![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
70 Cards in this Set
- Front
- Back
|
Where do cardiac precursors come from?
|
Primitive streak
-cells destined for heart are identified by Nkx or tinman gene family. |
|
|
When does heart beat begin?
|
Day 18
|
|
|
Where is the aortic sac and outflow tract in regard to the developing heart?
|
-Aortic sac most cranial
-Outflow Tract will divide into bulbus cordus and truncus arteriosus |
|
|
Where does the endocardium originate from?
|
Endocardium - from mesoderm of anterior embryo-continuous with endothelium of blood vessels.
-derived from mesoderm cells known as angioblasts,highly migratory. |
|
|
Where does the myocardium originate from?
|
Myocardium - from precardiac mesoderm
a. contains myocytes and myoblasts b. strongly secretory epithelium c. 1-5 cells thick |
|
|
Where does the pericardium originate from?
|
Epicardium - from dorsal mesentery (PEO)
a. migrates over heart as a sheet b. precursors for coronary vessels |
|
|
What is cardiac jelly?
|
Cardiac jelly - extracellular matrix of the heart
a. Largest concentration of acellular matrix (ECM) in the embryo, secreted by myocytes b. Components include collagen (types I and IV), GAGs, fibronectin, laminin and 40-50 additional proteins c. Adds strength and resiliency to wall |
|
|
What does the neural crest do in regards to the heart?
|
-Participates in the division of the outflow tract, migrates inward.
|
|
|
Describe the looping of the heart?
|
A. Accomplishes the expected orientation of the heart
i. brings inflow to cranial end of heart ii. is genetically programmed but the mechanism for looping is unknown a. malrotation results in situs inversus b. genes involved in looping include sonic " "hedgehog and a form of dynein |
|
|
Describe the looping process?
|
B. Shortly after fusion, the heart
begins to loop to the right. C. Atrium enlarges during looping. D. Once looping is complete, atrium contacts bulbus cordis (posterior of bulbus), ventricle is caudal to atrium |
|
|
What forms the pacemaker cells?
|
Myocytes that have lost their contractile elements.
|
|
|
What connects to the aortic sack?
|
Aortic arch, the pharyngeal arches have a central core artery that connects. Looks like an exhaust manifold.
|
|
|
How is the outflow tract divided?
|
Bulbus cordus and the truncus arteriosis
|
|
|
What are the sinus venosus and sinus horns?
|
Parts of the split heart tube, caudal to outflow before looping.
Proximal caudal heart tube= sinus venosus Distal= sinus horn, initially receives venous blood from various sources. After looping the sinus venosus and horn become tributaries of the right atrium. Right cardinal vein becomes the superior vena cava Left cardinal vein becomes the inferior vena cava Remnant of the left sinus v and horn become coronary sinus. |
|
|
What forms the inlet to the left atrium?
|
The pulmonary veins form into one vessel and puncture the left atrium.
|
|
|
Describe the steps of septation?
|
1. Separation of ventricles from atrium.
2. Division of left and right atrium 3. Division of the ventricles into left and right. 4. Outflow is divided into the two great vessels. |
|
|
Describe step 1 of septation.
|
Occurs during heart looping.
-Cardiac cushions form. expansions of cardiac jelly. -endocardial cells covering cushions undergo epithelial mesenchymal cell transformation. Mesenchymal cells invade jelly and migrate toward myocardium. -These cells eventually produce valves. -the cushions eventually expand across AV canal. Becomes septum intermedium. |
|
|
Describe step 2 of septation.
|
1. Formation of muscle tissue on superior and posterior walls of atrium= septum primum (crescent shaped)
-continues to enlarge and grows towards septum intermedium. The opening between these two flaps of tissue is called the OSTIUM PRIMUM Continued growth of septum primim closes ostium primum, but not before a hole is formed into the primum called the OSTIUM SECUNDUM. -A second flap of tissue forms on the right side which is called the septum secundum which also grows towards the S. intermedium. It does not reach the S intermedium which leaves a hole called the foramen ovale. The S. secundum overlaps the ostium primum causing the blood to flow in a diagonal pattern. -When pressure increases on the left side, the septum primum is pressed against the septum secundum which closes the foramen ovale. With time these flaps close. -the depression caused by the foramen ovale is called the FOSSA OVALIS. |
|
|
Describe step 3 of septation.
|
The interventricular septum is formed of muscle tissue, trabeculae carnae. Fusion occurs at the base, and moves upward. Fusion at the septum intermedium does not occur. This produces the INTERVENTRICULAR FORAMEN.
The interventricular foramen closes when the outflow tract is fully divided. It is closed by extensions of the septum intermedium and the bulbar cusions of the outflow tract. This forms the MEMBRANOUS SEPTUM. |
|
|
Describe step 4 of septation.
|
1. Formation of the bulbar ridges longitudinally.
2. Formation of valves through eithelial mesenchymal cell transormation. 3. Expansion of bulbar ridges by neural crest cells from pharyngeal arches. This causes fusion and completion of the division. Smooth muscle and fibroblasts develop from the neural crest cells. 3. Rotation: Great vessels spiral around each other. 4. Fusion of septum intermedium with interventricular septum separates the lumens. Failure of the ridges to form causes PATENT DUCTUS ARTERIOSUS (PDA) |
|
|
What is PATENT DUCTUS ARTERIOSUS (PDA)?
|
Failure of the outlet tract ridges to fuse= PATENT DUCTUS ARTERIOSUS (PDA)
-mix of high pressure blood going to body and lungs. |
|
|
What is transposition of the great vessels (TGV)
|
-Failure of the ridges to spiral.
-Pulmonary trunk is connected to left ventricle. -Blood from lungs pumped back to lungs, blood from body pumped back to body. A patent ductus arteriosis is pertinent for survival. It can be kept open with admin of prostaglandins or insertion of a stent. |
|
|
What is the role of the ductus arteriosus?
|
Usually closes at birth by contraction which produces the ligamentum arteriosum.
|
|
|
What is the incidence of congenital heart disease?
|
0.6-0.8% of live births.
VSD: 42% ASD: 10% |
|
|
What is the etiology?
|
• Chromosomal abnormalities
(e.g., trisomy 21) • Drugs (e.g., thalidomide) • Viruses (e.g., rubella) • Radiation • Unknown (90+%) |
|
|
What are the basic symptoms of the various defects?
|
Left to right:
Acyanotic to late cyanotic Right to left: Cyanotic Obstructions: acyanotic |
|
|
What are the common causes of left to right shunts?
|
1. VSD
2. ASD 3. PDA 4. AVSD 5. AV Canal |
|
|
Ventricular Septal Defect
|
-Most common
-most are membranous, few are muscular -larger size is much worse |
|
|
Atrial Septal defect
|
Secundum or primum
-90% are secundum |
|
|
Atrioventricular Septal
Defect (AVSD) |
-Conceptually a hole in the middle of the heart.
1/3 of complete AVSD have trisomy 21 |
|
|
Eisenmenger's Syndrome
|
-Left-to-right shunt reverses to right-to-left
-Shunt reversal due to hypertensive pulmonary vascular disease -Can happen with ASD, VSD, AVSD, or PDA -only tx is a heart and lung transplant |
|
|
Right to Left
Tetralogy of Fallot |
Four features:
– VSD – Subpulmonic/pulmonic stenosis – Overriding aorta – Right ventricular hypertrophy |
|
|
Transposition of great vessels
|
Vessels are switched and their is a loop. A shunt is required (PDA, ASD, VSD)
|
|
|
Truncus Arteriosus
|
Single artery receives blood from both ventricles.
-underlying VSD -other abnormalities |
|
|
Tricuspid Atresia
|
-No tricuspid valve
-ASD present -Hypoplastic right ventricle |
|
|
Total Anomalous Pulmonary
Venous Connection/Return (TAPVC/R) |
Pulmonary veins do not enter left atrium, return to other vessels instead.
-ASD -PDA |
|
|
Senile Calcification
|
-Produces aortic stenosis
• Very common with decline of RHD • Age-related: 70 |
|
|
Pathognomonic for Rheumatoid arthritis
|
Aschoff bodies: myocardial nodules of
fibrinoid necrosis surrounded by inflammation with Anitschkow cells— pathognomonic for RF |
|
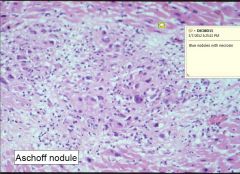
What is this and what is it pathognomonic for?
|
Rheumatoid Arthritis
|
|
|
What valves are typically involved in Rheumatic fever?
|
• Mitral valve alone: 65-70%
• Mitral Plus aortic valve: 25% • Right-sided involvement as well: 5-10% |
|
|
Organ that receives the greatest CO?
Organ that receives the greatest blood flow per gram? |
1. Liver
2. Kidney |
|
|
What is the most important form of regulation for cardiac muscle?
|
Local metabolic:
Hypoxia Adenosine |
|
|
What is the most important form of regulation for cerebral?
|
Local metabolic:
CO2 H+ |
|
|
What is the most important form of regulation for skeletal muscle?
|
Local metabolic:
Autonomic control: Alpha 1 constriction Beta 2 dilation Local control also a factor: lactate, potassium, heat, adenosine. |
|
|
What is the most important form of regulation for skin?
|
Autonomic control
|
|
|
What is the most important form of regulation for pulmonary?
|
Local control: hypoxia vasoconstricts, shunts blood away from poorly perfused areas.
|
|
|
What is the most important form of regulation for renal?
|
myogenic tubuloglomerular feedback
|
|
|
What is a normal ejection fraction?
|
55-65%
|
|
|
What is the ideal aPTT for heparin?
|
5000u Bolus+continuous IV infusion
45-54 seconds, increase dose 55-85 seconds, no change >85 seconds, decrease dose |
|
|
How does PE rank in terms of cause of death?
|
Third in US.
|
|
|
How to prevent DVT and PT.
|
1. Recognize risks and initiate therapy.
2. Recognize and treat DVT. 3. Recognize first PE and initial a preventative therapy. |
|
|
What is Virchows triad?
|
1. Endothelial damage
2. Hypercoagulability 3. Stasis |
|
|
Are DVTs in legs symptomatic.
|
Almost always asymptomatic.
|
|
|
What is the only reliable physical sign of DVT?
|
Unilateral Leg swelling
|
|
|
What is the TX for DVT?
|
1. LMWH or Fondaparinux for at least 5D.
2. Followed by Warfarin tx. |
|
|
Is testing for PE good?
|
No, low sensitivity and low specificity.
|
|
|
What is acute cor pulmonale?
|
Massive PE that obstructs more than 60-75% of pulmonary circulation.
|
|
|
What symptoms should cause suspicion of PE?
If suspected what should you then do? |
Dyspnea, syncope, chest pain
Use clinical probability models (Wells or Geneva) |
|
|
High Probability of PE
|
Chest CT
-CT= got to venous US of legs, VQ scan, VT venogram, digital subtraction angiography |
|
|
Low/Moderate Probability of PE
|
D Dimer
+ D dimer=chest CT -CT=no therapy +CT=treat for PE |
|
|
D Dimer
|
Very sensitive, but not specific.
|
|
|
VQ Scan
|
Absence of perfusion=90% probability of PE.
However, 73% of tests are indeterminate. |
|
|
Chest CT Angio
|
Most useful non invasive test
Sensitivity: 83% Specificity: 96% |
|
|
Treatment of Venous thromboembolism
|
1. LMWH or Fondaparinux should be given when the DX of PE is seriously suspected, 5 days, and until the INR is at least 2.0 for at least 24 hrs.
2. Warfarin should be started with heparin, INR targer 2.5, continued for 3 months -unprovoked episode, for a least a year Alternatives and not tested in randomized trial 1. thrombolytic therapy 2. pulmonary embolectomy 3. catheter fragmentation |
|
|
What is the best combination of therapy for for massive PE with shock?
|
Anticoagulant, lytic, IVC=8% mortality
|
|
|
What hepatotoxic metabolite is produced by acetaminophen?
|
NAPQI
-Increased ETOH consumption or malnutrition decreases CYP induction. |
|
|
What is used for acetaminophen toxicity?
|
N acetylcysteine (NAC)
-tetoxifies NAPQI and replenishes glutathione. |
|
|
Should NSAIDS be given to pregnant women?
If so, which one? |
No, but aspirin is the safest. D/C use well before delivery.
|
|
|
Trans fatty
|
Decrease HDL and increase LDL
|
|
|
What will ingestion of palmitic, lauric, myristic, an stearic saturated fatty acids
|
Palmitic, lauric, myristic, an stearic saturated fatty acids will blunt LDL:LDL receptor interaction.
|

