant use of Beta-blockers because of synergistic negative inotropy
|
|
|
these are side effects of what class?
Headache Peripheral Edema Gingival hyperplasia |
Ca++ channel blockers
|
|
|
SIde effects for Ca++ channel blocker usage (DHP only):
|
Tachycardia (especialy with Nifedipine
We do not know why this happens |
|
|
Side effects for Ca++ channel blocker usage (Verapamil only [phenylalkylamine]):
|
Constipation
|
|
|
Side effects for Ca++ channel blocker usage (non-DHP only):
|
CHF
|
|
|
Side effects for Ca++ channel blocker usage (short acting DHP only):
|
Acute MI
|
|
|
Peripheral edema is a side effect of all Ca++ channel blockers. Why does this happen?
|
Caused because these drugs are more effective arterial vasodilators rather than venous vasodilators.
Not a function of volume retention |
|
|
1) Name the two Direct vasodilators
2) Mechanism of action? |
1)Hydralazine
Minoxidil 2) unknown |
|
|
Reflex response from body to Direct vasodilators?
|
activation if sympathetic NS, and RAAS loop
|
|
|
1)Direct vasodilators Indicated for what group of patients?
2)Minoxidil indicated for what more specific subset? |
1) Pt. needing multidrug therapy with resistant hypertension
2) Refractory pateints with RENAL INSUFFICIENCY |
|
|
Direct vasodilators as a first line therapy?
|
Really never, should be the 5th or 6th drug tried
|
|
|
Direct Vasodilator Contraindication
|
Pericardial Effusion
|
|
|
Side effects of Direct Vasodilators
1) as a class 2) just for minoxidil |
1) Fluid retention
Tachycardia Lupus-like syndrome 2) Pericardial effusion/tamponade Hyypertrichois |
|
|
Why must vasodilators only be used in multi-drug therapy?
|
Need others to combt all of the side effects
|
|
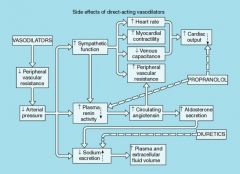
Answer is a diagram of the side effects of direct vsodilators and how they are countered by two drugs. This about the diagram, and name the two drugs and the side effects they counter.
|
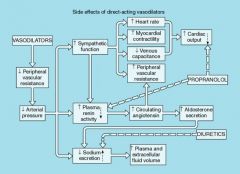
Propranolol (Beta-blocker) counters Tachycardia, and renin activity (this is just beta1 activity, so could probably use metoprolol)
Diuretics counter the sodium and volume retention |
|
|
1) 140/90 is the target BP when:
2) 130/80 is the target BP when: |
1) no evidence if complication (except high cholesterol
2) HTN with increased CV risk (i.e diabetes, Hx of MI; LVH; nphropathy; CHF, TIA/CVA) |
|
|
1) Alpha1 antagonists mechanism?
2) Reflex reaction of the body? |
1) Block peripheral α1-receptors causing direct arterial vasodilatation
2) Reflex activation of sympathetic nervous system in a dose-dependent fashion |
|
|
Alpha1 blockers:
1) effect on RAAS axis? 2) Positional effects? |
1) Minimal
2) More effective upright than supine |
|
|
Alpha1 blockers:
1) Especially indicated in what population in why? 2) Side effect in women? |
1) men with BPH because relaxes bladder neck
2) incontinence |
|
|
Prototypical Aplha-1 antagonist?
|
Prazosin (-osin drugs)
|
|
|
Indications for Alpha1 antagonist therapy?
|
1)Pt. requiring multidrug therapy
2)HTN complicated by metabolic abnormality like diabetes, insuil resistance, and hypercholesterolemia 3) BPH |
|
|
Side effect of Alpha1 antagonists?
|
Fluid retention, orthostasis, incontinence in women, lethargy, fatigue, dizziness, headache, first-dose hypertension
|
|
|
2 prototypical Central Alpha-2 agonists
|
clonidine, methyldopa
|
|
|
Alpha-2 agonists mechanism of action
|
Decreased sympathetic nervous system activity and lowered plasma renin activity by central α2-adrenergic receptor stimulation
|
|
|
Indications for central alpha-2 agonist
|
Resistant HTN
Anxiety driven HTN Perioperative HTN (analgesia and anesthesia sparing property) |
|
|
What class would you use for anxiety driven HTN?
|
aplha2 agonist
|
|
|
What cal would you use for perioperative HTH and why?
|
Central alpha-2 agonist- analgesia and anesthesia sparing property
|
|
|
1) What is the only drug that is actually indicated for HTN in pregnancy?
2) What drug is ACTUALLY used by Obstetricians in this case? |
1) methyldopa
2) nifedipine (DHP Ca++ blocker) |
|
|
Central Nervous pathway of Alpha-2 agonist meidating BP reduction
|

|
|
|
1)Side effect of all central aplha-2 agonists?
2) Side effect of just Clonidine? 3) side effect just of Methyldopa? |
1) fluid retention- dose dependant
bradycardia- dose dependant 2) sedation, dry mouth, skin iritation (transdermal) 3) autoimmune hemolytic anemia and hepatitis |
|
|
1) Major danger of Clonidine perscription
2) When is the probelem even more dangerous than normal? 3) how do we handle this |
1) Rebound hypertension if the drug is stopped suddenly
2) concomitant B-blocker 3) wean 30% per week until .1 mg/day and do not prescribe to unreliable people |
|
|
Beta Blockers: mode of action
(this is just speculative, we dont REALLY know) |
Reduce CO
Inhibit Renin release Direct CNS effect Alteration of catecholamine release or response |
|
|
Beta blockers:
1) Labetelol and carvediol are special, why? 2) Nebibolol is special, why? |
1) Beta and aplha1 antagonism, so they also lower PVR
2)Cardioselective vasodilator as a result of increased NO levels |
|
|
ALL beta b lockers except Nebibolol do what?
|
Decrease CO
|
|
|
SOme beta blockers have Intrinsic Sympathomimetic acitivty. We call these ISA Beta-blockers.
1) Three ISA B-blockers 2)In what sense are these Beta-blockers sympathomimetics? antagonists? |
1) propranolol, acebutolol, pindolol
2)They have a partial agonist acitivity at Beta1 and/or Beta2. Thas has little consequece in the absence of SNS input, but can act as as antagonists when the strong agonists like Epi and NE are released here. |
|
|
1) The mixed alpha1 and Beta blocking carvediol make them useful in treating HTN complicated by_____.
2) This alpha activity has what effect on C.O. |
angina
2) reduces PVR, which maintains CO while lone beta antagonists drop CO. |
|
|
Beta Blockers: Indications
|
uncomplicated HTN
Isolated Systolic HTN Pulse rate dependent HTN HTN with symptomatic CAD CHF Essential Tremor |
|
|
Beta Blockers: Contraindications-- Tell me why these are contraindications:
1) Bronchospasm 2) Decompensated CHF 3) Heart block, Sick Sinus 4) Insulin Dependant DM (relative contraindication) |
1) B2 blocker cuses bronchoconstriction- dont use non-selectives or B2 selelctives at HIGH doses)
2) Decompensated CHF due to decrease in C.O. 3) A.V. Nodal blockers 4) Blunts the symptoms of hypoglycemia ( tachycardia, tremor) |
|
|
Beta Blockers: Side effects
|
Bronchospasm
Heart Block Worsening CHF High triglycerides or Low HDL Mask hypoglysemia in IDDM Depression or nightmares Poor sleep |
|
|
Sympatholytics mechanism of action
|
Lower BP by depelting NE from presynaptic storage granules
|
|
|
Sympatholytics: Indication
|
Resistant HTN
|
|
|
Sympatholytics: Drug-Drug interactions
1) MAOI 2) TCAs |
1) Hypertensive crisis
2) Decreased hypotensive effect |
|
|
Sympatholytics: Side effects
1) HEENT 2) stomach 3) GI 4) GU 5) Psych |
1) stuffiness
2) gastric acidity 3)diarrhea 4) retrograde ejaculation 5) depression |
|
|
Definition of resistant HTN
|
BP which is not controlled despite pt. being on 3 drugs at maximal doses, one of which is a diuretic
|
|
|
Most people require __ drugs to control HTN
|
3
|
|
|
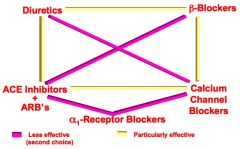
Particularly effective combinations of Antihypertensives:
Use Diuretics with- |
B blockers
ACE-I/ARB |
|
|
Particularly effective combinations of Antihypertensives:
Use Beta Blockers with |
Diuretics
Ca++ Channel Blockers |
|
|
Particularly effective combinations of Antihypertensives:
Use Ca++ Channel blockers with |
B Blockers
ACE-I/ ARB |
|
|
PArticularly effective combinations of Antihypertensives:
Use ACE Inhibitors and ARBs with |
Diuretics
Ca++ Channel Blockers |
|
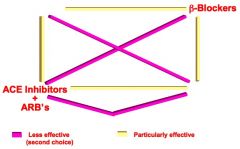
Fill in the blanks
|
|
|
|
Algoritihim for Treatment of HTN
|

|
|
|
Initial Drug Choice-
Uncompliated HTN |
thiazide
|
|
|
Initial Drug Choices-
CHF |
ACE inhibitors
Diuretics (Loop) |
|
|
Initial Drug Choices-
1) HTN with MI 2) HTN with MI with systolic dysfunction |
1) Non ISA - beta blockers
2) ACE inhibitors |
|
|
Initial Drug Choices-
HTN with DM |
ACE inhibitors
|
|
|
Initial Drug Choices-
ISH in elderly 1) preffered 2) other |
1) diuretics
2) Long acting DHP Ca++ channel blockers |
|
|
HTN drugs with favorable effects on Angina
|
B-blockrs
Ca++ channel blokckers |
|
|
HTN drugs with favorable effects on
Atrial tach and Fib |
B- blockers
Non-DHP Ca++ channel blockers |
|
|
HTN drugs with favorable effects on CHF
|
Carvedilol
Metoprolol Losartan |
|
|
HTN drugs with favorable effects on
MI |
Non-DHP Ca++ Channel blockers
|
|
|
HTN drugs with favorable effects on Cyclosporine induced hypertension
|
Ca++ channel blockers
|
|
|
HTN drugs with favorable effects on
DM I with proteinuria |
ACE inhibitor
|
|
|
HTN drugs with favorable effects on DMII with proteinuria
|
ARBs
ACE-inhibitors are used to cuz cheaper and may work as well |
|
|
HTN drugs with favorable effects on Dyslipidemia
|
alpha1-blockers
|
|
|
HTN drugs with favorable effects on BPH
|
aplha1-blockers
|
|
|
Renal Insuficiency
|
ACE inhibitors
|

