![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
45 Cards in this Set
- Front
- Back
|
Outline the mechanism by which arrythmias arise in heart failure
|
rapid ventricular response & loss of effective atrial contraction → systolic failure
• All arrythmias are more frequent in HF • The more severe the underlying heart disease, the more severe & frequent the arrythmias • Tx of HF must include Tx of arrythmia ^TG |
|
|
Give an example of an arrythmias that causes heart failure. (rare)
|
SVT
(control of the arrythmia can completely reverse HF) ^TG |
|
|
Bradyarrythmias, examples?
|
heart block
^TG |
|
|
Tachyarrythmias, examples?
|
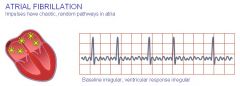
AF
atrial flutter with rapid ventricular response ^TG |
|
|
Types of atrial tachyarrythmias in HF?
|
AF > atrial flutter
^TG |
|
|
Pathophysiology of atrial tachyarrythmias in HF?
|
atrial enlargement → proarrhythmic effect of atrial stretch
^TG |
|
|
Management of substantial atrial enlargement
|
Maintenance of sinus rhythm following reversion is unlikely long term
Therapeutic Options: * ventricular rate control & antithrombotics ^TG |
|
|
Most sudden deaths in HF is due to
|
ventricular fibrillation ± preceding ventricular tachycardia
^TG |
|
|
All antiarrythmic drugs are
|
proarrythmic
^TG |
|
|
Antiarrythmic drugs can exacerbate which type of arrythmias?
|
Bradyarrythmias
^TG |
|
|
What is the drug of choice to suppress symptomatic ventricular arrythmias in heart failure?
|
amiodarone
^TG |
|
|
Patients with life-threatening ventricular arrythmias should be considered for?
|
Implantable cardioverter-defibrillator (ICD)
^TG |
|
|
Tx Approach to arrythmias in HF?
|
• avoid K+ depletion from diuretics (K+ > 4mM, optimally at 5mM)
• avoid Mg2+ depletion from diuretics • ACEI / ARB • Beta blocker • Avoid cardiac stimulants (milrinone, beta agonists) because of proarrythmic risk • Avoid class 1 antiarrythmics (flecainide) ^TG |
|
|
Pacemaker vs. ICD
|
Pacemaker - regulate HR such as in bradyarrythmias
ICD - monitors HR & rhythm → sends electric shocks when there are abnormalities |
|
|
Define 1st degree heart block
|
PR interval is fixed but > 0.2s
^djr im |
|
|
Define 2nd degree heart block (Mobitz type 1 or Wenckebach)
|
PR intervals progressively ↑ until a beat is dropped (P wave is not followed by QRS)
^djr im |
|
|
Define 2nd degree heart block (Mobitz type 2)
|
Fixed PR intervals with intermittent dropped QRS complexes
^djr im |
|
|
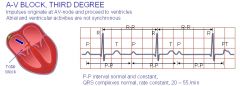
Define 3rd degree heart block (complete heart block)
|
* Dissociation between atrial & ventricular activity (no relationship between P waves & QRS intervals)
* Uniform P-P and R-R intervals ^djr im |
|
|
Tx for 1st degree heart block
|
no tx
|
|
|
Tx for 2nd degree heart block (Mobitz type 1 or Wenckebach)
|
cease offending drug
pacemaker if bradycardic |
|
|
Tx for 3rd degree heart block (complete heart block)
|
pacemaker
|
|
|
Tx for 2nd degree heart block (Mobitz type 2)
|
pacemaker to prevent progression to 3rd degree / complete heart block
|
|
|
Which drugs cause 2nd degree heart block?
|
digoxin
beta blockers CCB |
|
|
What is the most common chronic arrythmia?
|
AF
|
|
|
Types of Heart Block
|

|
|
|
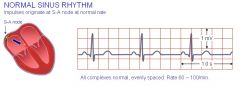
ECG Finding: normal sinus rhythm
|
|
|
|
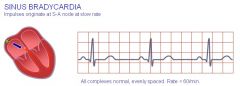
ECG Finding: sinus bradycardia
|
|
|
|
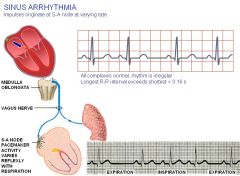
ECG Finding: sinus arrythmia
|
|
|
|
ECG Finding: AF
|
|
|
|
ECG Finding: Pacemaker Rhythm
|
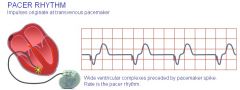
|
|
|
ECG Finding: First Degree AV Block
|
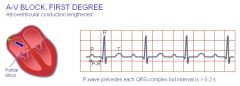
|
|
|
ECG Finding: 2nd degree AV Block
|
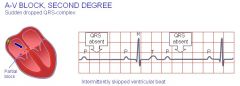
|
|
|
ECG Finding: RBBB
|
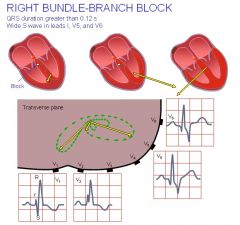
|
|
|
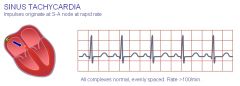
ECG Finding: Sinus Tachycardia
|
|
|
|
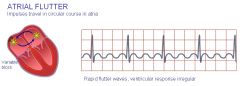
ECG Finding: atrial flutter
|
|
|
|
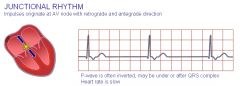
ECG Finding: junctional rhythm
|
|
|
|
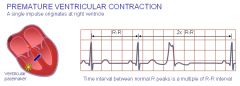
ECG Finding: premature ventricular contraction
|
|
|
|
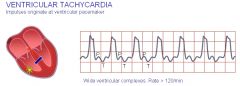
ECG Finding: ventricular tachycardia
|
|
|
|
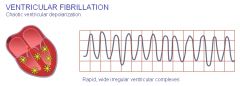
ECG Finding: ventricular fibrillation
|
|
|
|
ECG Finding: 3rd degree AV block
|
|
|
|
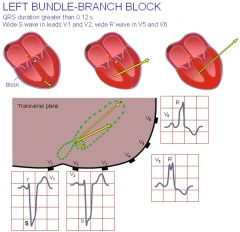
ECG Finding: LBBB
|
|
|
|
ECG Finding: LVH
|
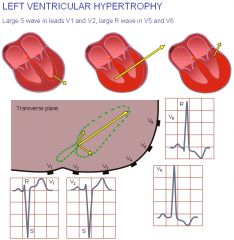
|
|
|
ECG Finding: R/L atrial hypertrophy
|
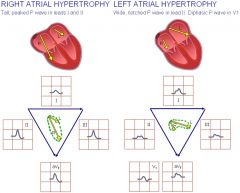
|
|
|
ECG Finding: RVH
|
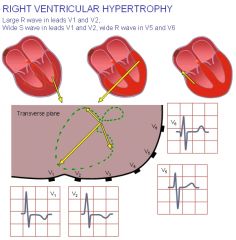
|
|
|
What are the 4 ECG changes with hyperkalemia & what is the order of progression?
|
absent p-wave
nodal rhythm Widened QRS complex Peaked T-waves V3-V4 Mild levels of hyperkalaemia are associated with acceleration of terminal repolarisation, resulting in T-wave changes. The most common changes seen in the T-waves are “tenting” or “peaking”, they are considered to be the earliest abnormalities seen in the ECG. Mild to moderate hyperkalaemia causes depression of conduction between adjacent cardiac myocytes, this results in prolongation of the PR and QRS intervals as potassium levels rise. P-wave amplitude disappears early because of the sensitivity of atrial myocytes to hyperkalaemia. As the severity of hyperkalaemia increases, there is further suppression of sinoatrial and atrioventricular conduction, resulting in the appearance of escape beats and escape rhythms. The QRS complex will continue to widen and may blend with the T-wave, creating a sine-wave appearance to the ECG. If the potassium level is allowed to rise without treatment, ventricular fibrillation will result. |

