![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
165 Cards in this Set
- Front
- Back
|
appropriate resp rate for hosp pt at rest, before handling |
< 40 breaths per minute |
|
|
cardiac cachexia |
loss of lean muscle mass, most notable along topline and temporals |
|
|
ascites |
accumulation of fluid (transudate) in peritoneal cavity - indicates R sided heart failure - severe ascites can cause dyspnea and inappetance |
|
|
normal mucous membranes |
CRT <2s pink moist |
|
|
prolonged CRT |
non-specific finding, but may indicate poor cardiac output |
|
|
abnormal central mucous membranes |
may be pale, injected, cyanotic
indicates global deoxygenation of blood, VQ mismatch - ER, life-threatening
most evident in oral mm |
|
|
abnormal peripheral mucous membranes |
localized decrease in oxygenated hemoglobin may indicate thromboembolism, vasconstriction most evident in foot pads or nail beds of affected limbs |
|
|
jugular pulses |
should not be normally distended distension indicates elevated venous pressures due to R sided heart failure |
|
|
ddx for systolic murmurs |
- mitral regurgitation - tricuspid regurgitation - subaortic stenosis - pulmonic stenosis - ventricular septal defect |
|
|
murmur resulting from mitral regurg |
PMI on L, 4-6th ICS common in older, small breed dogs |
|
|
murmur resulting from tricuspid regurg |
PMI on R, 3-5th ICS common in labs |
|
|
murmur resulting from subaortic stenosis |
PMI on L heart base or R cranial may be seen in conjunction w/ weak femoral pulses common in Boxers, Golden Retrievers, Newfies |
|
|
murmurs resulting from pulmonic stenosis |
PMI on L heart base normal femoral pulses common in pitbulls, labs |
|
|
murmur resulting from ventricular septal defects |
PMI R thorax (commonly) and L 5-6th ICS (less commonly) |
|
|
ddx for diastolic murmurs |
aortic insufficiency - most commonly from endocarditis pulmonic insufficiency- rarely audible |
|
|
ddx for continuous murmurs |
patent ductus arteriosus - loudest at cranial thorax, in conjunction w/ bounding pulses
|
|
|
Non-cardiac causes of murmurs |
physiologic murmurs in dogs <6 mos old
R ventricular outflow obstructions in older cats - normal finding
r/o anemia, hypertension, pregnancy, hyperthyroidism, fever |
|
|
bradyarrhythmia |
abnormally slow |
|
|
tachyarrhythmia |
abnormally fast |
|
|
2nd degree AV block in puppies and horses |
- induced by high vagal tone - arrhythmia should disappear with exercise |
|
|
respiratory sinus arrhythmia in dogs and horses |
HR increases w/ inhalation, slows down w/ exhalation "regularly irregular" normal finding in dogs and horses, very rare in cats - recommend ECG for abnormal rhythms ausculted in cats |
|
|
gallop rhythm |
S3 - ventricular filling S4 - atrial systole suggests myocardial failure - dogs: DCM, mitral valve disease, PDA - cats: HCM or restrictive cardiomyopathy |
|
|
systolic click |
can be heart in mid to late systole
due to prolapse of mitral valve, tensing of redundant leaflets, or elongated chordae tendinae |
|
|
crackles in lungs |
fluid filled alveoli popping open pulmonary edema, pneumonia, pulmonary fibrosis |
|
|
wheezes in lungs |
air moving through narrowed bronchi can be inspiratory or expiratory |
|
|
dull lung sounds |
be suspicious of pleural effusion |
|
|
absent lung sounds |
be suspicious of pneumothorax |
|
|
normal femoral pulses |
does not rule out heart disease! |
|
|
weak femoral pulses |
diseases leading to decreased forward flow - aortic stenosis - severe DMVD - cardiomyopathies (DCM, HCM, ARVC) |
|
|
bounding pulses |
caused by wide variation between systolic and diastolic pressures w/ a continuous murmur in a puppy, very likely PDA |
|
|
impaired valve closure/valve insufficiency leads to... |
blood regurgitation/backflow of blood |
|
|
factors that affect degenerative diseases |
- age (prevalence, severity increase w/ age) - species - breed - size |
|
|
valves that can be affected by degenerative disease |
all can be affected - AV affected more than semilunar - mitral affected more than tricuspid |
|
|
vet species primarily affected by DMVD |
dog (all species can be affected) |
|
|
mitral valve insufficiency |
- back flow from LV (120) to LA (5) - occurs during ventricular systole when the mitral valve should be closed |
|
|
tricuspid valve insufficiency |
- back flow from RV (25) to RA (5) - occurs during ventricular systole when the mitral valve should be closed |
|
|
aortic valve insufficiency |
- back flow from aorta (80) to LV (0) - occurs during ventricular diastole when the aortic valve should be closed |
|
|
pulmonic valve insufficiency |
- back flow from pulmonary artery (15) to RV (0) - occurs during ventricular diastole when the pulmonic valve should be closed |
|
|
mechanisms of valve insufficiency |
- lesions on the leaflets (degenerative, infectious, congenital) - dilation of the annulus secondary to dilation of the ventricle; the annulus supports the leaflets - rupture of the chordae tendinea (degenerative, infectious, trauma) - displacement of the papillary muscles --> displacement of the chordae tendinea --> disruption of the leaflets |
|
|
mechanism of valve degeneration |
- occurs as a result of aging, inherited factors, mechanical stress, etc.
- accumulation of glycosaminoglycans in spongiosa - "myxomatous changes" - disruption of the organization of the fibrosa - on necropsy: thickening of valve leaflets - chordae tendinea affected w/ thickening and elongation |
|
|
consequences of DMVD
|
- LA volume and pressure increase - increase in pulmonary v. and capillary pressures - pulmonary edema when capillary pressure reaches 20-25 mmHg - pulmonary hypertension, from increased pressure in pulmonary a. - mainstem bronchus compression by enlarged LA - syncope associated w/ atrial dilation - LA tear, chronic endothelial damage from jet of regurgitation --> can result in pericardial effusion/hemorrhage |
|
|
presenting complaints of DMVD |
- incidental finding: murmur - cough - increased RR, resp distress - syncope - weakness, exercise intolerance - weight loss |
|
|
auscultation of a DMVD |
- may hear systolic click at early stages
- left apical systolic murmur |
|
|
evaluation of chest rads for pulmonary edema |
- lateral: caudo-dorsal distribution - DV: right and left caudal; usu more pronounced in R caudal lung lobe |
|
|
NT-proBNP |
- secreted mostly by ventricles in response to wall stress - promotes natriuresis (secretion of Na+, water) - diagnostic test measures the "n-terminal" portion - predict risk for congestive heart failure - differentiate cardiac vs non-cardiac dyspnea |
|
|
"A" DMVD |
- considered at risk - auscult at yearly PE |
|
|
"B1" DMVD |
- considered mild
- obtain baseline rads, BP, +/- echo - then yearly rads, +/- echo |
|
|
"B2" DMVD |
- considered moderate - tx is controversial at this stage - restrict Na in diet, provide high quality protein - rads, BP, echo, chem panel - monitor RR daily - recheck rads/echo q6-12 months - w/ LA enlargement may tx w/ ACE-inhibitor OR pimobendan - w/ clinical signs (syncope or cough) tx w/ ACE-inhibitor OR pimobencan OR furosemide or combo |
|
|
"C" DMVD |
- considered severe - tx for congestive heart failure - restrict Na in diet - rads, BP, echo, chem panel - monitor RR daily - recheck as needed - acute presentation of pulmonary edema tx w/ oxygen, furosemide IV, pimobendan - pulmonary edema at home tx w/ furosemide PO, ACE inhibitor, pimobendan - refractory pulmonary edema tx w/ an additional diuretic (spironolactone and/or thiazide), change diuretic (i.e. torsemide), increase dosing of pimobendan |
|
|
"D" DMVD |
- pulmonary edema refractory to standard tx - monitor as in previous stages - acute presentation of pulmonary edema tx w/ oxygen, furosemide IV, pimobendan - pulmonary edema at home tx w/ furosemide PO, ACE inhibitor, pimobendan - refractory pulmonary edema tx w/ an additional diuretic (spironolactone and/or thiazide), change diuretic (i.e. torsemide), increase dosing of pimobendan |
|
|
enalapril, benazepril |
- ACE-inhibitor - mild increase in natriuresis - vasodilation - decreased angiotensin II and aldosterone synthesis/secretion |
|
|
pimobendan |
- inodilator - positive inotrope - vasodilator |
|
|
furosemide |
- diuretic |
|
|
endocarditis |
- infection on the cardiac valves - 1:1 occurrence on mitral valve and aortic valve - more common in large breed dogs - common causes: Staphylococcus spp., Streptococcus spp., E. coli, bartonella - lesions are called "vegetation", made up of fibrin, platelets, bacteria |
|
|
2-D echocardiography |
- sends sound waves and captures them as they are reflected from soft tissue surfaces to produce an image - produces cross-sectional slices |
|
|
ejection fraction (EF) |
amount/percentage of blood that is pumped/ejected out of the ventricles w/ each contraction |
|
|
M-mode echocardiography |
- displays cardiac structures in a one-dimensional plane - features assoc w/ the image scroll across the monitor, changing in thickness or position as the heart fills and contracts - used to assess size, function |
|
|
fractional shortening |
- fraction of any diastolic dimension that is lost in systole (how much you're contracting) - evaluate degree of shortening of LV diameter between end-diastole and end-systole |
|
|
E point to septal separation |
- measured from the M-mode recording at the mitral valve level - distance between the septum and peak opening of the anterior mitral valve leaflet - LV dilation, aortic insufficiency, mitral valve dysplasia can increase EPSS |
|
|
Doppler echocardiography |
- uses "Doppler principle" to calculate velocity of RBCs - allows detection and analysis of moving blood cells or myocardium - provides info about direction, velocity, character, timing of blood flow or muscle motions |
|
|
Spectral Doppler |
velocity of blood flow is calculated in a region of interest |
|
|
pulsed-wave |
U/S waves are transmitted in pulses, w/ the transducer acting as receiver and transmitter flow is examined at specific sites and region of interest is represented as a sample volume |
|
|
continuous-wave |
blood cells are examined along the beam as the U/S waves can be transmitted and received simultaneously no limit to the velocity that can be recorded |
|
|
Color Doppler |
blood flow is color-coded and superimposed on the black and white 2-D image red (towards), blue (away) velocity is color-coded; high velocities are represented as a mosaic of colors |
|
|
Tissue Doppler |
velocity of myocardial motion is displayed assess systolic and diastolic function and synchronicity |
|
|
R parasternal long-axis four chamber view |
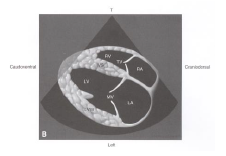
|
|
|
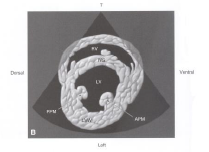
R parasternal long-axis inflow outflow view |

|
|
|
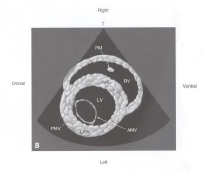
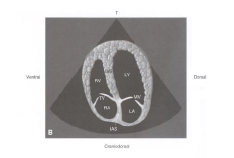
R parasternal short-axis LV w/ papillary muscles view |
|
|
|
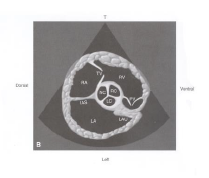
R parasternal short-axis LV w/ mitral valve view |
|
|
|
R parasternal short-axis of the heart base view |
|
|
|
L parasternal apical four chamber view |
|
|
|
M-mode of the LV |
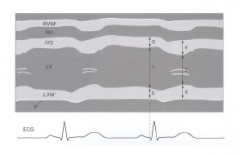
|
|
|
M-mode of the LV at mitral valve level |
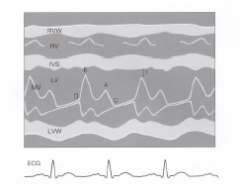
|
|
|
QRS complex |
- results from depolarization of the ventricles
- presence of a QRS complex suggests that the ventricle is depolarizing in a coordinated fashion - normal QRS complexes suggest ventricular depolarization via the His-Purkinjie system |
|
|
P wave |
- results from depolarization of the atria - presence of P waves suggests atria are depolarizing in a coordinated fashion - normal P waves suggest the atria are being paced by the sinus node, and are structurally normal |
|
|
P-R interval |
- represents the time elapsed during AV node conduction - beats that are supraventricular/atrial in origin should have consistent P-R intervals - prolonged P-R interval suggests delayed conduction through the AV node |
|
|
T wave |
- results from ventricular repolarization |
|
|
mean electrical axis |
- axis along which the summed electrical vector caused by ventricular depolarization travels - will be perpendicular to the isoelectric axis |
|
|
ventricular premature complexes (VPCs) |
- abnormal QRS complexes - originate in the ventricle and are wide and bizarre due to abnormal conduction path - can occur singly, as couplets, or triplets - more than 3 VPCs in a row = VTach |
|
|
ventricular tachycardia |
- can be non-sustained/paroxysmal or sustained/non-paroxysmal
- more than three VPCs in a row |
|
|
aberrancy |
- excitable tissue is stimulated during its relative refractory period, resulting in decreased conduction velocity - widens QRS complex - may alter electrical axis |
|
|
first degree AV block |
prolonged P-R interval |
|
|
second degree AV block |
intermittent loss of QRS complexes following P waves |
|
|
third degree AV block |
complete dissociation of P waves from QRS complexes |
|
|
escape beats |
ventricular depolarization via subsidiary pacemakers (AV node or ventricular myocardium) when conduction from the SA node cannot reach the ventricle |
|
|
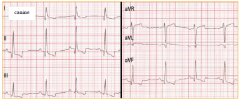
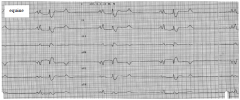
normal canine |
|
|
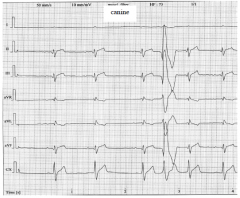
normal equine |
|
|
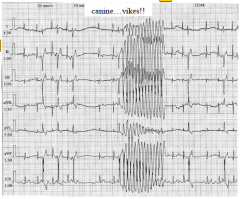
VPCs |
|
|
ventricular tachycardia |
|
|
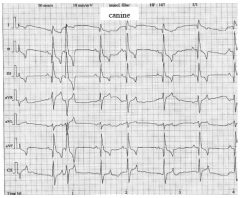
atrial premature complexes |
|
|
first degree AV block |
|
|
second degree AV block |
|

|
third degree AV block |
|
|
HCN |
- hyperpolarization/cyclic nucleotide gated channels - only voltage gated channels that open at relatively depolarized resting membrane potential of -65mV - found in the SA node - facilitates spontaneous depolarization of node |
|
|
conduction from atria to ventricles |
initiated by SA node --> through atria --> to AV node --> to ventricles via His-Purkinje system |
|
|
Na sensitive tissues |
- atrial myocardium - ventricular myocardium - His-Purkinje tissue |
|
|
Ca sensitive tissues |
- SA node - AV node |
|
|
absolute refractory period |
period after a depolarization event during which the channels are inactive, and the cell is completely inexcitable and cannot conduct current |
|
|
relative refractory period |
period after a depolarization event when the channels have begun to recover, but not fully, and the cell has not yet returned to resting membrane potential stimulation of the tissue during the RRP may result in the conduction of current, but the velocity is diminished |
|
|
requirements for reentry
|
- region of non-conduction (may be permanent or temporary/meandering - region of unidirectional block - region of slowed conduction (promotes reentry into previously depolarized tissue following the refractory period) |
|
|
triggered activity |
- possibly caused by spontaneous intracellular Ca release --> activity of Na/Ca exchanger - if oscillations in membrane potential caused by Ca release reach threshold may self perpetuate and cause tachycardia |
|
|
abnormal automaticity |
tissue that does not normally serve as the pacemaker becomes automatic (spontaneously depolarizes) may be due to alteration of resting membrane potential from autonomic tone, hypoxia, drugs... infrequent abnormal automaticity may be a trigger for malignant arrhythmias |
|
|
vulnerable parameter |
component of an arrhythmia accessible to the effect of an antiarrhythmic drug i.e. electrophysiologic substrate, trigger, modulator |
|
|
Class I antiarrhythmics |
- Na channel blockers - decrease phase 0 depolarization rate - decrease conduction - variable effect on action potential duration - use/reverse use dependence - acts on atrial and ventricular myocadrium, His-Purkinje tissue |
|
|
quinidine |
- Class I antiarrhythmic - increases action potential duration - causes peripheral alpha-blockade - tx supraventricular tachycardia (esp a. fib), VTac |
|
|
lidocaine |
- Class I antiarrhythmic - use dependence - shortens action potential duration - tx VPCs, VTac |
|
|
Class II antiarrhythmics |
- beta blockers - subtype selectivity (beta-1 selective) - variable effects on action potential duration - negative inotropes - i.e. atenolol, metoprolol, esmolol |
|
|
Class III antiarrhythmics |
- K channel blockers - prolong action potential duration - prolong refractoriness, delayed repolarization - i.e. sotalol |
|
|
Class IV antiarrhythmics |
- Ca channel blockers - act on nodal tissue - negative inotropes - i.e. diltiazem, verapamil |
|
|
tx of bradyarrhythmias |
- pacemaker implantation - sympathomimetics, parasympatholytics, phosphodiesterase inhibitors may be used as salvage strategies while awaiting device implantation |
|
|
wide complex tachycardias |
- originate outside the His-Purkinje system or depolarize the ventricle by a path that does not traverse the normal His-Purkinje tract - commonly ventricular ectopic rhythms (VTac) - uncommonly impulse from atrium bypass AV node and excite ventricle via bypass tract |
|
|
aberrant conduction |
electrical impulse travels down the His-Purkinje normally, but the system is stimulated during the relative refractory period --> conduction velocity is decreased --> wide QRS |
|
|
narrow complex tachycardias |
narrow complex suggests that depolarization is occurring through the His-Purkinje commonly include supraventricular reentry mediated arrhythmias (afib), and abnormal automaticity in supraventricular region (atrial tachycardia) |
|
|
pericardial effusion |
fluid surrounding the heart within the pericardial space fluid may be hemorrhagic, transudate, or exudate (rare) can occur in any species |
|
|
neoplastic ddx for pericardial effusion |
dogs: - hemangiosarc - chemodectoma - mesothelioma - lymphoma - ectopic thyroid carcinoma cats: - lymphoma - carcinoma |
|
|
non-neoplastic ddx for pericardial effusion |
dogs: - toxin (rodenticide) - LA rupture (w/ severe mitral regurg) - pericardioperitoneal diaphragmatic hernias - hypoalbuminemia - congenital pericardial cysts - immune mediated vasculitis - bacterial/fungal pericarditis - uremia cats: - heart failure (most common) - FIP |
|
|
presentation of pericardial effusion |
collapse vomiting/retching lethargy increased RR abdominal distension |
|
|
PE findings for pericardial effusion |
muffled heart sounds tachycardia weak +/- variable pulses increased CRT, pale mm +/- jugular pulses +/- ascites, hepatosplenomegaly |
|
|
to tap or not to tap? |
tap: - right atrial or ventricular tamponade - pt has clinical signs not: - not in tamponade, no clinical signs, scant fluid - abnormal coags - suspect L atrial rupture |
|
|
risks of pericardiocentesis |
arrhythmias laceration of coronary or atria intra-cardiac puncture pneumothorax (death from procedure is very rare) |
|
|
gross features of HCM |
- ventricular hypertrophy - thickened interventricular septum/free wall >6mm - decreased compliance - L ventricular outflow obstruction |
|
|
histopath findings of HCM |
- myofiber dissarray - intramural arteriosclerosis - fibrosis - CT abnormalities |
|
|
physiology of HCM |
- hypertrophic ventricular walls impair diastolic function (heart can't fill up) --> decreased stroke volume causes cardiac output to decrease --> heart rate increases to maintain cardiac output - w/ increased HR, diastolic filling time decreases, oxygen demand increases and coronary perfusion decreases |
|
|
predisposing factors to thromboembolism w/ HCM |
- dilated left atrium - endocardial injury - stasis - hypercoagulability |
|
|
PE findings w/ HCM |
- L apical systolic murmur - gallop rhythm - abnormal lung sounds - tachycardia - signs of thromboembolism |
|
|
restrictive cardiomyopathy |
- normally to mildly thick walls - mild ventricular dilation - mod to severe atrial dilation - low normal fractional shortening - spontaneous atrial contraction - fibrosis - poor prognosis |
|
|
tx of chronic HCM |
beta-adrenergic antagonists ACE inhibitors furosemide (+/- diuretics) pimobendan (off label use in cats) antithrombotics (aspirin, clopidogril) |
|
|
tx of acute/ER pulmonary edema in cats |
IV/CRI furosemide nitroglycerin ointment (transcutaneous) monitor: RR, HR, RE. mm, chest rads, BUN/creat, electrolytes |
|
|
occult cardiomyopathy |
- no clinical signs are present - echocardiographic changes and arrhythmias can be identified |
|
|
ECG findings of Doberman CM |
ventricular arrhythmias - VPCs - Vtach dx of CM if more than 100 VPC/24 hr, of if signs of complexity |
|
|
echo findings of Doberman CM |
- L ventricular dilation - eccentric hypertrophy - reduced systolic function of L ventricle |
|
|
echo findings of Boxer ARVC |
L ventricle dilation reduction in systolic function |
|
|
ECG findings of ARVC |
VPCs
- 50-300/24 hrs: possible ARVC - >300/24 hrs: likely ARVC VTach syncopal episodes a.fib. if atrial enlargement becomes severe |
|
|
causes of myocarditis |
- viral: parvo, adenoviruses, herpesviruses - bacterial: Borrelia sp. - protozoal: Trypanosoma cruzi - parasitic infection - fungal infection - toxicosis: anthracyclines - hypersensitivity: drug reactions - immunological syndromes: post-infectious, IMB, lupus |
|
|
causes of cardiomyopathies |
primary - congenital/inherited secondary - infection (viral, bacterial, protozoal, parasitic, fungal) - inflammation (hypersensitivity, immunologic) - toxicosis - nutritional deficiency - neoplastic cell infiltrate - arrhythmia/tachycardia induced |
|
|
dilated cardiomyopathy |
- most common in dogs - dilated ventricles - decreased systolic function - causes: inherited, inflammatory, nutritional, tachycardia-induced |
|
|
myocarditis |
- inflammation of the heart muscle - can be mild/transient to fulminant - infectious and non-infectious causes - cardiac function may be normal, but can include acute systolic dysfunction w/o dilation, or DCM - may have arrhythmias, including AV block, brady- or tachy-arrhythmias |
|
|
left heart failure - clinical signs |
- pulmonary edema - pleural effusion |
|
|
right heart failure - clinical signs |
- pleural effusion - ascites - SQ edema (rare in SA) |
|
|
furosemide |
- loop diuretic - most common - diuresis proportionate to dose - w/in 30 mins w/ IV; w/in 2-3 hrs w/ PO - decreased Na, K, Cl and increased in BUN |
|
|
torsemide |
- loop diuretic - stronger than furosemide - diuresis proportionate to dose - PO only - lose H2O, Na, K, Cl |
|
|
hydrochlorothiazide |
- diuretic, acts on distal tubule - strength between furosemide and spironolactone - reaches maximal diuretic effects at low dose - PO only - lose H2O, Na, K, Cl |
|
|
spironolactone |
- K sparing diuretic, acts on collecting duct - questionable diuretic effect - PO only |
|
|
monitoring response to diuretics in CHF |
monitor renal function: - baseline - 7-10 days after beginning tx - after ER tx - after any dose changes monitor for cavitary effusion: - daily RR - repeat chest rads |
|
|
chronic tx of CHF
|
dogs: - furosemide - ACE-inhibitors - beta-blocker - pimobendan - maintain calorie intake, modest salt restriction, monitor K, fish oil cats: - furosemide - ACE-inhibitors +/- pimobendan - monitor K |
|
|
primary goal in a cardiac ER |
restore adequate delivery of oxygenated blood to the periphery |
|
|
overall therapeutic options in cardiac ER |
positive inotropes removal of third space fluid diuretics antiarrhythmics delivery of DC current |
|
|
ECG findings of pericardial effusion |
- decreased R wave amplitude - tachycardia - electrical alterans |
|
|
thoracic rads w/ pericardial effusion |
- globoid pericardial silhouette - pericardiomegaly +/- dilated caudal vena cava |
|
|
echo findings w/ pericardial effusion |
- pericardial fluid +/- tamponade +/- space occupying lesions - caudal vena cava plethora +/- pleural fluid |
|
|
pathophysiology of VTach |
- increase of myocardial oxygen demand --> hypoxia/ischemia --> decreased systolic function, predisposed to malignant arrhythmias - decreased diastolic filling time --> decreased preload, SV and CO |
|
|
tx of VTach |
- not always an ER, may resolve spontaneously, but should be monitored and followed up - indications for tx: poor perfusion, multiphormic VPCs, R on T phenomenon, rapid rate, syncope - tx: lidocaine, procainamide [Na channel blockers], magnesium sulfate [Ca channel antagonist], amiodarone [K channel blocker], esmolol [beta blocker] |
|
|
supraventricular tachycardia |
rapid cardiac rhythm originating or sustained in SA node, atria and/or AV node |
|
|
pathophysiology of SVT |
rapid cardiac rhythms decreases ventricular filling time, preload, stroke volume and cardiac output
myocardial oxygen demand increases --> hypoxia/ischemia --> systolic dysfunction, malignant arrhythmias |
|
|
ECG findings of SVT |
- tachycardia - narrow QRS complexes +/- altered p wave electrical axis +/- absent p waves - p waves buried in previous t waves - r-r interval may be regular or irregularly irregular |
|
|
tx of SVT |
vagal maneuvers cardioversion - Na channel blockers - DC cardioversion - amiodarone diltiazem - Ca channel blocker esmolol - beta-blocker |
|
|
ventricular fibrillation |
disordered, asynchronous electrical depolarization of the ventricles |
|
|
pathophysiology of v. fib. |
loss of coordinated ventricular contraction --> acute cessation of cardiac output EMERGENCY!!! |
|
|
ECG during v. fib. |
rapid, irregular undulations w/o discernible QRS complexes |
|
|
tx of v. fib. |
CPR and DC cardioversion immediately! |
|
|
common heart sounds/murmurs in horses |
- split S2 - tricuspid regurg - mitral regurg - aortic insufficiency |
|
|
atrial fibrillation in horses |
- most common arrhythmia in horses - large atrial mass, high vagal tone (shortens action potential duration) - tx: cardioversion w/ quinidine, electrical conversion, antiarrhythmics in some cases, +/- digoxin |
|
|
second degree AV block in horses |
- high vagal tone - can be walked/jogged w/ repeat ECG to verify if block is physiologic |
|
|
troponin |
- found inside cardiac myoctes and is released into the serum/blood when myocytes are damaged - elevated troponin levels indicates myocyte damage/lysis |
|
|
common congenital defects in horses |
VSD tetrology of Fallot tricuspid valve atresia |

