![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
335 Cards in this Set
- Front
- Back
|
Characteristic radiation of pain from angina |
Left arm (can go to neck, jaw and back) |
|
|
Which troponin is used to measure myocardial ischemia? |
Troponin-I |
|
|
What does a Q-wave formation indicate? |
Prior MI |
|
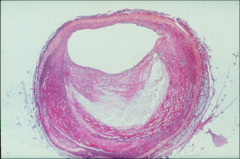
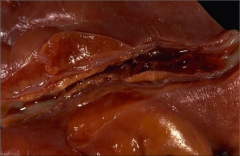
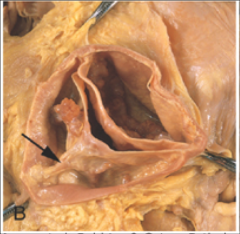
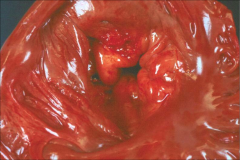
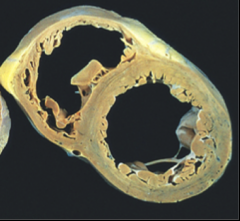
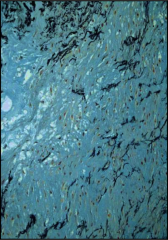
What's going on here? |
Atherosclerotic plaque |
|
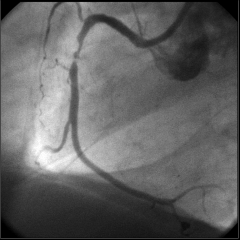
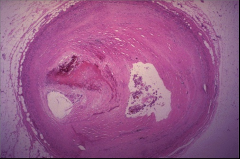
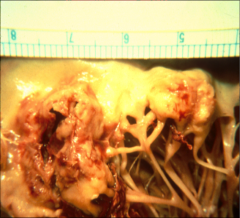
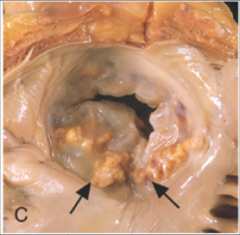
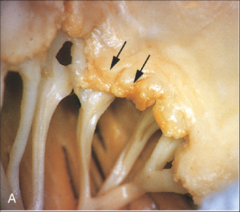
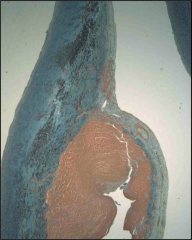
What's going on here? |
Unstable ulcerated coronary artery plaque |
|
|
Where are most coronary stenotic lesions? |
Proximal (i.e. closer to takeoff), epicardial |
|
|
Define right-dominant and left-dominant circulation. Which one is more common? |
Right-dominant: posterior descending coronary derived from the right coronary artery.
Left: derived from LCA.
R is more common |
|
|
What plaques are most prone to rupture? Define a vulnerable plaque. |
Take-home: plaques with larger core:cap ratio are most likely to rupture.
This means soft, newer plaques with high atherosclerotic content are more vulnerable.
Vulnerable plaque: >40% core |
|
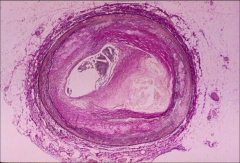
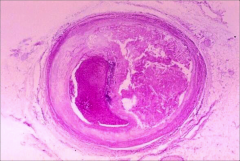
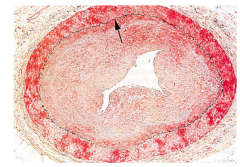
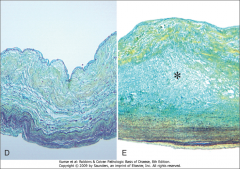
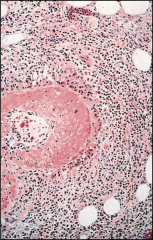
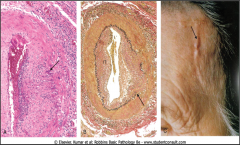
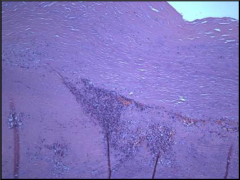
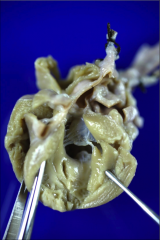
What's going on here? Identify key structures. |
Athereosclerotic plaque. |
|
|
Which vessel layers are implicated in the pathogenesis of atherosclerotic plaques? |
Intima AND media |
|
|
If you reduce the diameter of a vessel by 50%, you reduce the area by... |
75% |
|
|
Correlate degrees of coronary artery stenosis to clinical syndromes |
< 70-75%: asymptomatic |
|
|
Rupture vs. Erosion of plaque |
Erosion is a much less severe, superficial interruption; rupture implies exposure of the highly thrombogenic necrotic core to blood.
Ruptures are much more likely to be responsible for a STEMI. |
|
|
Macrophage role in plaque progression |
Macrophages release metallo-proteinases that contribute to destabilization and rupture |
|
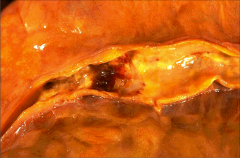
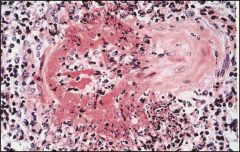
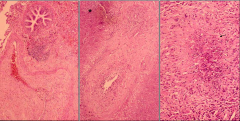
What's going on here? |
Ruptured plaque w/thrombus |
|
What's going on here? |
Coronary artery thrombus |
|

What's going on here? |
Coronary artery thrombus |
|
What's going on here? |
Recent Thrombosis With Total Occlusion |
|
What's going on here? |
Recanalized vessel after thrombus |
|
|
Why does a slow rate of occlusion have a better prognosis for MI? |
More collateral circulation |
|
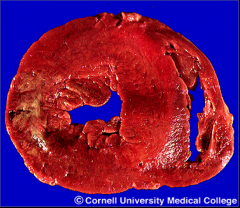
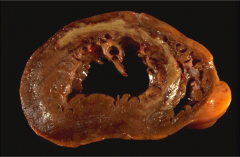
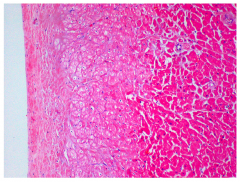
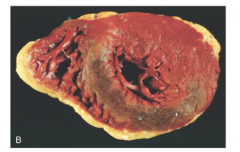
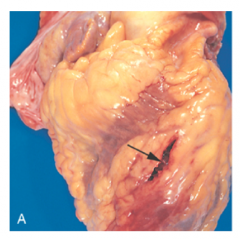
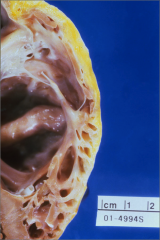
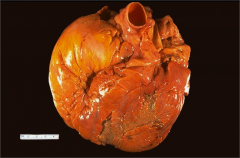
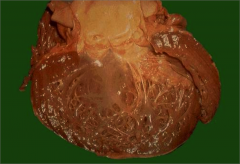
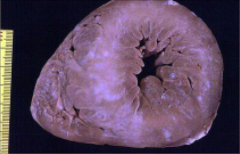
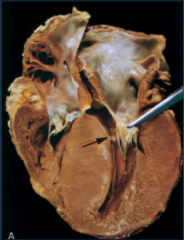
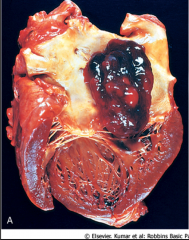
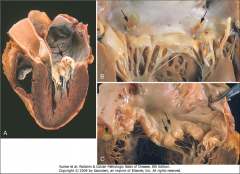
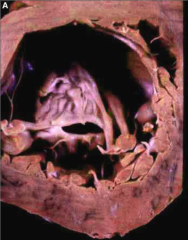
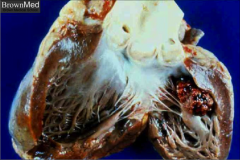
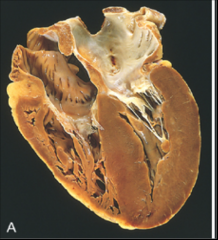
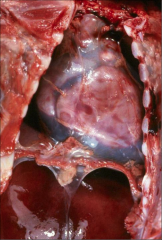
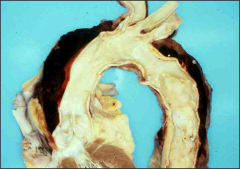
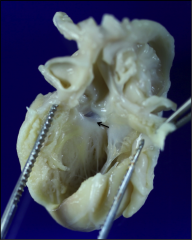
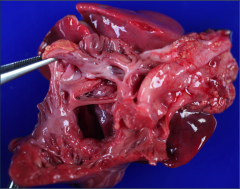
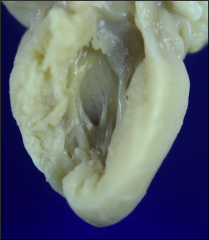
What's going on here? |
S/P MI (several days); note pallor of infarcted area (L ventricular wall).
Also note concentric hypertrophy of the left ventricle. |
|

What artery was involved here? |
L Circumflex |
|

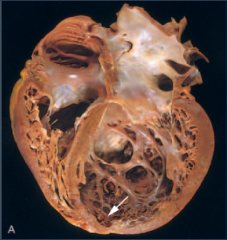
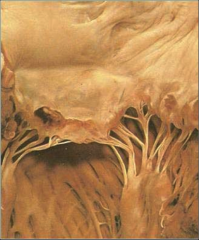
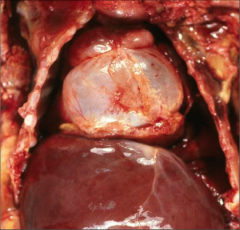
What's going on here? |
S/P MI (several days); note pallor of infarcted area (L ventricular wall), as well as other white scars indicative of prior MI.
Also note concentric hypertrophy of the L ventricle. |
|
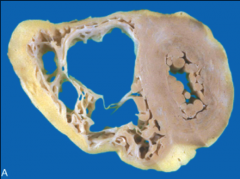
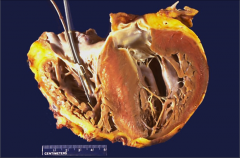
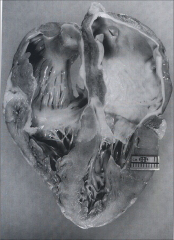
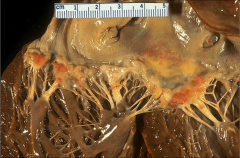
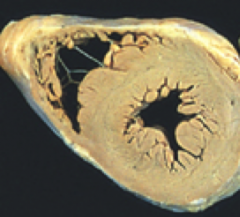
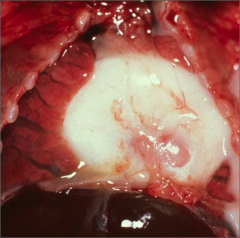
What's going on here? |
Anteroseptal MI: several days. Note white area of scarring surrounded by superficial, reddish-brown granulation tissue. |
|
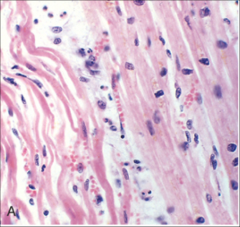
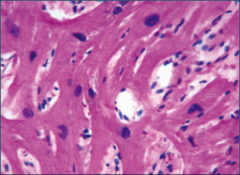
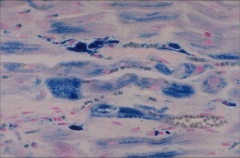
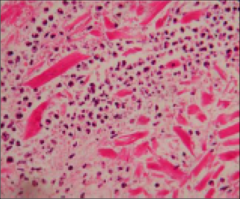
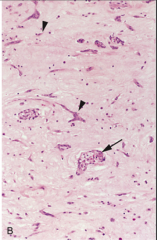
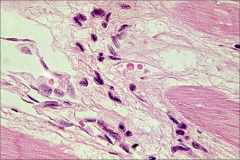
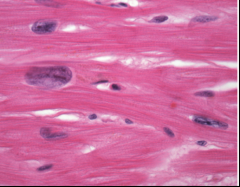
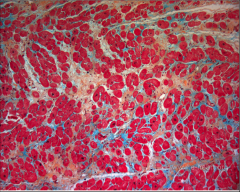
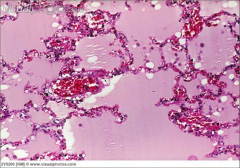
What's going on here? |
Wavy fibers - earliest pathological sign of MI |
|
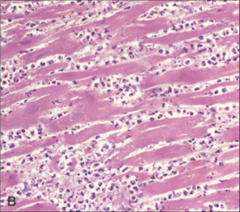
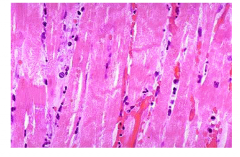
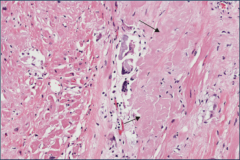
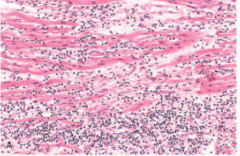
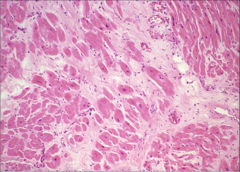
What's going on here? |
Few days s/p MI. Note disappearance of nuclei in cardiac myocytes, as well as hypereosinophilia and neutrophil infiltration |
|
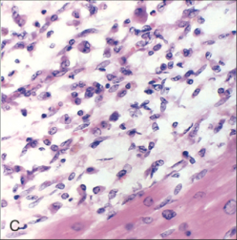
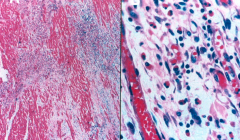
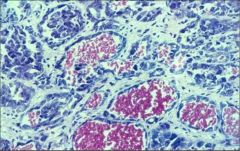
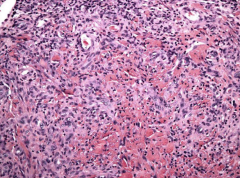
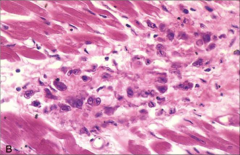
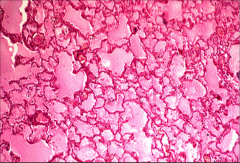
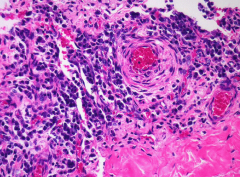
What's going on here? |
Days-weeks s/p MI: early stages of scar formation. Note macrophages infiltration and resorption of dead tissue |
|
|
When is myocardial tissue most prone to rupture s/p MI? |
3-7 days s/p MI (important fact!) |
|
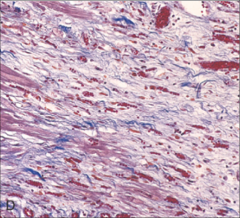
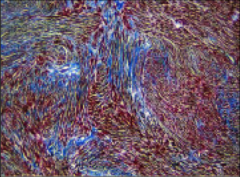
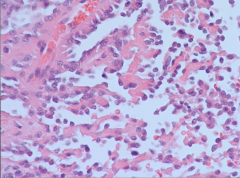
What's going on here? |
Weeks s/p MI: formation of granulation tissue. Note neovascularization (hyperemic) and deposition of collagen and other connective tissue. |
|
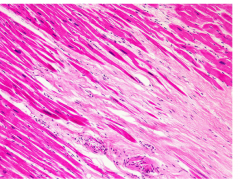
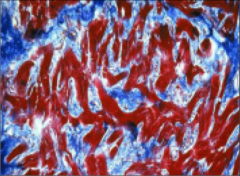
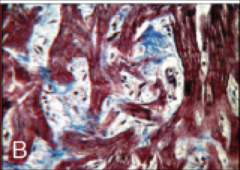
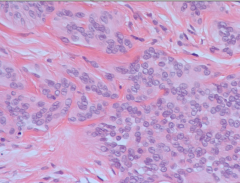
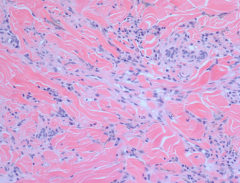
What's going on here? |
Healed MI: dense, avascular collagenous tissue |
|

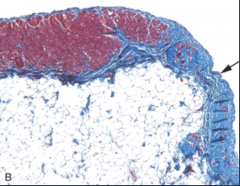
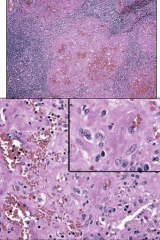
What's going on here? |
Healed MI w/trichrome stain demonstrating extensive collagen deposition |
|
What's going on here? |
Subendocardial myocytolysis |
|
What's going on here? |
Contraction bands indicative of nonviable tissue from reperfusion injury |
|
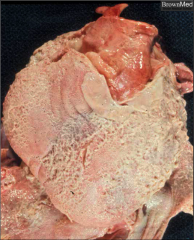
What's going on here? |
Evidence for reperfusion injury on gross pathology: note brown area of hemorrhage |
|
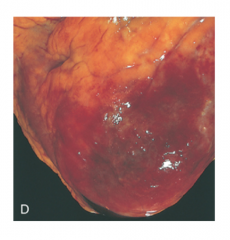
What's going on here? |
Fibrinous pericarditis; note fine, granular tissue on the surface of the heart |
|
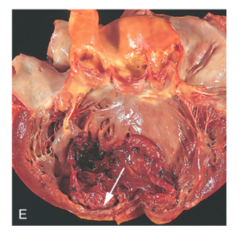
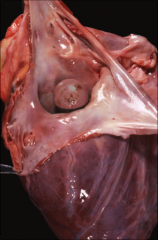
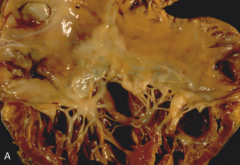
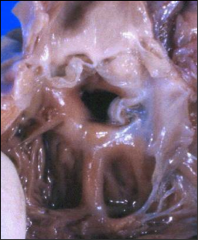
What's going on here? What are the consequences. |
Mural thrombus, usually resulting from a trasmural infarct. The ventricular surface becomes damaged and thrombogenic, leading to very dangerous systemic embolic consequences (DVT, stroke, renal thrombosis, etc.) |
|

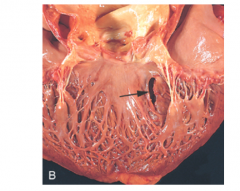
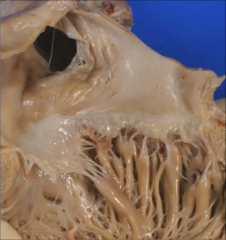
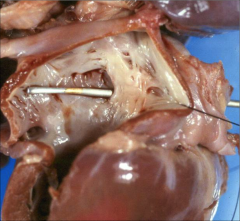
What's going on here? |
Papillary muscle rupture
|
|

What's going on here? |
Ventricular aneurysm |
|
What's going on here? |
Ventricular septal rupture |
|
What's going on here? What are the consequences? |
Anterior myocardial rupture |
|
|
Largest risk factor for sudden cardiac death |
Some form of ischemic heart disease (80-90% of cases) |
|
|
EKG changes in sudden cardiac death |
Trick question: there is no EKG or enzymatic evidence of acute MI in 80-90% of patients resuscitated from sudden cardiac death. |
|
|
Cardiac consequences of cocaine use (5) |
1. Increased myocardial oxygen demand (sympathomimetic: increase contractility/HR) 2. Vasoconstriction 3. Enhanced platelet aggregation 4. Arrhythmias 5. 24-FOLD INCREASE IN RISK OF MI |
|
|
Graft arteriopathy |
Diffuse intimal thickening of coronary arteries in a transplanted heart.
This is especially problematic because the grafted heart is denervated, and thus patient does not exhibit angina symptoms, and problem goes undetected. |
|
What's going on here? |
Graft arteriopathy - note thickening of intima |
|
|
Define a "critical" stenotic lesion |
75% area occlusion: compensatory vasodilation can no longer meet increases in demand (this is why stable angina tends to occur at this level of stenosis) |
|
|
When is return to exercise and normal activities recommended s/p STEMI? |
6-8 weeks: once fibrosis is completed and scar is properly healed |
|
|
Why do you ALWAYS call 911, even with small MI's? |
Even small MI's can lead to ventricular fibrillation. You want the defibrillator around in the ambulance; do not drive your loved ones to the hospital even if the infarct seems minor. |
|
|
Management of cardiogenic shock |
• Early reperfusion |
|
|
Ventricular septa defect (as sequelae to ischemic event): diagnosis and treatment |
Diagnosis: |
|
|
Intra-aortic balloon pump: mechanism, effects and indications |
Mechanism: balloon just fits the size of the aorta. It deflates during systole, creating a vaccuum and decreasing afterload. It inflates during diastole, increasing perfusion pressure to coronary arteries.
Effects: - Increased mean arterial pressure (inflation during diastole) - Decreases cardiac work (less afterload) - Increases cardiac output (deflation during systole) - Increases coronary blood flow
Indications: typically a temporary measure until surgery can be performed to fix defect (esp. w/mechanical complications after MI) |
|
|
Apical aneurysm formation s/p MI: Mechanism of formation, consequences and treatment |
Mechanism: LAD MI results in anterior wall/apical ischemia; Ischemia --> loss of compliance --> expansion w/o contraction --> aneurysm formation
Consequences: 1. Systolic dysfunction (poor contractioN) 2. Stasis of blood flow --> clot --> systemic thromboembolic events (DVT, stroke, renal infarct, etc.) 3. Ventricular arrhythmias
Treatment: ventricular defibrillator to prevent ventricular arrhythmia |
|
|
Which pressure-volume loops correspond to systolic and diastolic dysfunction? |
Systolic: same as decrease in contractility; top line moves down (increase in end-diastolic volume, decrease in stroke volume/ejection fraction).
Diastolic: Loss of compliance; bottom line moves up |
|
|
"Heart Failure" vs. "Congestive Heart Failure" |
Heart failure: structural/functional dysfunction that results in impaired ventricular filling or ejection.
Congestive heart failure: specifically implies a volume-overload status |
|
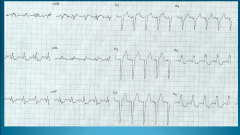
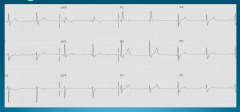
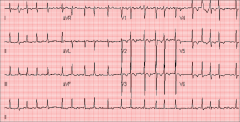
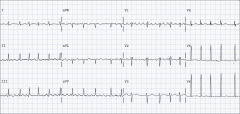
What's going on here? |
Left Bundle Branch block: note wide negative QS complex on V1; Wide, tall R wave w/o Q wave on V6 |
|
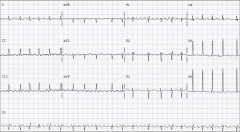
What's going on here? |
Left ventricular hypertrophy: note: • Higher voltage. Officially: V1 + V5/V6 > 35 mm (>7 big boxes or more) |
|
What's going on here? |
Prolonged PR interval: first-degree heart block |
|
What's going on here? |
Right bundle branch block; note "Rabbit ear” pattern on leads V1 |
|
|
What is the most accurate predictor for prognosis in shock? |
Lactate levels in the blood (high lactate levels directly correlate to low survival) |
|
|
Hemoglobin/hematocrit concentrations to measure blood loss |
Trick question: you can't |
|
|
Etiology of endocarditis |
By valve type: 1. Heart prostheses (prosthetic valves, pacemakers, ICD, etc.) - Mitral valve prolapse - Congenital heart defects - Degenerative valve disease (i.e. bicuspid) 3. Native valve, no prior valve disease: about 50%!
By setting of acquisition: 1. Injection drug use 2. Nosocomial acquisition: IV catheters, hemodialysis, etc. 3. Bacteremia, NOS |
|
|
Microbiologic etiology of enodcarditis |
1. Staphylococci: most common 2. Streptococci: typically viridans 3. Enteroccoci 4. Other: gram-negative, fungal, culture-negaitve
Special considerations: - Strep Gallolyticus/S. bovis: often from colonic malignancy (merits GI workup) - Enterococcus: older men/younger women w/GU manipulation - Early prosthetic valves, before they have endothelialized: less virulent, coagulase-negative strep species |
|
|
What's the most common culture-negative bacteria for endocarditis? |
A culture-positive bacteria and a history of recent antimicrobial therapy |
|
|
Pathophysiology of endocarditis |
1. STERILE (non-bacterial) vegetation formation, normally on valve 2. Transient bacteremia 3. Bacterial adherence and colonization of vegetation |
|
|
Clinical findings of endocarditis |
1. Functional and structural impairment of the cardiac valve due to vegetation/destructive processes - Significant murmur 2. Bland septic embolization to virtually any organ - Splenomegaly - Major infarcts (DVT, stroke, etc.) - Mycotic aneurysm (colonization and dilation of vessel wall) 3. Continuous bacteremia, often with metastatic foci - Fever 4. Circulating immune complexes - Clubbing - Petechiae - Splinter hemorrhages - Roth spots - Oslerian nodes (painful) - Janeway lesions (painless) |
|
|
What is the hallmark of endocarditis related to injection drug use? |
Bacterial colonization of the right heart
Clinical manifestations: - Congestive heart failure - Pleural effusions - Pulmonary emboli - Pneumonia
|
|

What's going on here? |
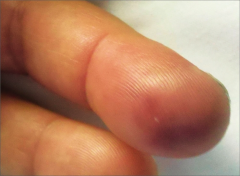
Clubbing secondary to endocarditis |
|
What's going on here? |
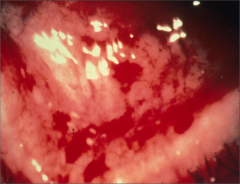
Endocarditis vegetation |
|
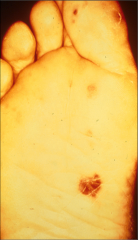
What's going on here? |
Janeway lesion secondary to S. aureus endocarditis |
|
What's going on here? |
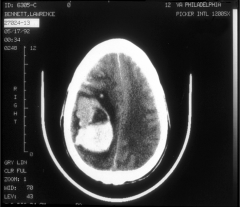
Hemorrhage due to mycotic aneurysm, secondary to endocarditis |
|
What's going on here? |
Osler node secondary to endocarditis |
|
What's going on here? |
Petechiae of the eye secondary to bacterial endocarditis |
|
What's going on here? |
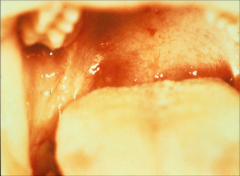
Petechiae of the palate secondary to bacterial endocarditis |
|
What's going on here? |
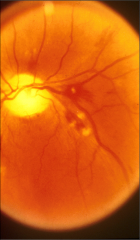
Roth spots secondary to bacterial endocarditis |
|
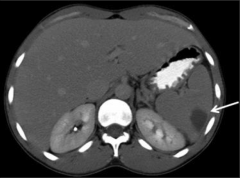
What's going on here? |
Splenic infarct secondary to bacterial endocarditis |
|

What's going on here? |
Splinter hemorrhages secondary to bacterial endocarditis |
|
|
Clinical findings unique to prosthetic valve endocarditis |
1. Congestive heart failure 2. Shock 3. Conduction abnormality |
|
|
Diagnosis of endocarditis |
1. BLOOD CULTURE
2. Electrocardiogram/echocardiogram (trans-thoracic AND trans-esophageal) to demonstrate vegetations (serum markers usually aren't particularly helpful) |
|
|
Principles of antimicrobial therapy for endocarditis (2) |
1. Bactericidal (HUGE concentrations of bacteria in vegetations with few devisions)
|
|
|
Antimicrobials for streptococcal endocarditis |
LOW MIC - Standard: 4 weeks penicillin (IV adminsitration) - Resistant: vancomycin
HIGH MIC - 4-6 weeks Penicillin + gentamycin - 4-6 weeks vancomycin |
|
|
Antimicrobials for staphylococcal endocarditis |
- 6 weeks Nafcillin + a few days of gentamicin - 6 weeks vancomycin if resistant - Rifampin addition w/prosthetic valve |
|
|
Efficacy of antibiotic therapy before dental work |
NOT proven |
|
|
Antibiotic prophylaxis for cardiac conditions |
Amoxicillin, ampicillin or ceftriaxone |
|
|
For which cardiac conditions is antibiotic prophylaxis recommended? |
- Prosthetic cardiac valve - Previous infective endocarditis - Congenital heart disease - Cardiac transplant
*** Note: even these are contentious (and not practiced in many countries!) |
|
|
For which situations is antibiotic prophylaxis against endocarditis recommended? |
1. Dental work with: - Gingival crevice - Periapical region of teeth - Perforation of oral mucosa
4. Bacterial GU infection |
|
|
What labs do you get for a second infarct (w/history of recent infarct) |
CPK - NOT troponin (troponin will still be elevated from first MI)? |
|
What's going on here? |
Arrhythmogenic right ventricular dysplasia - note fatty ventricular border |
|
What's going on here? |
Arrhythmogenic right ventricular dysplasia - note fatty ventricular border |
|
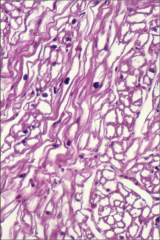
What's going on here? |
Arrhythmogenic right ventricular dysplasia - note replacement of muscle in ventricular wall with fibrotic tissue |
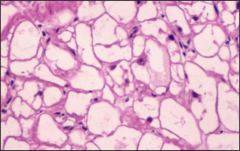
|
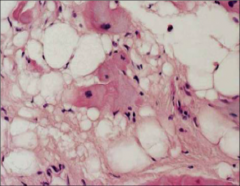
What's going on here? |
Arrhythmogenic right ventricular dysplasia - note displacement of cardiac myocytes with adipose |
|
What's going on here? |
Restrictive cardiomyopathy secondary to Pompe's disease - note glycogen deposits between cardiac myoctes |
|

What's going on here? |
Restrictive cardiomyopathy secondary to Pompe's disease - note pallor of heart on gross inspection |
|
What's going on here? |
Dilated cardiomyopathy |
|
What's going on here? |
Dilated cardiomyopathy |
|
What's going on here? |
Dilated cardiomyopathy |
|
What's going on here? |
Hypertrophic cardiomyopathy - note disarray and lateral attachments of myocytes |
|
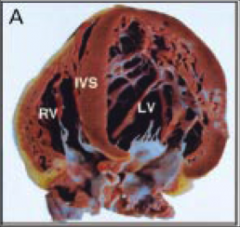
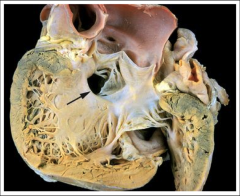
What's going on here? |
Hypertrophic cardiomyopathy - note dramatic hypertrophy of interventricular septum |
|
What's going on here? |
Hypertrophic cardiomyopathy - note slit-like appearance of ventricular cavity |
|
What's going on here? |
Hypertrophic cardiomyopathy - note disarray and lateral attachments of myocytes |
|
What's going on here? |
Hypertrophic cardiomyopathy - note disarray and lateral attachments of myocytes |
|
What's going on here? |
Hypertrophic cardiomyopathy - note disarray and lateral attachments of myocytes |
|
What's going on here? |
Hypertrophic cardiomyopathy with "flail" anterior mitral valve leaflet (that causes transient ventricular outflow obstruction) |
|
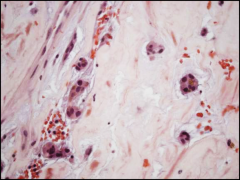
What's going on here? |
Restrictive cardiomyopathy secondary to hemochromatosis (iron stain) |
|
What's going on here? |
Restrictive cardiomyopathy - note bi-atrial dilatation |
|
What's going on here? |
Restrictive cardiomyopathy secondary to amyloid deposition (avascular area to the right of the field). |
|
What's going on here? |
Restrictive cardiomyopathy secondary to amyloid deposition (note inclusions) |
|
What's going on here? |
Isolated left ventricular non-compaction; note abnormal predominance of trabeculations |
|
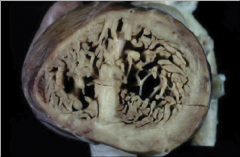
What's going on here? |
Isolated left ventricular non-compaction; note abnormal predominance of trabeculations |
|
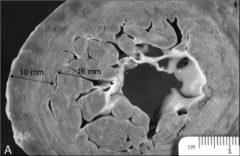
What's going on here? |
Isolated left ventricular non-compaction; note abnormal predominance of trabeculations |
|
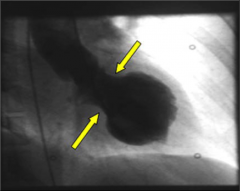
What's going on here? |
Apical ballooning typically seen with stress cardiomyopathy |
|
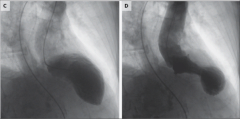
What's going on here? |
Apical ballooning typically seen with stress cardiomyopathy |
|
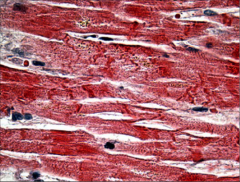
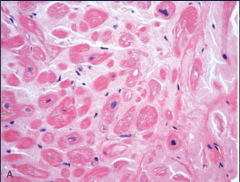
This sample was taken from a heart with no evidence of CAD. What happened? |
Contraction bands secondary to catecholamine release in stress cardiomyopathy |
|
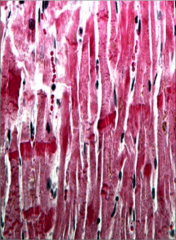
This sample was taken from a heart with no evidence of CAD. What happened? |
Contraction bands secondary to catecholamine release in stress cardiomyopathy |
|
|
Is endomyocardial biopsy an effective diagnostic tool for myocarditis? |
Not really; high chance of false-negative as myocarditis disease process can be patchy |
|
What's going on here? |
Abscess secondary to bacterial endocarditis |
|

What's going on here? |
Bacterial endocarditis |
|
What's going on here? |
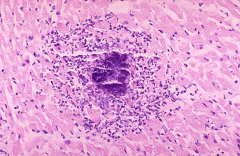
Giant cell myocarditis |
|
What's going on here? |
Giant cell myocarditis |
|
What's going on here? |
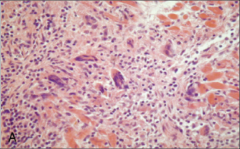
Loeffler's (eosinophilic) myocarditis |
|
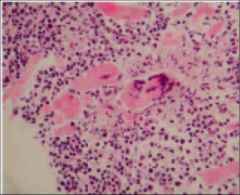
What's going on here? |
Loeffler's (eosinophilic) myocarditis |
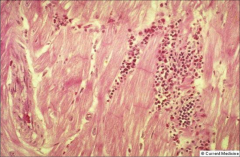
|
What's going on here? |
Loeffler's (eosinophilic) myocarditis |
|
What's going on here? |
Viral endocarditis (note predominance of monocyte infiltration) |
|
|
List ALL angiotesnsin-II effects |
1. Vasoconstriction 2. Aldosterone production 3. Myocyte hypertrophy 4. Fibroblast proliferation; collagen deposition 5. Apoptosis 6. Pro-thrombotic 6. Pro-oxidant 7. Adrenergic stimulation 8. Endothelial dysfunction |
|
|
What is ventricular modeling and how does it relate to management of cardiovascular disease? |
Ventricular remodeling refers to dilatation and hypertrophy to compensate to decreased cardiac output. It can lead to potentially fatal arrhythmias.
ACE inhibitors and beta blockers are particularly useful for preventing ventricular modeling, especially in the setting of ischemia (i.e. s/p MI) |
|
|
Best prognostic predictor of dilated cardiomyopathy |
Ejection fraction (low ejection fraction is the best predictor of sudden cardiac death) |
|
|
Indications for defibrillator placement in dilated cardiomyopathy |
1. <30% Ejection Fraction 2. 30-35% ejection fraction + heart failure |
|
|
Diagnosis of anterior mitral leaflet LV outflow obstruction in the context of hypertrophic cardiomyopathy (2) |
1. Cardiac cath "pull-back" tracing to detect drop in systolic pressure across the obstruction, just inferior to the aortic valave
2. Brockenbrough-Braunwald Sign: in a normal LV, agitation of heart muscle w/cath will produce an increased cardiac output; will not occur w/LVOO in HCM |
|
|
Best prognostic predictor of hypetrophic cardiomyopathy |
Magnitude of hypertrophy |
|
|
Physiologic vs. pathologic cardiac hypertrophy |
Thickness of ventricle never exceeds 15 mm in hypertrophy induced by endurance training |
|
What's going on here? |
Myxoma (round in appearance) |
|
What's going on here? |
Myxoma (round and gelatinous in appearance) |
|
What's going on here? |
Myxoma: myxoma cells (large multi-nucleated cels) w/mucco-polysaccharide matrix |
|
What's going on here? |
Myxoma: myxoma cells (large multi-nucleated cels) w/mucco-polysaccharide matrix |
|

What's going on here? |
Myxoma (round and gelatinous in appearance) |
|
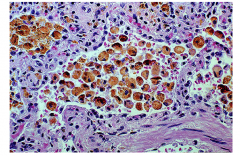
What's going on here? |
Rhabdomyoma - note polygonal cells with glygogen-rich vacuoles; "spider cells" |
|

What's going on here? |
Rhabdomyoma (in cut section of ventricle): note bland, grey-white appearance |
|

|
Angiosarcoma - dark and scary-looking in appearance |
|
|
Angiosarcoma: note bizarre/inappropriate epithelial cells |
|
|
Angiosarcoma: note bizarre/inappropriate epithelial cells |
|
|
Angiosarcoma: note bizarre/inappropriate epithelial cells |
|
|
Bacillary angiomatosis: note prolfierative capillaries and atypicalendothelial cells |
|

|
Bacillary angiomatosis (cherry papule) |
|

|
Kaposi sarcoma (early stages - looks like granulation tissue) |
|
|
Kaposi sarcoma - plump spindle cells with slit-like vascular spaces |
|
|
Kaposi sarcoma - plump spindle cells with slit-like vascular spaces |
|
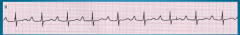
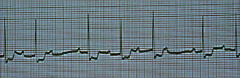
What's going on here (in terms of rate & rhythm)? |
Rate: 50 BPM (bradycardia)
Rhythm: - Regular - Narrow QRS - Absent P-waves
--> Impulse must be generated somewhere above the ventricles (narrow QRS) but belot he atria (absent P-waves)
--> Junctional escape (Rhythm comes from top of His-purkinje system |
|
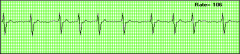
What's going on here (in terms of rate & rhythm)? |
Rate: 60 BPM (bradycardia)
Rhythm: - Regular - Narrow QRS - Present, uniform P-wave
--> Sinus bradycardia |
|
|
Re-entry tachycardia (definition) |
Circuit created within atrium (SA --> AV --> SA node) that produces tachycardia |
|

What's going on here (in terms of rate & rhythm)? |
Rate: 160
Rhythm: - Regular - Narrow QRS - P-waves are unusual/difficult to discern
--> Supraventricular tachycardia |
|
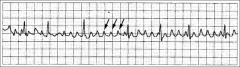
What's going on here (in terms of rate & rhythm)? |
Rate: atrial rate is VERY fast (about 300); QRS complex rate looks more normal.
Rhythm: - Regular - Flutter waves: sharp, saw-tooth baseline P-waves that can be traced through QRS complex - Narrow QRS complex
--> atrial flutter |
|
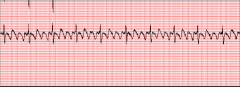
What's going on here (in terms of rate & rhythm)? |
Rate: Irregular Irregular
Rhythm: "Fibrillation" p-waves (just look like squiggly noise)
--> Atrial fibrillation |
|
What's going on here (in terms of rate & rhythm)? |
Rate: Irregular irregular
Rhythm: "Fibrillation" p-waves (just look like squiggly noise)
--> Atrial fibrillation |
|

What's going on here (in terms of rate & rhythm)? |
Rate: 75 BPM
Rhythm: - Regular - Narrow QRS - Absent P-waves
--> Impulse must be generated somewhere above the ventricles (narrow QRS) but belot he atria (absent P-waves)
--> Junctional tachycardia (Rhythm comes from top of His-purkinje system; normal for sinus rhythm but fast for junctional escape rhythm!) |
|
What's going on here (in terms of rate & rhythm)? |
Rate: 75 BPM
Rhythm: - Regular QRS - Narrow QRS - Normal P waves with the EXCEPTION of a premature atrial contraction w/compensatory pause
--> Premature atrial contraction |
|

What's going on here (in terms of rate & rhythm)? |
Rate: 70 BPM
Rhythm: - Wide QRS - Full compensatory pause
--> Premature ventricular contraction |
|
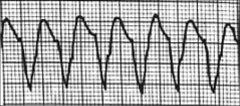
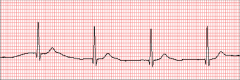
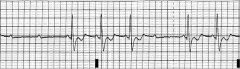
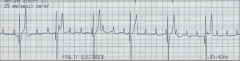
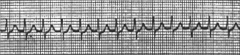
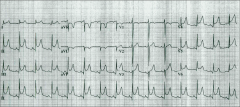
What's going on here (in terms of rate & rhythm)? |
Rate: 100 BPM
Rhythm: - Regular - Wide, strange QRS
--> Ventricular tachycardia |
|
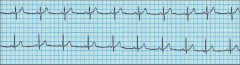
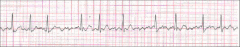
What's going on here (in terms of rate & rhythm)? |
Rate: 110 BPM
Rhythm: - Regular - Wide, strange QRS
--> Ventricular tachycardia |
|
|
You look at an EKG and you suspect (but can't confirm) that it is ventricular tachycardia. What elements of the patient's history would corroborate your suspicion? |
Prior MI for which there was NO tachycardia leading up to the event. |
|
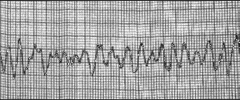
What's going on here (in terms of rate & rhythm)? |
Rate: Regular irregular
Rhythm: Irregular, wide QRS complex with no discernable structure
--> ventricular fibrillation |
|
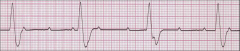
What's going on here (in terms of rate & rhythm)? |
Rate: 60 BPM
Rhythm: - Narrow QRS - Present, uniform p-waves - Prolonged PR interval (longer than one box or 0.2 seconds)
--> first-degree AV block |
|
|
List the irregular rhythms on EKG. Which one of these are irregular irregular? |
1. Premature atrial/ventricular contraction 2. Multifocal atrial tachycardia 3. Atrial fibrillation: ONLY irregular/irregular rhythm 4. Ventricular fibrillation 5. Second-degree AV block |
|
What's going on here (in terms of rate & rhythm)? |
Rate: regular irregular
Rhythm: - Prolonged pr interval - Progressive lengthening of PR interval until QRS beat is dropped (two p-waves in the low) - Narrow QRS complex
--> Mobitz 1/Wenckebach second-degree AV block |
|
What's going on here (in terms of rate & rhythm)? |
Rate: regular irregular
Rhythm: - Prolonged PR interval - Randomly dropped QRS beats with NO progressive lengthening of PR interval - Narrow QRS complex
--> Mobitz 1/Wenckebach second-degree AV block |
|
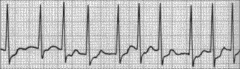
What's going on here (in terms of rate & rhythm)? |
Rate: 75
Rhythm: - Narrow - Present, regular P-waves
--> normal sinus rhythm
|
|
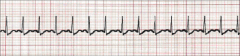
What's going on here (in terms of rate & rhythm)? |
Rate: 150
Rhythm: - Narrow QRS - Present, uniform P-waves
--> Sinus tachycardia |
|
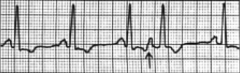
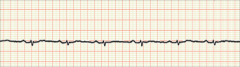
What's going on here (in terms of rate & rhythm)? |
Rate: 50
Rhythm: - P and QRS waves occur independently of each other - Wide QRS complex - Rhythm is regular
→ third degree AV block (complete absence of conduction through AV node) |
|
What's going on here (in terms of rate & rhythm)? |
Rate: Irregular Irregular
Rhythm: "Fibrillation" p-waves (just look like squiggly noise)
--> Atrial fibrillation |
|
What's going on here (in terms of rate & rhythm)? |
Rate: 75
Rhythm: - Normal QRS and p-waves, except: - Early, wide QRS complex w/complete compensatory pause - Present, uniform P-waves (except before premature QRS complexes)
--> Premature ventricular contraction (PVC) |
|
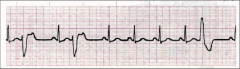
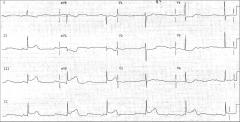
What's going on here (in terms of rate & rhythm)? |
Rate: 125
Rhythm: - Regular - No P-waves - Wide QRS complex
--> Ventricular tachycardia |
|
What's going on here (in terms of rate & rhythm)? |
Rate: irregular (but fast)
Rhythm: - No P-waves - Wide and erradic QRS complex
--> Ventricular fibrillation |
|
What's going on here (in terms of rate & rhythm)? |
Rate: 100 BPM
Rhythm: - Narrow QRS - No P-waves
--> Junctional escape tachycardia |
|
What's going on here (in terms of rate & rhythm)? |
Rate: 35 - Regular - Present, uniform P-waves that are not always followed by QRS - Wide QRS
--> Third-degree AV block |
|
What's going on here (in terms of rate & rhythm)? |
Rate: Irregular Irregular
Rhythm: "Fibrillation" p-waves (just look like squiggly noise)
--> Atrial fibrillation |
|

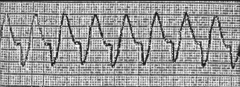
What's going on here (in terms of rate & rhythm)? |
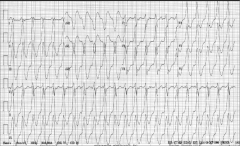
Rate: fast (around 200 BPM)
Rhythm: - Regular - P-waves absent - Wide QRS
--> Ventricular tachycardia |
|
|
Is the loudness of a murmur useful in predicting the extent of valve stenosis? |
Nope |
|
|
Is the peak timing of a crescendo-decrescendo of a murmur useful in predicting the extent of valve pathology? |
Yep - mid-late peaking is a bad prognostic predictor |
|
|
What morphological changes might you see with a bicuspid aortic valve? (4) |
1. Aortic valve stenosis 2. Aortic regurgitation 3. Aortic root dilation/aneurysm 4. Aortic coarctation |
|
|
Parvus et tardus |
Slow-rising carotid upstrokes: indicative of severe aortic stenosis |
|
|
Significance of widened pulse pressure |
Finding typical in aortic regurgitation: - Systolic BP is high (compensatory raised cardiac output0 - Diastolic BP is low (leakage of blood back into the atrium) |
|
|
Patient presents with rapid respirations (40/min) and low blood pressure that is precipitously falling.
Exam: - JVD - Tachycardia - Wide S2 splitting but otherwise normal heart sounds - Normal temperature - Clear lungs
What is your treatment plan? (1) Give fluids (2) Give diuretics (3) Give inotropes |
Give fluids - this sounds like R heart failure |
|
|
How does your treatment plan differ for L and pure R heart failure? |
L heart failure: Reduce preload (give duiretics)
R heart failure: increase preload (give fluids) |
|
|
Define dystrophic calcification |
Deposition of calcium in a tissue that has already been damaged by some other process |
|
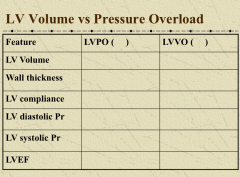
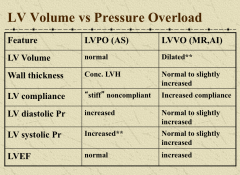
Compare and contrast three valvulopathies |
|
|

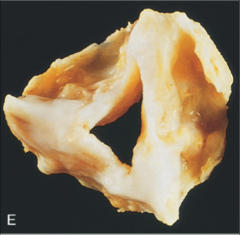
What's going on here? |
Tricuspid (normal) aortic valve with calcification and fibrosis ("stiffness") of valve leaflets |
|
What's going on here? |
Bicuspid aortic valve with calcification and thrombosis. Note “median raphe” (area of fibrous tissue); represents embryologic remnant of attempt at tricuspid valve |
|
|
Consequences of mitral annular calcification |
1. Often none (very common finding in elderly 2. Can cause mitral regurgitation or mitral insufficiency |
|
What's going on here? |
Mitral annular calcification |
|

What's going on here? |
Mitral annular calcification |
|
|
Mutation in Marfan's Syndrome? |
Fibrillin gene |
|

What's going on here? |
Mitral prolapse: note thin, elongated cordae tendinae and thickening/hooding of leaflets |
|
What's going on here? |
Mitral prolapse: note mucopolysaccharide material |
|
What's going on here? |
Myxomatous degeneration of the mitral valve secondary to mitral prolapse; note accumulation of mucopolysaccharides |
|
What's going on here? |
Mitral prolapse: note temendously dilated left atrium, thin, elongated cordae tendinae and thickening/hooding of leaflets |
|
|
Aschoff body with Anitschkow cells (bizarre macrophages w/chromatin in dense “ribbon resembling catepillar”). Associated with rheumatic heart disease. |
|
|
Aschoff body with Anitschkow cells (bizarre macrophages w/chromatin in dense “ribbon resembling catepillar”). Associated with rheumatic heart disease. |
|
What's going on here? |
Acute rhuematic endocarditis; note verucae |
|

What's going on here? |
Acute rhuematic endocarditis; note verucae |
|
What's going on here? |
"Fishmouth valve" - characteristic of mitral stenosis |
|
What's going on here? |
Aortic stenosis with comissural fusion |
|
What's going on here? |
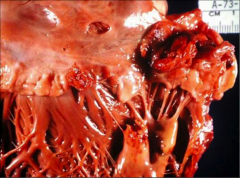
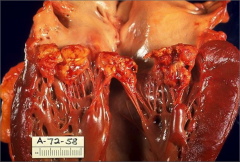
Acute Bacterial Endocarditis with large vegetation |
|
What's going on here? |
Acute bacterial endocarditis with valvular abscess formation |
|
What's going on here? |
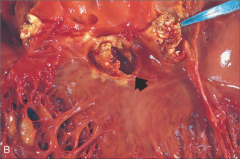
Bacterial endocarditis w/vegetations |
|
What's going on here? |
Bacterial endocarditis affecting valve |
|

What's going on here? |
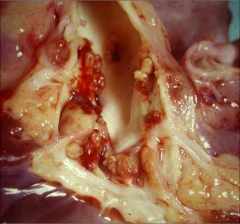
Bacterial endocarditis (tons of blue deposits) |
|
What's going on here? |
Endocarditis due to Candida |
|
|
Complications of bacterial endocarditis (5) |
1. Valvulopathies 2. Suppurative pericarditis 3. Emboli 4. Glomerulonephritis (antigen-antibody complexes) 5. Nonbacterial thrombotic endocarditis: in debilitated or hypercoagulable states, bland thrombi can form on lien of valve closure and are very prone to embolization |
|

What's going on here? |
Nonbacterial Thrombotic Endocarditis - note formation of bland thrombi along the line of closure of the valve |
|
What's going on here? |
Nonbacterial Thrombotic Endocarditis - note formation of bland thrombi along the line of closure of the valve |
|
|
Etiology of Libman-Sacks Endocarditis |
Lupus |
|
What's going on here? |
Libman-Sacks Endocarditis |
|
|
Carcinoid tumor |
GI tumor that produces serotonin; serotonin exposure causes fibrous plaque-like endocardial thickening on chambers/valves of RIGHT heart |
|
What's going on here? |
Consequence of serotonin exposure secondary to carcinoid tumor; note plaque-like thickening of right heart |
|
|
When does JVD occur in heart failure? |
Pure R-sided heart failure: early finding L-sided-induced right heart failure: late finding
|
|
|
Core pulmonal |
R heart failure secondary to parenchymal lung disease (COPD/interstitial lung disease) |
|

What's going on here? |
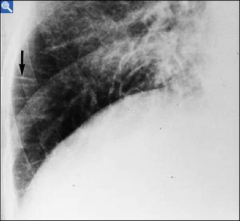
Kerley B-lines indicative of interstitial edema |
|
What's going on here? |
Kerley B-lines indicative of interstitial edema |
|
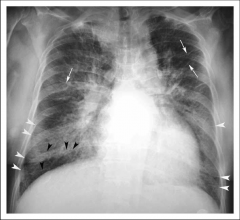
What's going on here? |
Kerley B-lines (white arrowheads) indicative of interstitial edema |
|
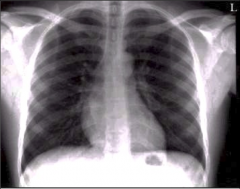
What's going on here? |
Normal chest X-ray |
|

What's going on here? |
Pleural effusion; note blunting of the "costo-phrenic" angle (the angle normally seen between the diaphragm and the chest wall) |
|

What's going on here? |
Pulmonary edema: note "fluffy infiltrates" |
|
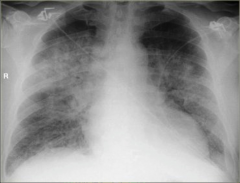
What's going on here? |
Pulmonary edema: note "fluffy infiltrates" |
|

What's going on here? |
Early pulmonary edema secondary to heart failure: note redistribution of pulmonary vasculature and prominence of cardiac silhouette (>1/2 chest diameter) |
|
|
Describe, on a cellular level, the process of cardiac hypertrophy |
- Hypertrophy: cells enlarge (NOT hyperplasia; cells stop dividing after birth) - Enlargement of nuclei - Increase in number of sarcomeres - Sarcomere becomes larger (width > length in concentric hypertrophy, length > width in eccentric and physiologic hypertrophy) - Recapitulation of fetal metabolism (glycolysis) - Altered calcium homeostasis - Remodeling: reorganization of sarcomeres, electric remodeling - Myocyte death and fibrosis |
|
|
Meaning of word "decompensated" in the context of heart failure |
Defect has gotten severe enough that compensatory mechanisms for heart failure can no longer preserve cardiac output |
|

What's going on here? |
Cardiomegaly |
|

What's going on here? |
Concentric hypertrophy |
|
What's going on here? |
Eccentric hypertrophy |
|
What's going on here? |
LV concentric hypertrophy |
|
What's going on here? |
Normal heart |
|
|
Molecular mechanism for hypertrophy |
1. Mechanical stimulation (i.e. stretching) of myoctyes --> activation of integrins 2. Integrins promote expression of ligand growth factors (along with other neuro-hormonal agonists: angiotensin II, NE, ect.) 3. Ligands bind and initiate signaling cascades that induce transcription of fetal proteins, growth factors and contractile machinery (with an autocrine mechanism of growth ligand/factor interaction as well!) |
|
|
Cellular mechanism of regression of hypertrophy after intervention |
- Suppression of pro-growth pathways - Activation of protein degradation proteins, including proteosome/ubiquitin system |
|
|
Most common site of thrombus generation in the heart |
Left atrial appendage |
|
What's going on here? |
Hypertrophic myocardium |
|
What's going on here? |
Hypertrophic myocardium w/interstitial fibrosis (demonstrated by trichrome stain) |
|
What's going on here? |
Hypertrophic myocardium w/interstitial fibrosis |
|
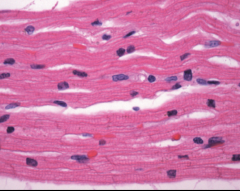
What's going on here? |
Normal myocardium |
|
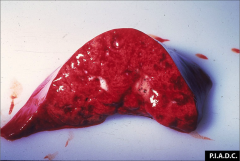
What's going on here? |
Pulmonary edema: note glossy appearance and presence of "bubbly" fluid |
|
What's going on here? |
Pulmonary edema with extravasation of RBCs |
|
What's going on here? |
Pulmonary edema |
|
What's going on here? |
Lung heart failure cells |
|
|
Structure of cardiac ion channels? |
Na/K channels: single, long polypeptide chain with 4 homologous domians, each with 6 transmembrane segemnts.
Calcium channels; simple conglomerate of 4 subunits |
|
|
Most important connexon |
Cx43 |
|
|
Electrophysical principle of defibrillation |
Maximally depolarize every cell --> put every cell into refractory period --> halts aberrant rhythm |
|
|
What is the physiologic mechanism for slow conduction through the AV node? |
The Ca2+-mediated upstroke is slow, and therefore conduction velocity through t he nodal tissue is slower.
Additionally, as the rate of stimulation increases, the length of the refractory period also becomes longer.
These parameters are of coursed influence by sympathetic/parasympathetic tone. |
|
|
EKG changes seen w/exercise |
Shortened PR interval (increased HR --> less time in diastole) |
|
|
What is the mechanism for catecholamine influence on the SA node? |
Catecholamines increase the slope of (and therefore shorten) phase 4 depolarization. The increased slope allows threshold to be reached sooner |
|
|
Most common class of clinical arrhythmias |
Reentrant tachycardia |
|
|
Calculate the LDL for the following panels. Is this a normal LDL?
1. TC 193, TG 275, HDL 35
2. TC 324, TG 135, HDL 46
3. TC 248, TG 855, HDL 30
|
1. LDL = 103
2. LDL = 251 High LDL
3. TG too high to calculate |
|
|
TC 208, TG 100, HDL 82: LDL 106
What's the diagnosis? |
Normal lipid panel (i.e. no elevated risk for CV disease); though TC is a little high, HDL is more than generous |
|
|
TC 193, TG 275, HDL 35: LDL 103
What's the diagnosis? |
High TG, slightly high LDL/HDL ratio
Diagnosis= dyslipidemia
|
|
|
TC 324, TG 135, HDL 46: LDL 251
Diagnosis? |
Familial hypercholesterolemia |
|
|
TC 248, TG 855, HDL 30: LDL ???
Differential diagnosis? |
Differential: - Remnant receptor disease - Familial hypertriglyceridemia - Undiagnosed and uncontrolled diabetes |
|
|
TC 203, TG 110, HDL 40: LDL 141
Differential diagnosis? |
Diet/polygenic hypercholesterolemia |
|
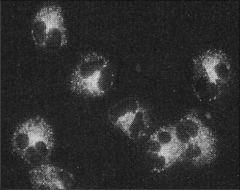
What's going on here? |
c-ANCA: cytoplasmic-staining antibodies against neutrophils, seen in some vasculitis |
|
What's going on here? |
p-ANCA: perinuclear-staining antibodies against neutrophils, seen in some vasculitis |
|

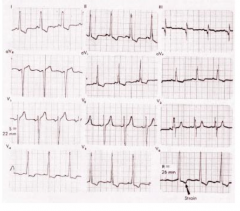
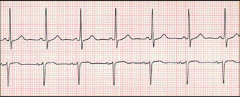
What's going on here? |

Autonomic atrial tachycardia (abnormal automticity tachyarrhythmia): note shift in p-waves, indicating an aectopic atrial pacemaker. Also note "warm-up" sequence preceding onset of tachcyardia. |
|
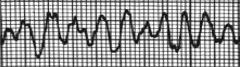
What's going on here? |
torsades de pointes |
|
What's going on here? |
Atrial flutter - note muliple, repeating, tachycardic p-waves without coupling to QRS complex, and narrow QRS complex |
|
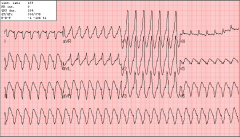
What's going on here? |
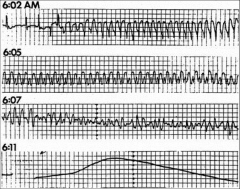
Suddenc cardiac death; progression from ventricular tachycardia to ventricular fibrillation to asystole. |
|
What's going on here? |
Wide complex tachycardia. Note wide QRS waves and regular, tachycardic rate (>100bpm). Also note that the p-waves are absent or decoupled from the QRS complexes |
|

What's going on here? |
Tendinous xanthoma due to pure hypercholesterolemia syndrome |
|
What's going on here? |
Eruptive xanthoma due to hypercholesterolemia syndrome, usually in conjunction with other metabolic disorders |
|

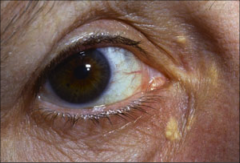
What's going on here? |
Arcus cornelius - cholesterol deposits in eyes, indicative of hypercholesterolemia |
|
What's going on here? |
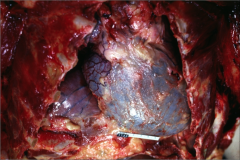
Hemopericardium; note globular blue-red appearance of pericardium (has not been removed) |
|
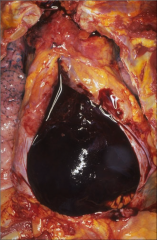
What's going on here? |
Hemopericardium; pericardim has been removed to reveal giant blood clot |
|
What's going on here? |
Hemopericardium; note globular blue-red appearance of pericardium (has not been removed) |
|
What's going on here? |
Pneumopericardium (distended pericardial sac) |
|
What's going on here? |
Pericardial effusion due to inappropriate TPN catheter placement |
|

What's going on here? |
Fibrinous pericarditis; note "shaggy" "bread and butter" appearance of pericardium. |
|
What's going on here? |
Fibrinous pericarditis; note "shaggy" "bread and butter" appearance of pericardium. |
|

What's going on here? |
Suppurative peridcarditis |
|

This is the heart from a 45 YO TB+ man. What happened? |
Caseous pericarditis |
|
|
Congenital abnormalities affecting the pericardium? |
Congenital absence of pericardium; rare reports of strangulation herniation or association with other disorders, but rarely has clinical consequences |
|
What's going on here? |
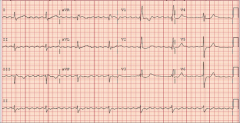
Pericarditis EKG; note ST elevation with "smiley face" pattern between ST elevation & QRS (and ST elevation covering all leads but AVR, as well as absence of reciprocal ST depression). Also note PR segment depression. |
|
|
Is pericardiocentesis used for diagnoistic purposes? |
Nope; just to treat cardiac tamponade |
|
|
How do you discern pulsus paradoxus? |
With blood pressure cuff: record pressure at which SOME systolic heart sounds are heard and ALL erradic heart sounds are heard. A difference between these points of >10 mm Hg is indicative of pericarditis. |
|
What's going on here? |
Cardiac tamponade; note electrical alternans |
|
|
Thromboangiitis obliterans |
Necrosis of fingers in smokers; caused by inflammation and thromboses in medium/small arteries, with a predilection for radial and tibial arteries. |
|
|
Rx for thromboangiitis obliterans? |
QUIT SMOKING; lesions will spontaneously resolve. |
|
|
True vs false aneruysms |
True: all 3 layers of vessel are compromised False: hematoma w/hole in vessel |
|
|
Risk of aneursym |
1. RuptureE 2. Thrombosis (turbulent flow) |
|
|
Etiology of aneurysm |
1. Acquired (atherosclerosis - most common); thins media 2. Congenital (genetic CT disease) |
|
|
Why do you worry about the location of a AAA? |
Infrarenal: won't compromise blood flow or throw clot to kidneys |
|
|
Berry aneursyms |
Small aneurysms at the circle of Willis. Often congenital CT disorders, including Marfan. Risk of rupture. |
|
|
Syphillic Aortitis |
Vasculitis that affects the vaso vasorum of aorta seen in tertiary syphillis. |
|
|
Aortic dissection |
Blood enters defective media through tear in intima; typically secondary to hypertension or congenital disease. Splits media into two layers. |
|
|
Microscopic changes that predespose the aorta to dissection |
Fragmentation of elastic tissue; pronounced "hole" (cyst?) in elastic stain. |
|
|
Complications of aortic dissection |
1. Rupture 2. Creation of another communicating channel (distal and proximal communication w/lumen) 3. Aortic regurg 4. Cardiac tapmonade |
|

What's going on here? |
Aortic dissection |
|
What's going on here? |
Aortic dissection |
|
What's going on here? |
Churg-Strauss syndrome: note eosinophils |
|
What's going on here? |
Cystic medial degeneration, predisposing lesion to aortic dissection |
|
What's going on here? |
Cystic medial degeneration, predisposing lesion to aortic dissection |
|
What's going on here? |
Giant cell arteritis; note giant cells, obliteration of elastic lamina and distended/hardened temporal artery |
|

What's going on here? |
Iliac artery dissection |
|
What's going on here? |
Polyarteritis nodosa; note partial (not circumfrencial) destruction of vessel |
|
What's going on here? |
Takayasu arteritis; note primary inflammation of the adventitia |
|

What's going on here? |
Thromboangiitis obliterans |
|

What's going on here? |
Wegner's granulomatosis; note large, nodular lesions on lung |
|
What's going on here? |
Wegner's granulomatosis; note both intravascular and perivascular granulomas |
|
|
Venodilators vs. vasodilators |
Venodilators (i.e. nitroglycerin): decrease preload Vasodilators: decrase afterload |
|
What's going on here? |
Membranous VSD (right under valves) |
|
What's going on here? |
ASD |
|
What's going on here? |
AV canal defect |
|
What's going on here? |
AV canal defect |
|
What's going on here? |
Membranous VSD (right under aortic valve) |
|
What's going on here? |
Membranous VSD (right under valves) |
|
What's going on here? |
Muscular VSD |
|
What's going on here? |
Patent foramen ovale (not visible w/o probe) |
|
|
Pediatric arrhythmias |
Usually SVT: treat in utero (direct intra-utero or through mother, but often involves administration of near-toxic doses of antiarrhythmic to reach effective dose for fetus) |
|
|
Best prognostic predictors of hypertrophic cardiomyopathy? |
(1) Family history |
|
|
Relationships between aging and diastolic heart failure |
Pure aging will cause thickening, stiffening and loss of compliance in the LV. However, pure aging is not enough in itself to produce heart failure. Diastolic heart failure will only occur when pure aging is superimposed on another disease process (i.e. hypertension). |
|
|
Cardiovascular changes associated with pure aging |
1. Cellular changes: decrease in myocyte number, increase in myocyte size. Increase in fibrocyte number.
2. Increased LV thickness and stiffness. This leads to less passive diastolic filling and more reliance on atrial contraction.
3. Incresed systmeic vascular resistance
4. Dilated L atrium, increased prevalence of afib
5. Less maximum heart rate, cardiac output and max O2 saturation
6. Less vasodilation with exercise (and even occasionally, paradoxical vasoconstriction with exercise) |
|
|
How is afib different in aging? |
Thickened, stiffened LV --> less passive diastolic filling --> more reliance on atrial kick --> more symptoms w/afib |
|
|
How is tachycardia different in aging? |
Thickened, stiffened LV --> less passive diastolic filling --> time in diastole is more important --> less tolerance of fast HR (rates <110 will produce symptoms of low cardiac output) |
|
|
Cellular changes in vasculature with pure aging |
Changes that lead to increased PVR & HTN:
2. Calcification of media, increase in vessel diameter/thickness with shrinkage of lumen
3. Decrease in endothelial function and NO production |
|
|
(Fun fact) what is the #1 risk factor for stroke? |
HTN! |
|
|
Clinical manifestations of CV changes associated with pure aging? |
1. Fatigue (decreased cardiovascular reserve)
2. High BP (increase in SVR)
3. Syncope - Blunted baroreceptor reflex - Autonomic dysfunction - Sinus node dysfunciton
4. Increased risk of thrombosis (increase in clotting factors)
5. Aortic stenosis (valvular sclerosis and calcification) |
|
|
Treatment of HTN in >80 YOs? |
Controversial; current theory is that HTN treatment (beta-blockers, diuretics, etc.) is therapeutic in active individuals |
|
|
At what stage does diastolic dysfunction become a positive predictor for five-year mortality? |
Even mild, NON-SYMPTOMATIC diastolic dysfunction involves a decreased mortality (take home: do not wait until symptoms manifest to treat). |
|
|
What are the risks of using diuretics in older age? |
Diuresis --> reduction in preload, superimposed on diastolic dysfunction of pure aging --> reduced cardiac output --> organ hypoperfusion --> kidney failure --> increased creatinine |
|
|
Do you use anti-coagulative therapies for afib in individuals >80YO? |
Yes, yes a thousand times yes. Risk of thombus w/afib is MUCH higher than risk of bleed w/anticoagulation. |
|
|
Physiologically, what does ST elevation and ST depression indicate? |
ST elevation: transmural ischemia; secondary to pericarditis, STEMI, or vasospasm of the coronary artery
ST depression: subendocardial ischemica, typically due to angina |
|
|
58 YO women presents with sudden onset severe chest pain that radiates to the back and neck. Her BP is 70 systolic, and her EKG demonstrates ST elevation in V2-V5. A prominent cardiac silhouette is seen on chest Xray. What's going on? |
Aortic dissection w/dissection flap occlusion of the L main coronary artery |
|
|
What is the most common cause of aortic dissection? |
Cystic medial degeneration (can be secondary to or independent of Marfan's syndrome) |
|
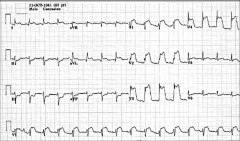
What's going on here? |
Atrial flutter |
|
What's going on here? |
Atrial flutter |
|
What's going on here? |
Atrial flutter |
|

What's going on here? |
Atrial flutter with 2:1 ventricular conduction |
|
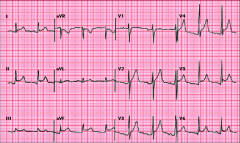
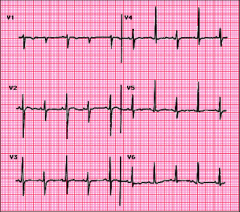
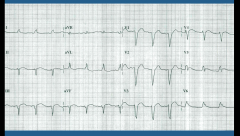
What's going on here? |
LAD and diagonal infarction |
|
What's going on here? |
Pericarditis |
|
What's going on here? |
Third-degree AV block |
|
What's going on here? |
LBBB (can't diagnose MI until catheterization) |
|
What's going on here? |
Perivascular cuffing seen in syphilic aortitis |
|
|
Levine's sing |
Closed fist over chest: often used to describe angina sensation |

