![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
671 Cards in this Set
- Front
- Back
|
Which law states that as preload increases, the left ventricle distends during diastole and the stroke volume increases?
|
Frank-Starling Law
|
|
|
Frank-Starling law states that as preload _____, the ____ _____ distends during _____ and the stroke volume _____.
|
increases
left ventricle diastole increases |
|
|
What are 3 manifestations of atherosclerotic cardiovascular disease?
|
coronary heart disease
stroke peripheral arterial disease |
|
|
What is the leading cause of death in developed countries?
|
cardiovascular disease
|
|
|
What are 3 unmodifiable risk factors of cardiovascular disease?
|
older age
male sex family history |
|
|
What are 3 major modifiable risk factors of cardiovascular disease?
|
cigarette smoking
dyslipidemia hypertension |
|
|
What is a dominant risk factor for stroke?
|
hypertension
|
|
|
What are 5 other modifiable risk factors of cardiovascular disease?
|
physical activity
diabetes mellitus obesity EtOH psychosocial |
|
|
For diabetes mellitus, men with type II DM have ___x the risk, while women with type II DM have ____x the risk of cardiovascular disease
|
2
4 |
|
|
What is the cardinal manifestation of myocardial ischemia?
|
chest pain
|
|
|
What common symptom of CVD results from elevated left atrial and pulmonary venous pressures or from hypoxia?
|
dyspnea
|
|
|
What are 2 things that may cause hypoxia which may result in dyspnea?
|
pulmonary edema
intracardia shunting |
|
|
What are 2 things that chest pain from CVD is not related to?
|
position
respiration |
|
|
Is chest pain with CVD reproducible with palpation?
|
no
|
|
|
Is paroxysmal nocturnal dyspnea more specific for cardiac or pulmonary disease?
|
cardiac
|
|
|
What are 9 symptoms of cardiovascular disease?
|
chest pain
dyspnea orthopnea paroxysmal nocturnal dyspnea palpitations dizziness syncope cardiogenic syncope neurocardiogenic syncope |
|
|
What is loss of consciousness caused by impaired cerebral blood flow?
|
syncope
|
|
|
What symptoms of CVD most commonly results from sinus node arrest, AV conduction block, v-tach, or v-fib?
|
cardiogenic syncope
(few prodromal symptoms and recovery is usually immediate |
|
|
What is another name for neurocardiogenic syncope?
|
vasovagal syncope
|
|
|
What symptom of CVD has inappropriate increase in vagal efferent activity, precedent increase in sympathetic cardiac stimulation, and may follow a brief period of diaphoresis and presyncopal symptoms?
|
neurocardiogenic syncope
|
|
|
Which sign of heart disease suggests hypotension or a hyperadrenergic state such as during pericardial tamponade, myocardial infarction, or tachyarrhythmias?
|
diaphoresis
|
|
|
Which sign of heart disease may be seen in patients with severe CHF or other chronic low cardiac output states?
|
cachexia (muscle wasting)
|
|
|
Which sign of heart disease usually indicates anemia, but may also be from low cardiac output?
|
pallor
|
|
|
Which type of cyanosis is due to arterial desaturation caused by pulmonary disease, left heart failure, or right -to-left shunting?
|
central cyanosis
|
|
|
Which type of cyanosis is due to impaired tissue delivery of adequately saturated blood from low output, polycythemia, or peripheral vasoconstriction?
|
peripheral cyanosis
|
|
|
Does shock cause hypo/hypertension? Central/peripheral cyanosis? Why?
|
hyptension
peripheral cyanosis (needs to get as much oxygen to the vital organs) |
|
|
Which sign of heart disease most commonly results from peripheral vascular disease and may be accompanied by localized bruits?
|
diminished peripheral pulses
|
|
|
Which sign of heart disease indicates increased stroke volume; may be from aortic regurgitation, coarctation, patent ductus arteriosus?
|
exaggerated pulses
|
|
|
What is valuable sign of pericardial tamponade?
|
pulsus parodoxus
|
|
|
Which sign of heart disease has a decrease in SBP during inspiration > 10mmHg?
|
pulsus paradoxus
|
|
|
Which sign of heart disease shows amplitude of the pulse alternating with every other heartbeat; occurs with very depressed cardiac contractility or large pericardial effusions?
|
pulsus alternans
|
|
|
Which sign of heart disease has elevated central venous pressure in > 3 vertical cm?
|
jugular venous pulsations
|
|
|
Which sign of heart disease has increased central blood volume if >1cm with sustained RUQ pressure?
|
jugular venous pulsations
|
|
|
With jugular venous pulsations, tricuspid obstruction has occurred if _____ wave exaggerated and tricuspid regurgitation has occurred if large ____ waves are seen.
|
alpha
cv |
|
|
What type of lung sound may be heard with congestive heart failure?
|
rales/crackles
|
|
|
What type of lung sound may be heart with left heart failure?
|
wheezing or rhonchi
|
|
|
What is common in congestive heart failure; more frequent and/or larger on the right?
|
pleural effusions (transudative)
|
|
|
Which sign of heart disease usually indicates right ventricular hypertrophy, pulmonary hypertension, or left atrial enlargement?
|
parasternal lift
|
|
|
Which sign of heart disease may occur with myocardial hypertrophy, volume overload, or high-output states?
|
enlarged apical impulse
|
|
|
Which condition has a fixed split S2?
|
atrial septal defects
|
|
|
Which condition has a wide split S2?
|
RBBB (right bundle branch block)
|
|
|
What are 3 conditions that have absent split S2 (paradoxic splitting)?
|
aortic stenosis
left ventricular failure LBBB |
|
|
Which heart sound does ventricular gallop occur?
|
S3
|
|
|
Which heart sound does atrial gallop occur?
|
S4
|
|
|
Which sign of heart disease is from ventricular volume overload or impaired compliance?
|
S3 (ventricular gallop) and S4 (atrial gallop)
|
|
|
Which sign of heart disease represents ejections sounds?
|
clicks
|
|
|
Which sign of heart disease usually indicates vavular disease?
|
murmurs
|
|
|
Which sign of heart disease has palpable vibrations associated with a murmur and are always clinically significant?
|
thrills
|
|
|
Which sign of heart disease is commonly caused by right heart failure?
|
edema
|
|
|
What is the most common cause of right heart failure?
|
left heart failure
|
|
|
Which sign of heart disease may be a part of pericardial disease, right-sided valve lesion, and cor pulmonale?
|
edema
|
|
|
which sign of heart disease may be due to venous insufficiency, venous obstructions, medications, and premenstrual hormonal changes?
|
edema
|
|
|
What is the fourfold diagnosis required for cardiac disease?
|
-etiology
-congenital/acquired -disturbance of rhythm and conduction/distrubance of contractility -functional classification (NYHA) |
|
|
Which NYHA classification of cardiac disease has no limitation of physical activity and no undue fatigue, dyspnea, or anginal pain with ordinary activity?
|
Class I
|
|
|
Which NYHA classification of cardiac disease has slight limitation of physical activity and has symptoms with ordinary activities?
|
Class II
|
|
|
Which NYHA classification of cardiac disease has marked limitation of physical activity; comfortable at rest; less than ordinary activity causes symptoms?
|
Class III
|
|
|
Which NYHA classification of cardiac disease has symptoms that may be present even at rest; unable to engage in any physical activity without discomfort?
|
Class IV
|
|
|
What causes acute or focal inflammation of the myocardium?
|
myocarditis
|
|
|
What heart condition EKG may show sinus tachycardia, other arrhythmias, conduction abnormalities, or ST-T changes?
|
myocarditis
|
|
|
What type of heart condition often follows a URI infection?
|
myocarditis
|
|
|
What are 7 causes of drug induced & toxic carditis?
|
doxorubicin
other cytotoxic agents cocaine phenothiazines lithium chloroquine radiation therapies |
|
|
What is the treatment for drug induced & toxic carditis?
|
supportive
|
|
|
What is the most common causes of myocarditis?
|
coxsackie virus (Rocky Mountain spotted fever)
chagas disease (S. America) |
|
|
What are the 3 main types of cardiomyopathies?
|
dilated cardiomyopathy (DCM)
hypertrophic cardiomyopathy (HCM) restrictive cardiomyopahty (RCM) |
|
|
Which type of cardiomyopathy is characterized by ventricular dilation oand decreased systolic contractile dysfunction?
|
dilated cardiomyopahty (stretched so far that no longer effective)
|
|
|
Which type of cardiomyopathy is characterized by thickened hypercontractile ventricles?
|
hypertrophic cardiomyopathy (ventricles so thick and not much room for blood)
|
|
|
Which type of cardiomyopathy is characterized by stiff myocardium, impaired ventricular relaxation, usually preseved contractile function?
|
restrictive cardiomyopathy (not pumping as effectively because stiff; something in the way)
|
|
|
What are 3 causes of restrictive cardiomyopathy?
|
scar tissue (fibrosis
tumor sarcoidosis |
|
|
What has rigid ventricales that impair diastolic filling but retain normal size and usually normal systolic function?
|
restrictive cariomyopathy
|
|
|
With RCM, what does the reduced compliance of the ventricles lead to?
|
elevated diastolic pressure (which leades to elevated systemic and pulmonic pressures which causes L and R vascular congestion; leads to reduced ventricular cavity size resulting in decreased stroke volume and cardiac output
|
|
|
Some signs and symptoms of RCM are fatigue, ___ exercise tolerance, dyspnea with ___, tachypnea, tachycardia, basilar ___ or ___, soft ___ and ___, low amplitude ___ pulsations, and JVD.
|
decreased
exertion rales or crackles S1 and S2 carotid |
|
|
What are 3 signs and symptoms of RCM that show heart failure?
|
peripheral edema
hepatomegaly ascites |
|
|
What is the condition that RCM's profile is shared with?
|
constrictive pericarditis (curable)
|
|
|
What 3 types of diagnostics can be used for RCM?
|
CT
MRI endomyocardial biopsy (ID infiltrate) |
|
|
RCM has a ___ prognosis, progress can sometimes be slowed by ____, other treatments are for ___ relief, and may need ___ for thrombus formation.
|
poor
steroids symptomatic anti-coagulant (coumadin) |
|
|
What is due to dilation of the ventricles with only minor hypertrophy?
|
dilated cardiomyopathy
|
|
|
What are the 3 most common causes of dilated cardiomyopathy?
|
viral (Coxsackie group B and echoviruses)
alcohol toxicity |
|
|
Which type of cardiomyopathy microscopically shows the myocytes degenerating with irregular hypertrophy and atrophy; there is extensive interstitial and perivascular fibrosis as well?
|
dilated cardiomyopathy
|
|
|
Which type of cardiomyopathy has two compensatory mechanisms that render the patient initially asymptomatic?
|
dilated cardiomyopathy
|
|
|
AS the cardiac output falls with dilated cardiomyopathy, the resulting decline in renal blood flow activates what system which causes increased peripheral vascular resistance and increased intravascular volume?
|
renin-angiotensin system (increase restriction of arteries peripherally)
|
|
|
As the ventricles enlarge with dilated cardiomyopathy, the AV valves fail and regurgiation ensues leading to atrial ___ which can lead to atrial ___, which leads to further ineffectiveness of the ___ ____ presenting to the systemic circulation.
|
dilation
fibrillation stroke volume |
|
|
With DCM what are 4 factors of fatigue?
|
lightheadedness
exertional dyspnea edema digital pallor |
|
|
Some of the signs and symptoms of DCM are ___ extremities, ___ BP, ___cardia, and pitting ___.
|
cool
low tachy edema |
|
|
What are the 2 lung sounds that may be heard with DCM?
|
late inspiratory crackles
basilar dullness |
|
|
With DCM, what are 5 signs of the heart?
|
enlarged heart
displaced diffuse PMI S3 regurg murmurs JVD |
|
|
Which cardiomyopathy CXR shows suggestive cardiac silhouette, alveolar edema, and/or plural effusion?
|
dilated cardiomyopathy
|
|
|
For DCM, the EKG shows A-V ___, dysrhythmias, R/L bundle branch ___ (interventricular septum), and diffuse ___ changes.
|
enlargement
block ST/T |
|
|
What type of diagnositic test for DCM shows chamber enlargement with little hypertrophy and reduced systolic contractile force?
|
two dimensional echocardiography
|
|
|
The treatment for DCM is to treat identified ___ causes, relieve pulmonic/systemic congestion with a ___, augmentation of ___ cardiac output with ___, prevent dysrhythmias, prevent thrombo-emboli with ___, and consider cardiac ___.
|
underlying
diuretic low Digoxin coumadin transplant |
|
|
The prognosis for DCM is ___ with a ___ year survival rate of less than ___%.
|
poor
5 50 |
|
|
Which type of cardiomyopathy is commonly found in young athletic men who die suddenly while vigorously exercising?
|
hypertrophic cardiomyopathy
|
|
|
What are the 2 forms of HCM?
|
sporadic and hereditary
|
|
|
Where is hypertrophy in HCM the most common?
|
septum (90%)
|
|
|
With HCM, the ___ valve function is impaired and it usually involves the ___ leaflet resulting in ___ regurgitation. The narrowed outflow tract will give rise to turbulent blood flow thus generating a ___ in the ___ area as well.
|
mitral
anterior mitral murmur aortic |
|
|
Some of the signs and symptoms of HCM are ___, ___, and ___; prominent ___ heart sound, a ___ apical impulse at the apex, prominent ___ pulsations that quickly rises and falls, rough ___-___ murmur at ___ sternal border, and a ___ regurgitation murmur may be heard at the apex.
|
dyspnea/angina/syncope
S4 double carotid crescendo-decrescendo left mitral |
|
|
What are 3 types of diagnostic studies for HCM?
|
EKG
echocardiography Doppler Flow |
|
|
An EKG for HCM shows ___ waves in inferior and lateral leads, atrial/ventricular dysrhythmias. ___ waves are usually seen after a heart attack.
|
Q
Q |
|
|
Treatment for HCM is ___ ____ to reduce the myocardial oxygen demand by ___ the HR and lessening the force of contraction, ___ ___ ___ to reduce ventricular stiffness and improve exercise capacity, anti-___ to reduce the symptomatic rhythm disturbances and prophylaxis for bacterial ____.
|
beta blockers
slowing calcium channel blockers arrhythmics endocarditis |
|
|
What is the most common congenital cardiac malformation?
|
bicuspid aortic valve
|
|
|
With bicuspic aortic valve, the heart functions normally at birth but often becomes gradually obstructed by ___ and ___ changes and may turn into ___ ___.
|
calcific
fibrous aortic stenosis |
|
|
What is the auscultatory hallmark for bicuspid aortic valve?
|
audible systolic ejection click heard best at the apex
|
|
|
Bicuspid aortic valve symptoms include angina, ___ dyspnea, ___, and syncope; may progress to ___ ___; diagnosis confirmed by ___ echo.
|
exertional
presyncope heart failure 2-D |
|
|
The treatment for bicuspid aortic valve is close ___ of patients; ___ patients with normal EKG and ___ test may have ___ athletic participation; ___ children without significant ___ insufficienty --> ___ aortic valvotomy; valve ___ in young adults.
|
supervision
asymptomatic exercise unlimited symptomatic aortic transcatheter replacement |
|
|
Where does coarctation of the aorta typically occur?
|
just distal to the left subclavian artery (increase blood flow to head & arms, so may have stronger pulses on upper body than lower)
|
|
|
The most common complications with coarctation of the aorta are systemic ___ and secondary ___ ventricular hypertrophy with heart failure; heart failure most common in ___ and after age ___; ___ exam is important for recognition.
|
hypertension
left infants 40 newborn |
|
|
For diagnosis of coarctation of the aorta: young adults may be ___; should always be considered in ___ and young ___ with unexplained ___ extremity ___; pressure differential may cause ___, headaches, leg ___, ___, angina; PE may show ___ body more developed than ___ body.
|
asymptomatic
adolescents men upper hypertrophy epistaxis fatigue claudication upper lower |
|
|
For diagnosis of coarctation of the aorta, systolic murmur is heard ___, EKG may show ___ ventricular hypertrophy, CXR with ___ sign and rib ___; upper pulses/BP are ___ than lesser pulses/BP; ___ is the best test to visualize the descending aorta.
|
posteriory
left 3 notching greater MRI |
|
|
___ is the treatment of choice for coarctation of the aorta and it is most effective in reducing ___ when performed at ___ age; after treatment, focal recoarctation may be treated with ___ ___ as needed; complications (rarely) include aortic ____ and aortic ___.
|
surgery
hypertension early balloon angioplasty aneurysms rupture |
|
|
What is the most common form of atrial septal defect?
|
persistence of the ostium secundum int the mid septum
|
|
|
With atrial septal defect, ___ blood from the ___ atrium passes into the ___ atrium, ___ RV output and pulmonary blood flow.
|
oxygenated
left right increased |
|
|
Most patients with atrial septal defect have ___ left-to-right shunts, but moderate to ___ shunts can lead to ___ hypertension.
|
small
large pulmonary |
|
|
With atrial septal defect, the ___ ___ does not close like it should and there is a mixture of oxygenated and deoxygenated blood on the ___.
|
foramen ovale
right |
|
|
Most patients with ASD are ___, but are predisposed to ___ fibrillation and ___ right-to-left emboli; ___ may be widely split; moderately loud systolic ___ murmur in the 2nd and 3rd intercostal spaces bilaterally.
|
asymptomatic
atrial paradoxical S2 ejection |
|
|
EKG of atrial septal defect may show ___ ventricular ___; incomplete or complete ___; CXR shows ___ pulmonary arteries, enlarged ___ atrium and ventricle, ___ aortic knob; echo shows large ___ with overload and may show actual defect.
|
right
hypertrophy RBBB large right small RV |
|
|
With ASD, pulmonary to systemic blood flow ratios > ___ are an indication for ___ to close defect; surgery withheld if pulmonary hypertension has caused ___ ___; want surgery before ___ years of age.
|
2.0
surgery reverse shunt 40 |
|
|
Is ASD or VSD worse?
|
VSD
|
|
|
Left-to-right shunting with VSD varies based on ___ of defect; large defects are associated with early ___ ___ failure.
|
size
left ventricular |
|
|
Many defects of ___ will close spontaneously in early childhood.
|
VSD
|
|
|
With VSD, large shunts have loud, harsh, holosystolic ___ in ___ 3rd and 4th intercostal spaces and systolic ___ is common.
|
murmur
left thrill |
|
|
What type of diagnostic technique may show ventricular septal defect?
|
echocardiography
|
|
|
What type of diagnostic technique can show the magnitude of shunting with VSD?
|
Doppler ultrasonography
|
|
|
With VSD, ___ prophylaxis is mandatory due to risk of ___.
|
antibiotic
endocarditis |
|
|
With VSD, large shunts may lead to ___ early in life; survival past ___ years is unusual; defects causing large shunts should be ___ repaired in late ___.
|
CHF
40 surgically childhood |
|
|
What is the most common cyanotic malformation?
|
tetralogy of Fallot
|
|
|
What is the tetrad for tetralogy of Fallot?
|
pulmonary stenosis
VSD aortic override right ventricular hypertrophy |
|
|
Does tetralogy of Fallot have increased left-to-right or right-to-left shunting?
|
right-to-left
|
|
|
Children with tetralogy of Fallot exhibit bluish skin during episodes of ___ or ___.
|
crying
feeding |
|
|
What is the most common EKG finding after repair of tetralogy of Fallot and what does CXR show?
|
RBBB
"boot-shaped" heart |
|
|
Which congenital heart disease CXR shows a "3 sign" and rib notching?
|
coarctation of the aorta
|
|
|
Which congenital heart disease CXR shows a "boot-shaped" heart?
|
tetralogy of Fallot
|
|
|
With situs inversus, the heart and stomach are on the ___, the liver is on the ___, atria and ventricles are ___.
|
right
left inverted |
|
|
Which congenital heart disease CXR shows right-sided apex of the heart and right-sided stomach bubble?
|
situs inversus
|
|
|
EKG for sinus inversus shows and inverted ___ and ___ wave in lead I with ___ QRS deflection.
|
P
T negative |
|
|
Which congenital heart disease shows the tricuspid valve displaced into the RV with possible ASD?
|
Ebstein's anomaly
|
|
|
With Ebstein's anomaly, the valve is ___, there is a wide spectrum of severity, auscultation reveals a clicking "___ ___", and EKG shows high peaked ___ waves with bizarre QRS complexes.
|
regurgitant
sail sound P |
|
|
Which congenital heart disease reveals a clicking "sail sound" with auscultation?
|
Ebstein's anomaly
|
|
|
Complications of Ebstein's anomaly are atrial ____ due to severe ___ atrial enlargement and ___ due to ___-to___ atrial shunt.
|
arrhythmias
right cyanosis right-to-left |
|
|
What connects the pulmonary artery and aorta in utero?
|
ductus arteriosus
|
|
|
Small PDA function normally, but are at risk for infectious ____; moderate to large PDA will have ___-to___ shunting.
|
endarteritis
left-to-right |
|
|
2/3 of patients with patent ductus arteriosus die by age ___.
|
60
|
|
|
EKG of PDA shows a bifid ___ wave in at least 1 limb lead and variable degree of ___ hypertrophy.
|
P
LV |
|
|
In older patients with PDA, CXR shows ___;___ aorta and pulmonary ___ are ___.
|
calcification
ascending artery dilated |
|
|
Surgery/closure for patent ductus arteriosus is contraindicated with ___-to___ shunt.
|
right-to-left
|
|
|
With anomalous venous return, pulmonary ___ connect to the ___ vena cava and there is usually ___.
|
veins
superior ASD |
|
|
CXR with anomalous venous return shows a shadow that resembles a Turkish ___ (sometimes called ___ syndrome); can be associated with hypoplasia of the ___ lung.
|
sword
scimitar right |
|
|
What are 9 types of congenital heart disease?
|
bicuspid aortic valve
coarctation of the aorta atrial septal defect ventricular septal defect tetralogy of Fallot situs inversus Ebstein's anomaly patent ductus arteriosus anomalous venous return |
|
|
What is the #1 killer in the US and worldwide?
|
coronary heart disease
|
|
|
What is the #1 preventable cause of cardiovascular disease?
|
smoking
|
|
|
Is hypo- or hyper- estrogenemia in women a more likely risk factor for coronary heart disease?
|
hypoestrogenemia
|
|
|
The risk of CHD decreased 50%, after how many years after quitting smoking?
|
1 year
|
|
|
What is an example of a drug that helps people cut back on smoking?
|
Chantix
|
|
|
Are LDL's or HDL's considered bad cholesterol?
|
LDL
|
|
|
What is an independent risk factor of lipid metabolism?
|
hypertriglyceridemia (may be hereditary)
|
|
|
For the LDL:HDL ratio, <___ is protective and >___ is higher risk. You want to have LDL <___ and HDL >___.
|
3
5 100 40 |
|
|
What is the best characterized inflammatory marker for CHD?
|
C-reactive protein (CRP)
|
|
|
What are 4 markers of imflammation which are a strong risk for CHD?
|
C-reactive protein
interleukin-6 CD-40 ligand placental growth factor |
|
|
What are 3 treatments of lipid abnormalities?
|
statins (stabilize plaque so they don't break off)
oral niacin antioxidant therapy? |
|
|
What are 2 methods of antiplatelet therapy?
|
ASA 325mg po qod
omega-3 fatty acids (fish oil) |
|
|
For prevention of CHD, what are the 4 types of high risk patients that ACE-I should be given for?
|
DM
atherosclerotic disease heart failure LV dysfunction |
|
|
Decreasing homocysteine levels is one type of prevention of CHF, which is done with folic acid with ___ and ___.
|
B6
B12 |
|
|
The initial step of atherosclerosis is "___ ___", which contains ___ and lipid-laden ___.
|
fatty streak
lipids (LDL) monocytes |
|
|
For atherosclerosis, after the "fatty streak", ___ cells are formed, then ___ muscle migrates, and a ___ ___ is formed, which turns into a ____. When platelets stick together they can form a ___.
|
foam
smooth fibrous cap plaque clot |
|
|
What are 3 things that increase plaque vulnerability?
|
higher lipid content
higher concentration of macrophages very thin fibrous cap |
|
|
What happens when foam cells die?
|
they release fat
|
|
|
If a clot is formed in the ___ artery then a stroke can occur (goes to the brain)?
|
carotid
|
|
|
What are 2 things that myocardial ischemia are provoked by?
|
increased demands for oxygen
decreased oxygen supply |
|
|
Is unstable or stable angina usually due to a thrombus or platelets plugging the lumen?
|
unstable angina
|
|
|
What type of pathophysiology of coronary heart disease is reversible and occurs in areas that are persistently underperfused-->develop sustained contractile dysfunction and can lead to LV failure?
|
myocardial hibernation
|
|
|
What is persistent contractile dysfunction following prolonged or repeated episodes of ischemia?
|
myocardial stunning
|
|
|
Angina pectors occurs most commonly during ___ and is relieved by ___; more common after ___, during ___, or with exposure to ___; more common in the morning with strong ___.
|
activity
rest meals excitement cold emotion |
|
|
What is the classic sign of angina pectoris?
|
clenched fist over the middle of the chest (Levine's sign)
|
|
|
Which dermatomes may angina pectoris radiate to and where does it usually radiate?
|
C8-T4
left shoulder |
|
|
Where is angina pectoris most often located?
|
substernally
|
|
|
Angina pectoris is not usually describes as "___", but as tightness, pressing, choking, aching, etc.; usually occurs between 3 and ___ mins and then goes away.
|
pain
20 |
|
|
What do angina pectoris attacks lasting more than 30 minutes suggest?
|
unstable angina or MI
|
|
|
What type of medication is beneficial in relieving angina pectoris attacks and also in preventing attacks?
|
NTG (vasodilates)
|
|
|
What are 5 possible signs of angina pectoris?
|
elevated BP
hypotension gallop rhythm xanthelasma tendinous xanthomas |
|
|
What is the most useful noninvasive test for angina pectoris?
|
exercise stress test
|
|
|
What are 3 things to evaluate if suspicious of angina pectoris?
|
lipid levels
EKG exercise stress test |
|
|
What marks a positive stress test for angina pectoris?
|
1mm ST depression (false positives are uncommon if there is a 2mm ST depression
|
|
|
What are 6 indications for myocardial scintigraphy?
|
resting EKG hard to interpret
stress test confirmation localize ischemia assess bypass surgery results prognostic indicator distinguish b/t ischemic and infarcted myocardium |
|
|
Myocardial scintigraphy uses ___ or ____ and looks for areas not taking up as much ___ or ___.
|
thallium; technetium
thallium; technetium |
|
|
What is the definitive diagnostic procedure for CAD?
|
coronary angiography
|
|
|
The type of treatment that can be used for angina pectoris sublingual ___, which work in ___ minutes and can be repeated every ___ minutes. However, if there is no response after ___ doses or ___ minutes, call 911.
|
NTG
1-2 5 3 20 |
|
|
What is the only anti-anginal agents that has been shown to prolong life?
|
Beta blockers
|
|
|
What are 4 types of prevention medications for angina pectoris?
|
nitrate theraphy
beta blockers calcium channel blockers platelet inhibitors |
|
|
What are 2 types of platelet inhibitors?
|
aspirin
clopidogrel (Plavix) |
|
|
What is CABG?
|
coronary artery bypass grafting
|
|
|
What other vein is used with CABG?
|
saphenous vein
|
|
|
What are 2 types of revascularization techniques?
|
CABG
percutaneous transluminal coronary angioplasty (PTCA) & stenting |
|
|
What is defined as accelerating patterns of angina with less exertion or at rest?
|
unstable angina
|
|
|
What plays an important role in unstable angina?
|
thrombosis
|
|
|
What agents should be used for thrombolytic and antiplatelet therapy for unstable angina?
|
*2 or more*
ASA IV heparin Clopidogrel (Plavix) |
|
|
What are 5 indications for revascularization?
|
-symptoms despite medical therapy
-left main coronary artery stenosis > 50% -3 vessel disease w/ LV dysfunction -unstable angina -post MI patients w/ angina |
|
|
What results from a prolonged myocardial ischemia and in most cases is precipitated by a thrombus at the site of a plaque?
|
myocardial infarction
|
|
|
For acute MI, what should be considered in young patients without risk factors?
|
cocaine (vasoconstriction)
|
|
|
What are 3 common locations of acute MI?
|
anterior descending branch of LCA
left circumflex right coronary artery |
|
|
A transmural infarction usually has development of ___ waves.
|
Q
|
|
|
A subendocardial infarction usually has no ___ waves.
|
Q
|
|
|
Sudden death and early arrhythmias occur in 20% of patients with acute MI and they will usually die before reaching the hospital due to ___.
|
v-fib
|
|
|
For acute MI, the lungs may have basilar ___; heart has abnormal ___, usually S4 ___; ___ of extremities indicates low output.
|
rales
PMI gallop cyanosis |
|
|
What are the 2 labs that can be done for acute MI?
|
CK-MB (elevated 4-6 hours)
Troponin-I,T (elevated 5-7 days) |
|
|
Which lab for acute MI is more specific for coronary necrosis?
|
troponins
|
|
|
What is the classic evolution of changes found on an EKG for acute MI?
|
peaked T waves
ST segment elevation Q wave development T wave inversion |
|
|
What is a convenient bedside assessment of LV global and regional function?
|
echocardiography (normal wall motion makes infarction unlikely)
|
|
|
Scintigraphic studies can be used to diagnose acute MI after ___ hours, provides a "___ ___" image, but is insensitive to ___ infarctions.
|
18
hot spot small |
|
|
What are 4 things that can be used as thrombolytic therapy with acute MI?
|
streptokinase
anistreplase alteplase (t-PA) reteplase and tenecteplase (longer half life) |
|
|
Generally, patients with non-ST segment elevation MI do not have persistent ___ coronary occlusions.
|
thrombotic
|
|
|
For acute MI, if NTG is not effective then IV ___ can be used as analgesia.
|
opioids (morphine)
|
|
|
What type of medication for acute MI has been shown to improve survival rate, but should be avoided in unstable heart failure or asthma?
|
beta blockers
|
|
|
What type of medication for acute MI has both short and long term improvement and is most effective in patients with low EF or heart failure?
|
ACE-I
|
|
|
What can be used as a antiarrhythmic prophylaxis for acute MI and is only recommended for patients with nonsustained ventricular tachycardia?
|
lidocaine
|
|
|
What type of complication of MI is most common in inferior infarctions?
|
sinus bradycardia
|
|
|
With complications of MI, block at the ___ node is more common in post MI.
|
AV
|
|
|
What type of block is the most common and does not require treatment?
|
first degree block
|
|
|
What should v-tach be treated with if patient is stable or by electrical cardioversion?
|
lidocaine
|
|
|
With second degree block, it is usually ___ type ___, often transient and usually does not require treatment.
|
Mobitz
I |
|
|
Complete AV block (3rd degree block) will often resolve ___, can be treated with IV ___, and temporary ___ may be required.
|
spontaneously
atropine pacing |
|
|
In anterior infarction (Mobitz type ___ or ___ heart block): requires urgent ___ pacing, mortality is ___ and a permanent ___ should be considered.
|
II
complete ventricular high pacemaker |
|
|
What is the most appropriate pressor for cardiogenic hypotension?
|
dopamine
|
|
|
What is blood clots inside the chambers of the heart called?
|
mural thrombus (usually seen in anterior infarctions)
|
|
|
What are 12 complications of MI?
|
postinfarction ischemia
sinus bradycardia supraventricular tachyarrhythmias ventricular arrhythmias conduction distrubances acute LV failure hypotension and shock mechanical defects myocardial rupture LV aneurysm pericarditis mural thrombus |
|
|
What are 7 types of valvular heart disease?
|
aortic stenosis
mitral stenosis mitral regurgitation mitral valve prolapse aortic regurgitation tricuspid regurgitation pulmonic stenosis |
|
|
What is the most common surgical valve lesion in developed countries?
|
aortic stenosis
|
|
|
Aortic stenosis is usually asymptomatic until ___ or ___ age, there are delayed and diminished ___ pulses, soft/absent/paradoxically split ___, harsh ___ murmur, and often thrill which radiates to neck.
|
middle
old carotid S2 systolic |
|
|
What are 2 conditions that aortic stenosis is more common in?
|
smokers
hypertensives |
|
|
For aortic stenosis, EKG usually shows LV ___ and x-ray may show ___ valve.
|
hypertrophy
calcified |
|
|
What are 2 common clinical scenarios of aortic stenosis?
|
congenital bicuspid valve
degenerative aortic stenosis |
|
|
What diagnostic study is helpful to assess valve opening and LV wall thickness for aortic stenosis?
|
echo
|
|
|
What type of diagnositc study for aortic stenosis is used to evaluate blood flow?
|
Doppler (reduced, rapid blood flow)
|
|
|
What diagnostic technique provides definitive diagnosis for aortic stenosis?
|
cardiac catherization
|
|
|
After onset of ___ ___, ___, or ___ prognosis of aortic stenosis is poor (once notice symptoms).
|
heart failure
angina syncope |
|
|
Which type of valvular heart disease has a stiff valve that doesn't open well, turbulent flow, and is usually asymptomatic until middle or old age?
|
aortic stenosis
|
|
|
What are things that often precipitate symptoms of mitral stenosis?
|
pregnancy
a-fib |
|
|
What do nearly all patients with mitral stenosis have underlying?
|
rheumatic heart disease (Strep.)
|
|
|
What is the characteristic finding of mitral stenosis?
|
localized mid-diastolic murmur
|
|
|
What is the most valuable diagnostic test to assess mitral stenosis?
|
echo
|
|
|
Which vavular heart disease has left atrium hypertrophy and a thickened valve that opens poorly and closes slowly; if backed up then will also be backed up in lungs?
|
mitral stenosis
|
|
|
What are 3 essentials of diagnosis for mitral stenosis?
|
dyspnea
orthopnea PND |
|
|
Mitral stenosis has a prominent mitral ___, ___ snap, apical ___ ___ murmur, EKG often shows ___, and ___ confirms diagnosis.
|
S1
opening diastolic crescendo a-fib echo |
|
|
Which valvular heart disease has an enlarged left atrium that predisposes to a-fib and systemic emboli?
|
mitral stenosis
|
|
|
With mitral stenosis, a-fib should be converted and maintained in ___ rhythm; best results when converted before ___ months and if the ___ is not enlarged; once a-fib has occurred, must be anticoagulated with ___.
|
sinus
12 atrium warfarin (coumadin |
|
|
What is the preferred procedure for mitral stenosis?
|
percutaneous balloon valvuloplasty
|
|
|
When is valve replacement for mitral stenosis indicated?
|
when there is stenosis and insufficiency or valve is too distorted
|
|
|
With mitral stenosis, what is required for a prosthetic valve?
|
warfarin
|
|
|
What occurs when the mitral valve does not close completely?
|
mitral regurgitation
|
|
|
With mitral regurgitation there is a pansystolic murmur at __ of heart radiating into ___ that is associated with ___ heart sound, and a hyperdynamic ___; may predispose to infective ___.
|
apex
axilla S3 PMI endocarditis |
|
|
What is myxomatous mitral valve?
|
floppy mitral valve
OR mitral valve prolapse |
|
|
Are most patients with aortic stenosis male or female?
|
male (4:1)
|
|
|
Are most patients with mitral valve prolapse male or female?
|
female (many are thin)
|
|
|
With mitral valve prolapse, midsystolic ___ are heard best when the patient is standing; valve ___ is preferred to valve ___; patients with murmurs are prone to ___ and require ___ prophylaxis.
|
clicks
repair replacement endocarditis antibiotic |
|
|
What may secondary mitral regurgitation come from?
|
dilated cardiomyopathy
|
|
|
With mitral regurgitation,___ shows underlying pathology and ___ shows severtiy.
|
echo
Doppler |
|
|
What are 3 types of conditions that may cause acute mitral regurgitation often require emergency surgery?
|
endocarditis
MI ruptured chordae tendinae |
|
|
Which vavular heart disease has blood going into the left ventricle from 2 different sources?
|
aortic regurgitation
|
|
|
Aortic regurgitation is usually asymptomatic until ___ age, presents with ___ heart failure or chest pain, wide pulse pressure, hyperactive enlarged ___ ventricle, and diastolic murmur along ___ sternal border.
|
middle
left left left |
|
|
For aortic regurgitation, ___ shows LV hypertrophy and ___ confirms diagnosis.
|
EKG
echo |
|
|
___ aortic regurgitation has become less common due to use of ___.
|
rheumatic
antibiotics |
|
|
What are 3 major causes of aortic regurgitation (non-rheumatic)?
|
congenitally bicuspid valve
infective endocarditis hypertension |
|
|
With chronic regurgitation what may be the only sign?
|
soft aortic diastolic murmur
|
|
|
What progressively enlarges with aortic regurgitation?
|
left ventricle
|
|
|
What are 5 common symptoms of aortic regurgitation?
|
fatigue
exertional dyspnea pulmonary edema PND chest pain |
|
|
What are 4 characteristic findings of aortic regurgitation?
|
Corrigan's pulse
Quincke's pulses Duroziez's sign Musset's sign |
|
|
What is also known as waterhammer's pulse; rises and falls really fast?
|
Corrigan's pulse
|
|
|
What creates a head bob with each pulse?
|
Musset's sign
|
|
|
If you partially compress a peripheral artery (ex. femoral), which sign can you hear blood going to and fro?
|
Duroziez's sign
|
|
|
What is called when you can see pulsations in the bed of the fingernails?
|
Quincke's pulses
|
|
|
With aortic regurgitation threre is s ___ pulse that is ___ displaced; aortic diastolic murmur that is high-pitched and ___.
|
apical
laterally decrescendo |
|
|
With aortic regurgitation, ___ can reduce severity and postpone need for surgery; prognosis is ___ without surgery once symptoms occur.
|
vasodilators (hydralazine, nifedipine, ACE-I)
poor |
|
|
Treatment for aortic regurgitation needs to be followed by serial ___ when asymptomatic; ___ size usually decreases after surgery.
|
echos
LV |
|
|
Which type of valvular heart disease backs up into the right atrium and may back up into the body (ascites, peripheral edema)?
|
tricuspid regurgitation
|
|
|
What are 2 types of patients that tricuspid regurgitation is commonly seen in?
|
pulmonary or cardiac disease
|
|
|
What is the catch 22 for tricuspid regurgitation?
|
often due to RV dilation, and regurgitation worsens RV dilation, which worsens regurgitation
|
|
|
What are 4 causes of tricuspid regurgitation?
|
pulmonary hypertension
severe pulmonic regurgitation cardiomyopathy left heart failure |
|
|
Tricuspid regurgitation has a systolic ___ wave in jugular venous pulsations, holosystolic murmur along ___ sternal border that increases with ___, possible ___ heart sound, and possible cyanosis.
|
c-v
left inspiration S3 |
|
|
What is the definitive treatment for tricuspid regurgitation?
|
elimination of the cause
|
|
|
Is anticoagulation required for tricuspid regurgitation?
|
not required unless there is associated a-fib
|
|
|
For tricuspid regurgitation diagnostic studies, ___ is usually nonspecific, chest x-ray shows dilated ___, and ___ helps assess RV size and function.
|
EKG
RA echo |
|
|
What is a congenital disease resulting from fusion of the pulmonic valve cusps?
|
pulmonary stenosis
|
|
|
Where is the pulmonic valve located?
|
2nd intercostal space on left of sternum
|
|
|
Pulmonary stenosis is usually detected and corrected in ___, symptoms include ___ and ___, and signs are early systolic ejection ___ followed by systolic ejection ___.
|
childhood
angina syncope click murmur |
|
|
___ confirms the diagnosis for pulmonary stenosis. Once symptoms develop, balloon ___ is effective in relieving symptoms.
|
echo
commissurotomy |
|
|
What are 6 things that can increase the prevalence of arrhythmias?
|
electrolyte abnormalities
hormonal imbalances hypoxia drug effects myocardial ischemia stress |
|
|
What are 2 disorders of automaticity arrhythmias?
|
sinus node arrest
premature beats |
|
|
What are 5 abnormalities of conduction arrhythmias?
|
sinus node
AV node inter-ventricular system sinoatrial exit block AV block |
|
|
What are 4 ways that arrhythmias can be classified?
|
disorder/abnormality of:
automaticity conduction reentry triggered activity |
|
|
What are 5 techniques for evaluation of arrhythmias?
|
EKG
Holter Event monitor electrophysiologic testing tilt table testing |
|
|
What are the 4 classes of antiarrhythmic drugs?
|
Class I: Na+ channel blockers
Class II: beta blockers Class III: block K+ channels Class IV: Ca2+ channel blockers |
|
|
Which class of antiarrhythmic drugs does quinidine, procainamide, disopyramide, and moricizine fall into?
|
Class Ia (sodium channel blockers)
|
|
|
Which class of antiarrhythmic drugs does lidocaine, phenytoin, and mexeletine fall into?
|
Class Ib (sodium channel blockers)
|
|
|
Which class of antiarrhythmic drugs does flacainide and propafenone fall into?
|
Class Ic (sodium channel blockers)
|
|
|
Which class of antiarrhythmic drugs does should be used for life-threatening VT or VF?
|
Class Ic (sodium channel blockers)
|
|
|
Which class of antiarrhythmic drugs decreases automaticity, prolongs AV conduction, prolongs and refractoriness?
|
Class II (beta blockers)
|
|
|
Which class of antiarrhythmic drugs does esmolol and propanolol fall into?
|
Class II (beta blockers)
|
|
|
Which class of antiarrhythmic drugs does amiodarone, sotalol, dofetilide, ibutilide, and bretylium fall into?
|
Class III (block potassium channels)
|
|
|
Which class of antiarrhythmic drugs prolong repolarization, widen the QRS, and prolong the QT interval?
|
Class III (block potassium channels)
|
|
|
Which class of antiarrhythmic drugs decrease automaticity and decrease AV conduction?
|
Class IV (calcium channel blockers)
|
|
|
What are 6 things that can increase the prevalence of arrhythmias?
|
electrolyte abnormalities
hormonal imbalances hypoxia drug effects myocardial ischemia stress |
|
|
What are 2 disorders of automaticity arrhythmias?
|
sinus node arrest
premature beats |
|
|
What are 5 abnormalities of conduction arrhythmias?
|
sinus node
AV node inter-ventricular system sinoatrial exit block AV block |
|
|
What are 4 ways that arrhythmias can be classified?
|
disorder/abnormality of:
automaticity conduction reentry triggered activity |
|
|
What are 5 techniques for evaluation of arrhythmias?
|
EKG
Holter Event monitor electrophysiologic testing tilt table testing |
|
|
What are the 4 classes of antiarrhythmic drugs?
|
Class I: Na+ channel blockers
Class II: beta blockers Class III: block K+ channels Class IV: Ca2+ channel blockers |
|
|
Which class of antiarrhythmic drugs does quinidine, procainamide, disopyramide, and moricizine fall into?
|
Class Ia (sodium channel blockers)
|
|
|
Which class of antiarrhythmic drugs does lidocaine, phenytoin, and mexeletine fall into?
|
Class Ib (sodium channel blockers)
|
|
|
Which class of antiarrhythmic drugs does flacainide and propafenone fall into?
|
Class Ic (sodium channel blockers)
|
|
|
Which class of antiarrhythmic drugs does should be used for life-threatening VT or VF?
|
Class Ic (sodium channel blockers)
|
|
|
Which class of antiarrhythmic drugs decreases automaticity, prolongs AV conduction, prolongs and refractoriness?
|
Class II (beta blockers)
|
|
|
Which class of antiarrhythmic drugs does esmolol and propanolol fall into?
|
Class II (beta blockers)
|
|
|
Which class of antiarrhythmic drugs does amiodarone, sotalol, dofetilide, ibutilide, and bretylium fall into?
|
Class III (block potassium channels)
|
|
|
Which class of antiarrhythmic drugs prolong repolarization, widen the QRS, and prolong the QT interval?
|
Class III (block potassium channels)
|
|
|
Which class of antiarrhythmic drugs decrease automaticity and decrease AV conduction?
|
Class IV (calcium channel blockers)
|
|
|
Which class of antiarrhythmic drugs does verapamil, diltiazem, adenosine, and digoxin fall into?
|
Class IV (calcium channel blockers)
|
|
|
What can all classes of antiarrhythmic drugs do?
|
exacerbater arrhythmias
|
|
|
What is often the primary treatment of arrhythmias?
|
radiofrequency ablation
|
|
|
What are 5 types of supraventricular arrhythmias?
|
sinus arrhythmia
sinus bradycardia sinus tachycardia atrial premature beats paroxysmal SVT (PSVT) |
|
|
Which type of arrhythmia has a cyclic increase in normal heart rate with inspiration and decrease with expiration and is seen most often in young children and the elderly?
|
sinus arrhythmia
|
|
|
Which type of arrhythmia has a heart rate slower than 50bpm and can cause weakness, confusion, or syncope; pacing may be required?
|
sinus bradycardia
|
|
|
Which type of arrhythmia has a heart rate faster than 100bpm and may lead to LV dysfunction?
|
sinus tachycardia
|
|
|
Which type of arrhythmia is caused by firing of an ectopic focus on the atria?
|
atrial premature beats
|
|
|
Which type of arrhythmia has P wave that is usually different in contour, may occur frequently in normal hearts, and may cause bizarre QRS or may not conduct to the ventricles?
|
atrail premature beats
|
|
|
What does a 1:1 relationship between P waves and QRS complexes in bradycardia usually mean?
|
supraventricular origin
|
|
|
What is the most common paroxysmal tachycardia and often occurs in patients without structural heart disease?
|
paroxysmal supraventricular tachycardia
|
|
|
What may be the heart rate for paroxysmal SVT?
|
140-240
|
|
|
What is the most common mechanism of paroxysmal SVT?
|
reentry
|
|
|
How are most PSVT resolved?
|
spontaneously
|
|
|
What is the therapy plan for PSVT?
|
ablation in the reentry circuit
|
|
|
What are 3 types of treatment for acute attacks of PSVT?
|
mechanical measures
drug therapy cardioversion |
|
|
What are 2 types of mechanical measures to treat an acute attack of PSVT?
|
valsalva maneuver
carotid sinus massage |
|
|
What type of drug therapy can be done for a PSVT acute attack?
|
IV adenosine (chest discomfort, flushing)
oral verapamil (if patient stable) |
|
|
When should cardioversion be used for PSVT acute attacks?
|
if patient is hemodynamically unstable or if adenosine and verapamil are contraindicated/ineffective
|
|
|
What is the preffered approach for recurrent PSVT to prevent further attacks?
|
radiofrequency ablation
|
|
|
What type of drugs can be used to prevent PSVT attacks?
|
digoxin (drug of choice?)
verapamil alone verapamil with dioxin beta blockers |
|
|
What is the most common chronic arrhythmia?
|
atrial fibrillation
|
|
|
Atrial fibrillation incidence and prevalence increases with age to nearly 10% in people over ___ years old.
|
80
|
|
|
What is "holiday heart" in atrial fibrillation due to?
|
alcohol excess
|
|
|
What is the EKG pattern of atrial fibrillation known as?
|
irregularly irregular
|
|
|
What is the only common arrhythmia in which the ventricular rate is rapid and the rhythm very irregular?
|
atrial fibrillation
|
|
|
What is the difference between the apical rate and the pulse rate in atrial fibrillation known as?
|
"pulse deficit"
|
|
|
What are 3 things that atrial fibrillation can lead to?
|
hypotension
myocardial ischemia myocardial dysfunction |
|
|
What is the atrial rate and ventricular response in atrial fibrillation?
|
atrial rate is 400-600 with irregular ventricular response 80-180
|
|
|
What is the most serious complication of atrial fibrillation?
|
thrombus formation --> embolization --> cerebrovascular accident (CVA)
|
|
|
What should patients with 1 or more risk factors for CVA and a-fib be treated with?
|
warafarin/coumadin
ASA (low risk patients) |
|
|
What is the initial management for atrial fibrillation in unstable patients?
|
hospitalization and immediate treatment
|
|
|
What is the initial management for patients with shock, severe hypotension, pulmonary edema, or an ongoing MI?
|
cardioversion
|
|
|
What is the initial management for atrial fibrillation in stable patients or patients with high risk for embolism?
|
rate control with beta blockers or calcium channel blockers
|
|
|
Heart failure patients should receive ___ or a beta blocker for subsequent management of atrial fibrillation.
|
digoxin
|
|
|
Subsequent management of atrial fibrillation includes anticoagulation with ___ until INR is ___.
|
warafarin
2.0-3.0 |
|
|
If cardioversion is planned for atrial fibrillation patients, then it should be done after 3 weeks of therapeutic ___.
|
INR
|
|
|
Atrial flutter is less common than fibrillation and occurs most often in patients with ___.
|
COPD
|
|
|
What type of heart condition has a varying P wave morphology and intervals with a rate between 100-140 and is associated with severe COPD?
|
multifocal atrial tachycardia
|
|
|
What type of condition uses the AV node or bundles of His as the pacemaker and has rate between 40 and 60?
|
AV junctional rhythm
|
|
|
What is AV junctional rhythm most commonly associated with?
|
myocarditis
CAD digitalis toxicity may be normal |
|
|
What are the characteristics of ventricular extrasystoles?
|
wide QRS complexes
P wave absent Bi-/Trigeminy +/- palpitations |
|
|
What are the first line agents for ventricular extrasystoles?
|
beta blockers
|
|
|
What is ventricular extrasystoles also known as?
|
ventricular premature beats (PVC)
|
|
|
What are 4 types of ventricular arrhythmias?
|
ventricular extrasystoles
ventricular tachycardia ventricular fibrillation & sudden death long QT syndrome |
|
|
What is defined as 3 or more consecutive ventricular premature beats with a rate between 160-240?
|
ventricular tachycardia
|
|
|
What is a frequent complication of acute MI or dilated cardiomyopathy?
|
ventricular tachycardia
|
|
|
What is a form of ventricular tachycardia in which QRS morphology twists around the baseline and may occur spontaneously int he setting of hypokalemia/hypomagnesmia (or drugs that prolong the QT interval)?
|
torsades de pointes (poor prognosis)
|
|
|
What is common with sustained v-tach?
|
sudden death
|
|
|
What type of drug reduces the risk of sudden death in patients with CHD or heart failure?
|
beta blockers
|
|
|
What is the treatment of acute v-tach?
|
cardioversion
IV lidocaine IV procainamide amiodarone ventricular overdrive pacing? |
|
|
How should sustained v-tach be managed?
|
with ICDs (internal cardiac defibrillation)
stable management with amiodarone +/- beta blocker |
|
|
What is defined as 3 or more ventricular beats lasting less than 30 seconds?
|
nonsustained v-tach (comes and goes)
|
|
|
What is the most common cause of sudden cardiac death?
|
ventricular fibrillation
|
|
|
What is the treatment of choice for appropriate patients with ventricular fibrillation?
|
implantable defibrillator
|
|
|
What is an uncommon disease that is characterized by recurrent syncope, a long QT interval, documented ventricular arrhythmias, and sudden death?
|
long QT syndrome (congenital)
|
|
|
What diagnosis is applied to patients with sinus arrest, sinoatrial exit block, or persistent sinus bradycardia?
|
sick sinus syndrome
|
|
|
What type of pacing is preferred for sick sinus syndrome?
|
dual chamber pacing (symptomatic relief following pacing has not been consistent)
|
|
|
Which type of AV block is characterized with PR interval > .21 second with all atrial impulses conducted?
|
first degree
|
|
|
Which type of AV block is characterized by intermittent blocked beats and is subclassified?
|
second degree
|
|
|
Which type of AV block is complete heart block in which no supraventricular impulses are conducted to the ventricles?
|
third degree
|
|
|
Which subclassification of AV block is characterized as the PR interval progressively lengthing, with the RR interval shortening before the blocked beat?
|
Mobitz type I (Wenckebach)
|
|
|
Which subclassification of AV block is characterized as intermittently nonconducted atrial beats not preceded by lengthening AV conduction?
|
Mobitz type II
|
|
|
Which type of AV block is often due to a lesion distal to the bundle of His?
|
complete heart block
|
|
|
Which type of AV block is almost always due to organic disease?
|
Mobitz type II (second degree)
|
|
|
What are 3 indications for permanent pacing?
|
symptomatic bradyarrhythmias
asymptomatic Mobitz type II complete heart block |
|
|
For standardized nomenclature of permanent pacing, which letter refers to the chamber which is stimulated?
|
first letter
|
|
|
For standardized nomenclature of permanent pacing, which letter refers to the chamber where sensing occurs?
|
second letter
|
|
|
For standardized nomenclature of permanent pacing, which letter refers to the sensory mode?
|
third letter
|
|
|
For standardized nomenclature of permanent pacing, which letter refers to programmability?
|
fourth letter
|
|
|
What is the most physiologic approach for permanent pacing?
|
a pacemaker that senses and paces in both chambers
|
|
|
What is dual chamber pacing most useful for?
|
LV dysfunction and physically active patients
|
|
|
What is transient loss of consciousness with prompt recovery?
|
syncope
|
|
|
What may be due to excessive vagal tone or impaired reflex control of the peripheral circulation and what group of people is it the most common for?
|
vasomotor syncope
young women |
|
|
What is orthostatic hypotension?
|
decline in BP more than 20mmHg upon standing, usually with increased HR
|
|
|
What is mandatory for cardiogenic syncope?
|
ambulatory ECG monitoring
|
|
|
How many Americans have HTN and is greater in blacks or whites?
|
66 million
blacks |
|
|
What is classified as normal BP?
|
S: <120
D: <80 |
|
|
What is classified as prehypertension?
|
S: 120-139
D: 80-89 |
|
|
What is classified as stage I hypertension?
|
S: 140-159
D: 90-99 |
|
|
What is classified as stage II hypertension?
|
S: >160
D: >100 |
|
|
Which type of hypertension is applied to the 95% of cases in which no cause for hypertension can be identified?
|
primary/essential hypertension
|
|
|
What are 5 environmental factors of primary/essential hypertension?
|
sympathetic nervous systen hyperactivity, renin-angiotensin system, defect in natriuresis, intracellular sodium and calcium, exacerbating factors
|
|
|
What are 7 exacerbating factors that can cause essentail hypertension?
|
obesity
salt intake EtOH smoking polycythemia NSAID use low K+ |
|
|
What type of hypertension is seen in approximately 5% of patients with hypertension with a specific cause?
|
secondary hypertension
|
|
|
What are 9 causes of secondary hypertension?
|
estrogen use, renal disease, primary hyperaldosteronism, Cushing's syndrome, pheochromocytoma, coarctation of the aorta, pregnancy
|
|
|
Of the 5% of women that have secondary hypertension from estrogen use, what group of women is it more common in?
|
>35 years old
|
|
|
With renal disease causing secondary hypertension, what is the most often cause?
|
fibromuscular hyperplasia (especially in women <50 years)
|
|
|
Where is the lesion generally located for primary hyperaldosteronism and Cushing's syndrome?
|
adrenal (adenoma)
|
|
|
What is one of the most common causes of maternal and fetal morbidity and mortality?
|
secondary hypertension
|
|
|
What are 5 complications of untreated HTN?
|
hypertensive cardiovascular disease, cerebrovascular disease and dementia, renal disease, aortic dissection, atherosclerosis
|
|
|
What is a major predisposing cause of stroke?
|
hypertension
|
|
|
What are 2 things that chronic HTN can lead to involving renal disease?
|
nephosclerosis and renal insufficiency
|
|
|
What is the most frequent symptom for HTN?
|
headaches (typically suboccipital early in the moring and subsiding during the day)
*usually asymptomatic for many years |
|
|
What may a fundoscopic exam for HTN show?
|
narrowing of the retinal arterial diameter to less than half the venous diameter, copper or silver wiring, hemorrhages or papilledema, AV nicking
|
|
|
What signs may be seen with the heart and arteries for HTN?
|
LV enlargement with a LV heave; possibly S4 gallop
|
|
|
What can be done to rule out coarctation when assessing signs for HTN?
|
compare upper and lower pulses
|
|
|
What are 7 recommended lab tests to do for HTN?
|
hemoglobin, urinalysis, renal function tests, electrolytes, fasting blood sugar levels, serum lipid levels, serum uric acid
|
|
|
What are 7 ways that may improve HTN nonpharmacologically?
|
DASH diet, weight reduction, moderation of EtOH, reduce salt intake, gradually increase activity levels, stop smoking, Ca2+ and K+ supplements
|
|
|
What are 7 types of drugs that can be taken for HTN?
|
diuretics
beta blockers ACE inhibitors angiotensin receptor blockers calcium channel blockers alpha blockers arteriolar dilators |
|
|
What type of HTN drug decreases plasma volume and reduces peripheral vascular resistance?
|
diuretics
|
|
|
What is the most widely used diuretic for HTN?
|
thiazides (HCTZ)
-relatively more effective in smokers |
|
|
What type of HTN drug is effective as single agent in 50% of patients with mild to moderate HTN?
|
diuretics
|
|
|
What type of HTN drug decreases heart rate, cardiac output, and renin release?
|
beta blockers
-especially effective in younger white patients |
|
|
What type of HTN drug neutralizes reflex tachycardia and is good for patients with a migraine and anxiety?
|
beta blockers
|
|
|
What are some possible side effects for using beta blockers for HTN?
|
bronchospasm, AV conduction depression, worsening left heart failure, nasal congestion,
Raynaud's phenomenon, fatigue, lethargy, impotence |
|
|
Using beta blockers for HTN may increase plasma ____ and decrease ___.
|
triglycerides
HDL's |
|
|
When should beta blockers be used with caution?
|
in type I diabetics, peripheral vascular disease
|
|
|
What are 2 types of beta blockers used for HTN?
|
Atenolol (Tenormin)
Carvedilol (Coreg) |
|
|
Which type of HTN drug inhibits the renin-angiotensin-aldosterone system, bradykinin degeneration, and stimulates prostaglandins?
|
ACE inhibitors
-more effective in younger whites |
|
|
Which type of HTN is very potent in combination with diurectics and calcium channel blockers?
|
ACE inhibitors
|
|
|
What is the drug of choice for HTN in diabetics and patients with heart failure?
|
ACE inhibitors
|
|
|
What are some possible side effects of ACE inhibitors?
|
hypotension, cough, hyperkalemia, skin rashes, taste alterations with captopril, angioedema
|
|
|
What are 2 types of ACE inhibitors used for HTN?
|
Captopril (Capoten)
Lisinopril (Zestril or Prinivil) |
|
|
What type of HTN drug is reserved primarily for pateints unable to tolerate an ACE-I?
|
angiotension receptor blockers (ARBs)
-higher cost |
|
|
What are 2 types of ARBs used for HTN?
|
Candesartan (Atacand)
Losartan (Cozaar) |
|
|
Which type of HTN drug acts by causing peripheral vasodilation?
|
calcium channel blockers
|
|
|
Which type of HTN drug may be preferable to beta blockers and ACE-I in blacks and older patients?
|
calcium channel blockers
|
|
|
What may diabetic patients on calcium channel blockers have higher rates of?
|
heart failure and MI
|
|
|
What are the most common possible side effects of calcium channel blockers?
|
headache, peripheral edema, bradycardia, constipation
|
|
|
What is the only agent that is proven safe in heart failure?
|
amlodipine
|
|
|
What are 2 types of calcium channel blockers used for HTN?
|
Amlodipine (Norvasc)
Nifedipine (Procardia XL) |
|
|
What type of HTN drug relaxes smooth muscle and lower peripheral vascular resistance?
|
alpha blockers
|
|
|
What are the common possible side effects of alpha blockers for HTN?
|
marked hypotension and syncope
*side effects are relatively common |
|
|
What are 2 types of alpha blockers used for HTN?
|
Prazosin (Minipress)
Terazosin (Hytrin) |
|
|
Which type of HTN drug relaxes vascular smooth muscle?
|
arteriolar dilators
|
|
|
What may happen if arteriolar dilators are given alone for HTN?
|
stimulate reflex tachycardia and cause headache, palpitations, and fluid retention
|
|
|
What are arteriolar dilators usually given with for HTN?
|
beta blockers or diuretics in resistant HTN
|
|
|
What are 2 types of arteriolar dilators for HTN?
|
Hydralazine
Minoxidil |
|
|
What is a new type of medication that inhibits renin in the arteris?
|
Tekturna (aliskiren)
-prevents vasoconstriction by angiotension II |
|
|
What does renin do?
|
splits angiotensinogen into angiotensin I which is further split into angiotensin II by ACE
|
|
|
What is the target BP for diabetic hypertensive patients?
|
<130/85
|
|
|
What should be part of the initial treatment for diabetic hypertensive patients?
|
ACE-I
|
|
|
What are 2 types of HTN drugs that are less effective in black patients?
|
ACE-I and ARBs
initial therapy should include a diuretic |
|
|
What is the goal of hypertensive emergencies?
|
partial reduction of BP with relief of symptoms
|
|
|
What is a type of hypertensive emergency characterized by encephalopathy or nephropahty and papilledema?
|
malignant hypertension (parenteral therapy)
|
|
|
What can excessive reductions in BP (treating a hypertensive emergency) trigger?
|
ischemia
|
|
|
If BP not lowered within 1 hour of a hypertensive emergency then what are some serious complications that can occur?
|
encephalopahty, nephropathy, intracranial hemorrhage, aortic dissection, pre-eclampsia/eclampsia
|
|
|
What are 10 types of parenteral agents that can be given for a hypertensive emergencies?
|
**nitroprusside sodium IV**, nitroglycerin IV (ischemia), **labetalol IV (pregnancy)**, esmolol IV, nicardipine IV (Ca2+ channel blocker), fenoldopam, enalaprilat, diazoxide (eclampsia), hydralazine IV/IM, diuretic IV (heart failure or fluid retention)
|
|
|
What are 3 types of oral agents that can be given for hypertensive emergencies?
|
*clonidine
*captopril nifedipine (unpredictable) |
|
|
Which type of oral agent given for hypertensive emergencies may cause sedation and rebound hypertension?
|
clonidine
|
|
|
What is considered a hypertensive emergency?
|
severe HTN (SBP >220 or DBP >125) or with optic disk edema, target organ complications, and severe perioperative HTN
|
|
|
What are 2 types of cerebrovascular incidences that have increased HTN?
|
vascular dementia and Alzheimer's
|
|
|
What are 2 types of diuretic drugs used for HTN?
|
HCTZ
Furosemide (Lasix) |
|
|
What type of HTN medication cannot be given to pregnant women?
|
arteriolar dilators (Hydralazine & Minoxidil)
|
|
|
What are 19 disorders of the blood vessels?
|
abdominal aortic aneurysm
thoracic aortic aneruysm popliteal aneurysm femoral aneurysm mesenteric aneurysm renal artery aneurysm aortic dissection LE occlusive disease carotid dissection carotid artery aneurysm visceral artery insufficiency arterial embolism acute arterial thrombosis Buerger's disease Raynaud's disease varicose veins superficial thrombophlebitis chronic venous insufficiency |
|
|
What is an aneurysm?
|
weakened wall of vessel --> increases in diameter (don't want it to rupture)
|
|
|
Where do most abdominal aortic aneurysms originate?
|
below the renal arteries (over 90%)
|
|
|
What is the normal diameter of an artery and what diameter indicates that it is an aneurysm?
|
normal diameter 2cm
aneurysm >3cm |
|
|
What are essentials (signs and symptoms) of diagnosis for symptomatic abdominal aortic aneurysm?
|
most are asymptomatic
symptomatic aneurysms-mid back or abdominal pain with a prominent aortic pulsation |
|
|
What are signs and symptoms of a ruptured abdominal aortic aneurysm?
|
severe back, abdominal or flank pain and hypotension (not a good prognosis)
|
|
|
What is the screening study of choice for an abdominal aortic aneurysm?
|
ultrasound
|
|
|
What are 3 types of imaging that can be done for an abdominal aortic aneurysm?
|
ultrasound
contrast enhanced CT scan MRI (if can't tolerate contrast) |
|
|
What is the treatment of choice for an abdominal aortic aneurysm?
|
surgical excision and synthetic graft placement for aneurysms > 5cm in diameter
|
|
|
What are 2 types of standard therapies that can be done for an abdominal aortic aneurysm?
|
surgical excision
endovascular repair |
|
|
What type of complication of an abdominal aortic aneurysm can be detected by contrest CT?
|
persistent endoleak
|
|
|
What is the prognosis for an abdominal aortic aneurysm?
|
mortality is 1-5% following aneurysm repair
5 years survival rate is 60-80% 5-10% will develop another aortic aneurysm |
|
|
Generally where is the pain (if present) for a thoracic aortic aneurysm?
|
substernal, back, or neck pain
|
|
|
What type of imaging is used for a thoracic aortic aneurysm?
|
CT and MRI (most accurate)
aortography may be necessary |
|
|
What are 3 indications for surgery for a thoracic aortic aneurysm?
|
presence of symptoms
rapid expansion size greater than 5cm |
|
|
What is the prognosis for a thoracic aortic aneurysm?
|
5 year survival rate is 20-25% without repair for aneurysms > 6.0
most deaths are due to rupture |
|
|
What does endovascular repair for a thoracic aortic aneurysm reduce?
|
cardiopulmonary risk
|
|
|
With thoracic aortic aneurysms, what is 5-30% of paraplegias due to?
|
great radicular artery
|
|
|
Is popliteal and femoral aneurysm more common in men or women? What age group?
|
men > 50 years
|
|
|
What is the diagnostic study of choice for popliteal aneurysms and which study is required before surgery?
|
ultrasound
MRA |
|
|
When is surgery indicated for popliteal aneurysms?
|
symptomatic aneurysms or ones > 2.0cm
|
|
|
What are symptoms of popliteal aneurysms due to?
|
arterial thrombosis, peripheral embolization or compression of adjacent structures
|
|
|
If a graft is used for bypass for a popliteal aneurysm, which vein is generally used?
|
saphenous
|
|
|
What does a femoral aneurysm present like?
|
pulsatile groin masses
|
|
|
What may pseudoaneurysms result from?
|
injury due to IV drug abuse or femoral line insertion
|
|
|
Which type of aneurysm historically has a high mortality rate?
|
mesenteric aneurysm
|
|
|
What may mesenteric aneurysms be related to? (3)
|
blunt trauma, trauma during abdominal surgeries, pregnancy
|
|
|
Does mesenteric aneurysms affect more men or women?
|
women 4 x more than men
|
|
|
What are most superior mesenteric aneurysms associated with? (2)
|
infective endocarditis and septic emboli
|
|
|
What type of imaging for mesenteric aneurysms has increased detection rate and therefore reduced mortality?
|
CT scanning
|
|
|
When is surgery indicated for mesenteric aneurysms?
|
symptomatic aneurysms or those > (or equal to) 2.0cm
|
|
|
What group of people has the highest risk of rupture of a mesenteric aneurysm?
|
young women during pregnancy
|
|
|
What is the most common aortic catastrophe?
|
aortic dissection
-caused by an intimal teat |
|
|
What are 2 conditions that may be present with an aortic dissection?
|
HTN or Marfan's syndrome
|
|
|
What are the signs/symptoms of aortic dissection?
|
sudden severe chest pain with radiation to the back
appears in shock, but BP is normal or elevated 85% report sudden excruciating "ripping" pain in the chest or upper back peripheral pulses may be unequal |
|
|
What are the 2 types of aortic dissection?
|
type A-just distal to aortic valve
type B-just distal to left subclavian artery |
|
|
What type of imaging should be done for an aortic dissection?
|
TEE is highly sensitive and specific
|
|
|
What differentiates an aneurysm from and aortic dissection?
|
pain (aortic dissection)
|
|
|
With aortic dissection, what type of medication can be given for pain relief? To decrease heart rate?
|
opioids
beta blockers |
|
|
With the 2 types of aortic dissections: type ___ should undergo emergent repair; type ___ can undergo medical treatment.
|
A
B |
|
|
What is the prognosis for an aortic dissection?
|
5 year survival rate post surgery
all patients who do not have surgery should have annual CT or MRI scan |
|
|
Which type of blood vessel disorder is a common cause of disability?
|
LE occlusive disease
|
|
|
How many distinct patterns of LE occlusive disease are there?
|
3
|
|
|
What is Leriche's syndrome?
|
triad of bilateral hip and buttock claudication, ED, absent femoral pulses
|
|
|
What are some signs and symptoms of LE occlusive disease?
|
impotence, claudication, rest pain (usually nocturnal), gangrene, Leriche's syndrome, ABI less than 0.8, atrophy of the skin and muscles of the calf, dependent rubor, hair loss and coolness of the skin, painful ulcers
|
|
|
What are 3 types of imaging techniques for LE occlusive disease?
|
angiography prio ro surgery
MRA or duplex U/S x-rays to r/o osteomyelitis |
|
|
What is rubor (LE occlusive disease)?
|
legs red when dangling and white when elevated
|
|
|
Are painful ulcers from an artery or vein?
|
artery
|
|
|
Are unpainful ulcers from an artery or vein?
|
vein
|
|
|
What are 5 medications that can be used for treatment of LE occlusive disease?
|
lipid-lowering meds.
Cilostazol (Pletal) ASA Clopidogrel (Plavix) Viagra (for ED) |
|
|
What are 2 types of surgeries that can be performed for LE occlusive disease?
|
endovascular techniques using stent angioplasty
open surgery -aortobifemoral bypass graft -saphenous vein graft -thromboendarterectomy |
|
|
What is the prognosis for LE occlusive disease?
|
25% with claudication will develop rest pain or ulcers
5 year survival rate of 50% related to coexisting cardiovascular disease collateral circulation will develop in some patients |
|
|
What type of blood vessel disorder has a false channel in the wall of the carotid artery caused by a tear in the intima?
|
carotid dissection
(can be spontanous or traumatic) |
|
|
*What is the classic triad of symptoms for carotid dissection?
|
unilateral neck pain or headache
stroke or TIA incomplete Horner syndrome (miosis, and ptosis but no anhidrosis) |
|
|
What is the primary treatment for a carotid dissection?
|
anticoagulation to INR between 2-3
|
|
|
Which type of blood vessel disorder is more common in the intracerebral portion than the cervical portion and has a pulsatile mass in the neck?
|
carotid aneurysm
|
|
|
Which diagnosis confirms a carotid aneurysm?
|
angiography
|
|
|
Which blood vessel disorder is associated with atherosclerosis or trauma; or mycotic aneurysm; neck pain, cranial nerve dysfunction, TIA or stroke?
|
carotid aneurysm
|
|
|
When is surgery indicated for a carotid aneurysm?
|
for penetrating trauma, neurologic deficit, mycotic aneurysms, or > 2cm
|
|
|
What are 4 conditions that are associated with visceral artery insufficiency?
|
chronic intestinal ischemia
acute intestinal ischemia mesenteric vein occlusion ischemic colitis |
|
|
Which condition has bouts of crampy lower abdominal pain and bloody diarrhea?
|
ischemic colitis (must be distinguished from IBD)
|
|
|
atrial fibrillation
|
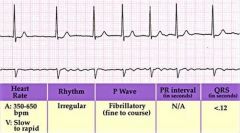
What does this picture show?
|
|
|
atrial flutter
|
What does the picture show?
|
|
|
bigeminy (ventricular extrasystole)
|
What does the picture show?
|
|
|
third degree AV block (complete heart block)
|
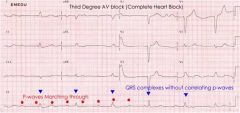
What does the picture show?
|
|
|
first degree AV block
|
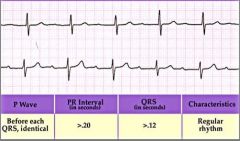
What does the picture show?
|
|
|
second degree heart block (Mobitz type II)
|
What does the picture show?
|
|
|
normal sinus rhythm
|
What does the picture show?
|
|
|
Torsades de Pointes (ventricular tachycardia)
|
What does the picture show?
|
|
|
trigeminy (ventricular extrasystoles)
|
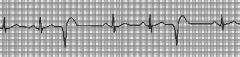
What does the picture show?
|
|
|
ventricular fibrillation
|
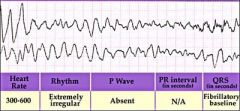
What does the picture show?
|
|
|
ventricular tachycardia
|

What does the picture show?
|
|
|
second degree heart block-Mobitz type I (Wenckebach)
|
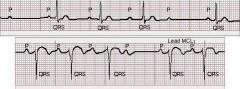
What does the picture show?
|
|
|
What type of arrhythmia may occur with fever, exercise, emotion, pain, anemia, heart failure, shock, thyrotoxicosis or response to drugs; can also been seen with alcohol and alcohol withdrawal?
|
sinus tachycardia
|
|
|
What type of arrhythmias is seen with valvular heart disease, dilated cariomyopathy, ASD, hypertension and CHD, or in normal hearts?
|
atrial fibrillation
|
|
|
What is the drug of choice for rate control and rhythm with atrial flutter?
|
amiodarone
|
|
|
Which type of arrhythmia may be difficult to distinguish from SVT, may be sustained or nonsustained, and may be asymptomatic or cause syncope?
|
ventricular tachycardia
|
|
|
Which type of arrhythmia has over 75% of patients with severe CAD and patients who survive need exercise stress testing or coronary arteriography?
|
ventricular fibrillation
|
|
|
What is the most effective drug for long QT syndrome?
|
beta blockers
|
|
|
What type of syndrome may be secondary to antiarrhythmic or antidepressant drugs, electrolyte abnormalities, myocardial ischemia, or bradycardia?
|
acquired long QT syndrome
|
|
|
What can acquired long QT syndrome lead to?
|
v-tach, especially torsades de pointes
|
|
|
How is acquired long QT syndrome treated?
|
IV beta blockers
temporary ventricular pacing |
|
|
Which type of AV block may occur in normal patients with heightened vagal tone, may also occur as a drug effect, and prognosis is usually good?
|
first degree or second degree-Mobitz type I (Wenckebach)
|
|
|
Which type of AV block has PR intervals that are the same length for all of the conducted beats and prophylactic pacing is required?
|
second degree-Mobitz type II
|
|
|
Which type of AV block has a wide QRS complex, slow ventricular rate (usually <50), exercise does not increase the rate, and patients may complain of weakness of dyspnea?
|
third degree-complete heart block
|
|
|
Which type of blood vessel disorder is caused by atherosclerosis (usually older males) or fibromuscular dysplasia (young women)?
|
renal artery stenosis
|
|
|
What is the initial screening for renal artery stenosis?
|
duplex U/S or MRA
|
|
|
With renal artery stenosis, ___ is required before surgery, ___ with stenting; if not effective, surgery to ___ diseased artery; ___ may be required if there is renal atrophy.
|
angiography
angioplasty bypass nephrectomy |
|
|
What are the 6 P's of acute ischemia associated with arterial embolism?
|
pain
pallor pulselessness paresthesias poikilothermia paralysis |
|
|
What are the usual causes of arterial embolism? (3)
|
a-fib
rheumatic heart disease valvular prostheses |
|
|
What is the treatment plan for arterial embolism?
|
heparin started as soon as diagnosis made
emergent embolectomy with balloon catheter lifelong anticoagulation recommended |
|
|
Which type of blood vessel disorder is most commonly a complication of chronic atherosclerotic disease?
|
actue arterial thrombosis
|
|
|
What is the treatment plan for actue arterial thrombosis?
|
injection of alteplase directly into the thrombus through a catheter
limb salvage rate is almost 90% if related to trauma, surgical repair is required |
|
|
What is another name for thromboangiitis obliterans?
|
Buerger's Disease
|
|
|
Which blood vessel disorder has episodic and segmental inflammatory and thrombotic process of the peripheral arteries and veins?
|
Buerger's disease
|
|
|
Which blood vessel disorder is more common in men under age 40 who smoke, especially Eastern European or Asian background?
|
Buerger's disease
|
|
|
Which type of blood vessel disorder causes occlusion of the distal arteries with claudication rest pain and necrosis?
|
Buerger's disease
|
|
|
Which blood vessel disorder has migratory superficial thrombophlebitis, is never confined to one limb, and has a episodic clinical course?
|
Buerger's disease
|
|
|
What does the prognosis of Buerger's disease depend on and what can be used as pain control?
|
smoking cessation
NSAIDs or opioids |
|
|
What type of procedure can be done to reduce vasospasms in Buerger's disease patients?
|
sympathectomy
|
|
|
Which type of blood vessel disorder is also known as Takayasu's disease?
|
pulseless disease
|
|
|
Which blood vessel disorder is most common in Asian women under the age of 40 and has rare polyarteritis of unknown cause?
|
pulseless disease
|
|
|
What can pulseless disease cause? (3)
|
segmental stenoses, occlusions, and aneurysms
|
|
|
What is essential for the diagnosis of pulseless disease?
|
angiography
|
|
|
With pulseless disease, what is used to control symptoms and limit progression of the disease?
|
corticosteroids (reduce inflammation)
|
|
|
Is Raynaud's disease more common in men or women?
|
women (70-80% are women)
|
|
|
What are the essentials of diagnosis for Raynaud's disease?
|
episodic BILATERAL digital pallor, cyanosis, and rubor (red, white, blue)
precipitated by cold or emotional stress, relieved by warmth |
|
|
Raynaud's phenomenon is associated with ___ disease.
|
autoimmune (worse prognosis than Raynaud's disease)
|
|
|
Is Raynaud's disease or phenomenon benign and completely reversible between attacks?
|
Raynaud's disease
|
|
|
Will Raynaud's disease or phenomenon possibly progress to atrophy and fingertip gangrene?
|
Raynaud's phenomenon
|
|
|
What type of test can be done to assess for arterial occlusive disease?
|
Allen test
|
|
|
What are 8 types of treatment for Raynaud's disease?
|
-warmth/protection of hands
-moisturizers -stop smoking (vasoconstrictor) -stress management -discontinue oral contraceptives, beta blockers, and ergotamines (if needed) -ASA to reduce risk of thrombosis -vasodilators (nifedipine or prozac) -surgery (reconstruction, sympathectomy) |
|
|
What are the essentials of diagnosis for varicose veins? (3)
|
-dilated tortuous superficial veins
-fatigue and discomfort -increase frequency after pregnancy |
|
|
15% of adults will develop ___ veins varicosities?
|
saphenous (long saphenous vein > short saphenous vien)
|
|
|
What are 5 risk factors for varicose veins?
|
female gender
pregnancy family history prolonged standing history of phlebitis |
|
|
What are the S/S of varicose veins? (5)
|
-dull, aching heaviness
-itching -tortuous, dilated veins visible when patient stands -telangiectasias and spider veins -signs of chronic venous insufficiency |
|
|
What are 3 nonsurgical treatments for varicose veins?
|
compression stockings
leg elevation regular exercise |
|
|
What are 3 indications for surgery of varicose veins?
|
persistent pain
recurrent thrombophlebitis chronic venous insufficiency |
|
|
What are 3 types of treatment that can be performed for varicose veins?
|
-stab avulsion surgery
-endovenous radiofrequency ablation -compression sclerotherapy (inject something to cause veins to stick together) |
|
|
What is the recurrence rate after procedure for varicose veins?
|
about 10%
other veins may become varicose |
|
|
What are the essentials of diagnosis for superficial thrombophlebitis?
|
induration, erythema and tenderness along a superficial vein
often history of recent IV or trauma may occur spontaneously with varicose veins or in pregnancy |
|
|
What are the S/S of superficial thrombophlebitis?
|
dull pain, erythema, induration and tenderness over vein
chills and high fever suggest septic complication |
|
|
What is the prognosis for superficial thrombophlebitis?
|
generally a benign and brief condition
|
|
|
What are the types of treatment for superficial thrombophlebitis?
|
-NSAIDS, local heat, & elevation
-ambulation -excision of the vein segment if it recurs or persists -IV antibiotics for septic thrombophlebitis |
|
|
What are the essentials of diagnosis for chronic venous insufficiency?
|
-history of phlebitis or leg injury
-ankle edema is earliest sign -late signs: stasis pigmentation, dermatitis, varicosities, and ulceration |
|
|
What is chronic venous insufficiency most often secondary to?
|
DVT
|
|
|
Does a venous or arterial ulcer have a more irregular border and is thicker and dryer and generally painless?
|
venous
|
|
|
Does a venous or arterial ulcer have a more round border and is generally thinner and painful?
|
arterial
|
|
|
What are the S/S of chronic venous insufficiency?
|
-progressive edema of the leg that begins at the ankle
-dull, aching pain -worse at the end of the day, better with elevation -varicosities often present -stasis dermatitis -brownish pigmentation -brawny induration |
|
|
What is the #1 treatment of chronic venous insufficiency?
|
prevention!
|
|
|
How can chronic venous insufficiency be prevented? (4)
|
elevation of legs at night and intermittently during the day; avoid long periods of sitting or standing; compression stockings; exercise
|
|
|
What is the prognosis for chronic venous insufficiency?
|
commonly progressive
can be managed but not cured |
|
|
How can stasis dermatitis associated with chronic venous insufficiency can be treated?
|
strict bedrest with leg elevation and saline compresses
antibiotics/antifungals if indicated |
|
|
What are 2 ways to treat ulcers associated with chronic venous insufficiency?
|
unna boot
surgical debridement with skin graft for very large ulcers |
|
|
What is systolic function of the heart governed by? (4)
|
myocardium contraction
preload of the ventricle afterload heart rate |
|
|
What is the normal ejection fraction of the left ventricle?
|
60% (below becomming heart failure)
|
|
|
What are 5 types of congestive heart failure?
|
high-output heart failure
diastolic dysfunction systolic dysfunction right sided heart failure left sided heart failure |
|
|
Which type of heart failure is uncommon but occurs when the cardiac pump function may be supranormal but nonetheless inadequate when metabolic demands or requirements for blood flow are excessive?
|
high-output heart failure
|
|
|
Which type of heart failure involves abnormal filling of the LV or RV either because of myocardial relaxation is impaired or because the chamber is noncompliant ("stiff")?
|
diastolic dysfunction
|
|
|
Which type of heart failure involves patients who have symptoms of low cardiac output and elevated pulmonary venous pressure; dyspnea is the predominant feature?
|
left heart failure
|
|
|
Which type of heart failure shows signs of fluid retention and the patient exhibits edema, hepatic congestion, and on occasion, ascites?
|
right heart failure
|
|
|
What is the primary cause of right heart failure?
|
left heart failure
|
|
|
What is right heart failure secondary with?
|
Cor Pulmonale
|
|
|
What are some of the etiologies congestive heart failure? (9)
|
myocardial infarction
ischemic cardiomyopathy systemic HTN CAD alcoholic cardiomyopathy valvular heart disease hyperthyroidism hypothyroidism |
|
|
What are 5 preventitive measures for HTN?
|
early detection and intervention
control HTN control hypercholesterolemia reduction of EtOH control of DM |
|
|
Which stage of heart failure involves patients at high risk due to the presence of conditions; no identified structural or functional abnormalities of the pericardium, myocardium or cardiac valves and have never shown symptoms or signs of heart failure?
|
A
|
|
|
Which stage of heart failure involves patients who have developed structural heart disease; have never shown S/S of heart failure?
|
B
|
|
|
Which stage of heart failure involves patients who have current or prior symptoms of heart failure associated with underlying structural heart disease?
|
C
|
|
|
Which type of heart disease involves patients with advanced structural heart disease and marked symptoms of heart failure at rest despite maximal medical therapy and who require specialized interventions?
|
D
|
|
|
What can improve the mortality for CHF?
|
ACE-I and beta blockers
|
|
|
What is the prognosis for heart failure?
|
poor prognosis
5 year survival is <50% increased mortality w/ CAD |
|
|
What are the 4 categories of heart failure?
|
I asymptomatic
II symptomatic with moderate activity III symptomatic with mild activity IV symptomatic at rest |
|
|
What are the symptoms of heart failure?
|
SOB (majority)
exertional dyspnea orthopnea PND dyspnea at rest chronic non-productive cough nocturia fatigue exercise intolerance RUQ discomfort anorexia nausea |
|
|
Will a patient with CHF show signs of sympathetic or parasympathetic nervous system activity?
|
sympathetic
|
|
|
A patient with severe heart diesease (heart failure) may appear comfortable at ___, dyspneic with conversation or minor ___, cachectic, cyanotic, ___cardia, ___tension, and ___pulse pressure.
|
rest
activity tachy- hypo- reduced |
|
|
Patients with CHF may show signs of ___ venous pressure, abnormal pulsations of ___ artery, abnormal lung sounds (crackles or absent), and pleural effusions.
|
increased
carotid |
|
|
Patients with CHF may show signs of expiratory ___, hepatomegaly, abnormal heart sounds, and ___ peripheral edema (most often on lower extremities).
|
wheezing
pitting |
|
|
What are 4 labs that can be done for CHF?
|
complete blood count (CBC)
chemistry panel (CMP) thyroid-stimulating hormone (TSH) serum beta-natiuretic peptide (BNP) |
|
|
What are 6 types of diagnostics that can be done for CHF?
|
labs
EKG chest x-ray echocardiogram angiography cardiac catheterization |
|
|
What does a CXR for CHF show?
|
increased cardiac silhouette
dilation of upper lobe veins haziness of vessel outlines interstitial edema pleural effusions chronic HF may be normal |
|
|
What does the pharmacologic treatment for CHF include? (10)
|
diuretics (Lasix or Spironalectone)
ACE-I ARB spironolactone beta blockers glycosides vasodilators inotropic agents calcium channel blockers anticoagulation |
|
|
What does the non-pharmacologic treatment for CHF include? (9)
|
case management
dietary restrictions exercise and rehabilitaion coronary revascularization cardiac pacing cardiac transplantation cardiomyoplasty ventriculr reduction surgery palliative care |
|
|
What are the essentials of diagnosis for acute heart failure and pulmonary edema?
|
acute onset
worsening dyspnea at rest tachycardia diaphoresis cyanosis (distal/periorbital) pulmonary rales, rhonchi expiratory wheezing arteriolar hypoxemia |
|
|
What does an x-ray generally show for acute heart failure and pulmonary edema?
|
cardiomegaly
|
|
|
What are 5 typical causes of acute cardiogenic pulmonary edema?
|
acute myocardial infarction
severe ischemia exacerbation of CHF volume overload mitral stenosis |
|
|
What are the 5 most common causes of acute cardiogenic pulmonary edema?
|
discontinuation of med.
excessive salt intake myocardial ischemia tachyarrhythmias (a-fib) infections |
|
|
What are 5 clinical findings of acute CHF?
|
severe dypnea
pink, frothy sputum (bubbly) diaphoresis cyanosis rales in all lung fields |
|
|
How should acute CHF be treated?
|
-place patient in sitting position with dependant legs
-supplemental oxygen -morphine (vasodilator) -diuretic (Lasix) -nitrates (nitroglycerin sublingual) -after patient is stabilized treat the underlying cause |
|
|
Which type of heart failure occurs when the heart is pumping normal or even above normal amounts of blood, but still can't meet the demands of the body because the oxygen demands are unusually high or the blood is unusually low in oxygen?
|
high output heart failure
|
|
|
What are 3 causes of high output heart failure?
|
thyrotoxicosis
severe anemia arteriovenous shunting |
|
|
What are 3 types of cardiac infections?
|
infectious endocarditis
rheumatic fever acute pericarditis |
|
|
What are 6 essentials of diagnosis for infectious endocarditis?
|
pre-existing organic heart lesion
fever new/changing heart murmur evidence of systemic emboli positive blood culture vegetation on echocardiogram |
|
|
What are 3 factors that determine the clinical presentation of infectious endocarditis?
|
type of infecting organism
valve involved route of infection |
|
|
What is are the common organisma that causes infectious endocarditis? (2)
|
*S. aureus (normally located on the skin)
Strep virdans |
|
|
What are the 2 types of infectious endocarditis?
|
native valve endocarditis
prosthetic valve endocarditis |
|
|
What are 2 epidemiologies of infectious endocarditis?
|
IV drug use
underlying valvular disease |
|
|
What are 3 S/S of infectious endocarditis?
|
-febrile illness lasting several days to 2 weeks
-new/changing heart murmur -peripheral lesions (5) |
|
|
What are 5 characteristic peripheral lesions that may be seen with infectious endocarditis?
|
-petechiae (palate or conjunctiva)
-subungal "splinter" hemorrhages -osler nodes (painful) -Janeway lesions (painless) -Roth spots (retina) |
|
|
What are 3 types of laboratory tests that can be done for infectious endocarditis?
|
blood cultures
CBC urinalysis |
|
|
What are the Duke criteria to make a definitive diagnosis of infectious endocarditis?
|
must have 2 major, 1 major + 3 minor, or 5 minor
|
|
|
What are the Duke criteria for infectious endocarditis?
|
Major criteria:
-2 pos. blood cultures for typical organism -pos. echo -new regurgent murmur Minor criteria: -predisposing condition (ex. prolapse) -fever >38 (100.4) -embolic disease -immunologic phenomena -blood culture pos. for other organism |
|
|
Which type of echocardiography is more sensitive for infectious endocarditis?
|
transesophageal (90%)
|
|
|
What is the antibiotic treatment plan for infectious endocarditis?
|
-nafcillin+penicillin+gentamicin
-vancomycin (if PCN allergy or MRSA suspected) -regimen tapered to culture results when available |
|
|
What type of surgery can be done for infectious endocarditis and what are the 4 indications for it?
|
valve replacement
-valvular regurgitation resulting in acute heart failure that doesn't respond quickly to antibiotics -fungal endocarditis -infections not responding to appropriate antibiotics after 7-10 days -recurrent infections with the same organism |
|
|
What are 6 complications of infectious endocarditis?
|
-destruction of infected heart valves
-myocardial abscesses -systemic embolization -metastatic infectiouns mycotic aneurysm (fungal or bacteria) -septic pulmonary emboli in right-sided endocarditis |
|
|
What is prophylaxis of infectious endocarditis recommended for?
|
-prosthetic cardiac valves
-previous bacterial endocarditis with or without heart disease -most congenital cardiac arrhythmias -rheumatic and other acquired valve dysfunctions -hypertrophic cardiomyopathy -mitral valve prolapse with regurgitation |
|
|
What medication can be given for adult prophylaxis of infectious endocarditis?
|
amoxicillin
clindamycin or azithromycin/clarithromycin if PCN allergy |
|
|
What is the peak incidence ages of acute rheumatic fever?
|
5-15 years
|
|
|
What criteria is the diagnosis of acute rheumatic fever based on?
|
Jones criteria
|
|
|
What does acute rheumatic fever commonly follow?
|
GABHS (group A beta hemolytic Strep.) infection of the pharynx
|
|
|
What can acute rheumatic fever lead to?
|
progressive valvular deformity
|
|
|
Which valve does acute rheumatic fever most commonly affect?
|
mitral valve
|
|
|
What are the Jones criteria for acute rheumatic fever?
|
Major criteria:
-carditis -erythema marginaturm and subcutaneous nodules -Sydenham's chorea (involuntary movements) -polyarthritis Minor criteria: -fever >38 (100.4) -polyarthalgias (pain without inflammation) -reversible PR prolongation -elevated sed rate or elevated CRP |
|
|
What are 2 complications of acute rheumatic fever?
|
-acute CHF in severe cases
-development of rheumatic heart disease long term |
|
|
What is the treatment plan for acute rheumatic fever?
|
-strict bedrest
-ASA -PCN (depot shot) -erythromycin (if allergic to PCN) -short course of corticosteroids if joint pain does not respond to ASA |
|
|
What type of prevention can be done for rheumatic fever?
|
-prevention of initial episode by early treatment of GABHS infections
-prevention of recurrence is critical |
|
|
How long may rheumatic fever last?
|
initial episode may last for months in children or weeks in adults
|
|
|
Presence of ___ in initial episode of rheumatic fever indicates a poorer prognosis?
|
carditis
|
|
|
What is the prognosis for rheumatic fever?
|
-immediate mortality rate is low
-30% of children with recurrences will die within 10 years -2/3 of patients will have detachable valvular abnormalities |
|
|
What are the 7 etiologies of pericarditis?
|
*viral
bacterial atypical malignancy systemic disease medications immunologic |
|
|
What are the essentials of diagnosis for acute pericarditis?
|
-anterior pleuritic chest pain (worse when supine)
-pericaridal rub -fever -elevated sed rate -diffuse ST segment elevation with associated PR depression |
|
|
What are 6 etiologies of pericarditis?
|
-viral (coxsackie, echovirus)
-bacterial -systemic (autoimmune, uremia) -neoplasm -radiation -drug toxicity (minoxidil, PCN) |
|
|
Is pericarditis greater in men and women?
|
men (usually under age 50)
|
|
|
What are the S/S of pericarditis? (4)
|
-chest pain (usually pleuritc and relieved by sitting forward)
-dyspnea -fever -pericardial friction rub |
|
|
pericarditis
|
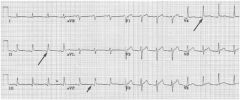
What does the picture show?
|
|
|
What is the treatment plan for pericarditis?
|
analgesics
NSAIDs (corticosteriods if unresponsive) diuretic pericardiocentesis antibiotics |
|
|
What are 2 complications of acute pericarditis?
|
pericardial tamponade
constrictive pericarditis (pericardium doesn't stretch b/c it gets fibrotic --> heart can't beat as effectively) |
|
|
What type of condition results from pericardial effusions with elevated intrapericardial pressure >15mmHg
|
cardiac tamponade
|
|
|
What does cardiac tamponade restrict?
|
venous return and ventricular filling
may result in shock or death |
|
|
What are 6 S/S of cardiac tamponade?
|
dyspnea and cough
tachycardia tachypnea narrow pulse pressure relatively normal systolic pressure pulsus paradoxus |
|
|
What is the most sensitive test for cardiac tamponade?
|
echocardiogram
|
|
|
What type of diagnostic test can be used for diagnosis and treatment of cardiac tamponade?
|
pericardiocentesis
|
|
|
What are 2 types of treatment that can be done for cardiac tamponade?
|
urgent pericardiocentesis
pericardial window to prevent recurrences |
|
|
For acute rheumatic fever how many major/minor criteria must be met to establish diagnosis?
|
must have 2 major, or 1 major + 2 minor
|

