![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
138 Cards in this Set
- Front
- Back

Pt presents c/ dysphagia and barium swallow shows "bird beak" narrowing |
Achalasia:
-Neuronal degeneration in muscle wall (decreased ganglion cells in Auerbach's plexus) -> Failure of peristalsis, poor LES relaxation after a food bolus -> Dysphagia, regurgitation, weight loss, resp sx -Can get tortuous, dilated esophagus, epiphrenic diverticula, BIRDBEAK appearance -Manometry: HIGH LES PRESSURE, incomplete LES relaxation, NO PERISTALSIS -Tx: Ca channel blocker, LES dilation 60% effective -Nitrates -Failure of medical mgmt => Heller myotomy = L thoracotomy, transect cicular layer of upper and lower esophagus. Also do partial Nissen fundoplication -Trypanosoma cruzi => similar sx |
|
|
Pt presents c/ dysphagia and barium swallow shows "bird beak" narrowing
-This suggests _ -Must R/o _ |
Achalasia:
-Neuronal degeneration in muscle wall (decreased ganglion cells in Auerbach's plexus) -> Failure of peristalsis, poor LES relaxation after a food bolus -> Dysphagia, regurgitation, weight loss, resp sx -EGD to R/O PSEUDOACHALASIA = TUMOR @ GE JUNCTION -Confirm c/ MANOMETRY: HIGH LES PRESSURE, incomplete LES relaxation, NO PERISTALSIS -Tx: Ca channel blocker, LES dilation 60% effective -Nitrates -Failure of medical mgmt => Heller myotomy = L thoracotomy, transect cicular layer of upper and lower esophagus. Also do partial Nissen fundoplication -Trypanosoma cruzi => similar sx |
|
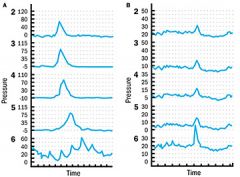
Lady presents to clinic c/ dysphagia, regurgitation, weight loss, resp sx
-Barium swallow shows _ -Manometry shows increased LES pressure, incomplete LES relaxation, no peristalsis -This is consistent c/ diagnosis of _ (manometry normal on L, abnl on R) |
Achalasia:
-Neuronal degeneration in muscle wall -> Failure of peristalsis, poor LES relaxation after a food bolus -> Dysphagia, regurgitation, weight loss, resp sx -Can get tortuous, dilated esophagus, epiphrenic diverticula, BIRDBEAK appearance -Manometry: increased LES pressure, incomplete LES relaxation, NO perstalsis -Tx: Ca channel blocker, LES dilation 60% effective -Nitrates -Failure of medical mgmt => Heller myotomy = L thoracotomy, transect cicular layer of upper and lower esophagus. Also do partial Nissen fundoplication -Trypanosoma cruzi => similar sx |
|
|
during attempted achalasia dilation, gastroenterologist not successful but pt develops chest pain p/ procedure.
-Gastrograffin study normal but thin barium swallow shows peforation -Operative repair of injury should include |
Operative repair: L thoracotomy, myotomy to see extent of injury, butressed repair c/ intercostal muscle or pleura, then short segment myotomy on side opposite of repair to relieve the obstruction
|
|
|
manometry shows failure of LES to relax, lack of peristalsis. Diagnosis is _
|
The manometric criteria of Achalasia are failure of the LES to relax reflexively with swallowing and lack of progressive peristalsis throughout the length of the esophagus. The distal esophageal HPZ pressure is generally normal or elevated, but marked hypertonicity of DES is not seen.
|
|
|
A 40 year-old male presents with symptoms and radiograph consistent with Achalasia. An esophagoscopy fails to reveal neoplasia. The next test to confirm diagnosis is
|
The most important study to diagnose Achalasia is manometry. This study will confirm the failure of LES to relax reflexively with swallowing and lack of progressive peristalsis throughout the length of esophagus.
|
|
|
#1 esophageal cancer = _
|
Adenocarcinoma = #1 esophageal cancer
|
|
|
#1 lung cancer = _
|
Adenocarcinoma = #1 lung cancer
|
|
|
type _ alveoli => functional gas exchange
|
Type 1 alveoli: functional gas exchange
Type 2 alveoli: product surfactant, 1 % of alveoli |
|
|
type _ alveoli => produce surfactant
|
Type 1 alveoli: functional gas exchange
Type 2 alveoli: product surfactant, 1 % of alveoli |
|
|
Angioplasty => __ restenosis by 1 yr
-Vein graft => __% 5-year patency -IMA graft => __% 20-yr patency |
Angioplasty:
-20% restenosis by 1 year -vein graft has 80% 5-yr patency -IMA graft has 95% patency @ 20 yrs |
|
|
#1 cause of ascending aortic aneurysms = _
|
#1 cause of ascending aortic aneurysms =
CYSTIC MEDIAL NECROSIS (e.g. idiopathic #1, Marfans) |
|
|
#1 cause of descending aortic aneurysms = _
|
#1 cause of descending aortic aneurysms =
ATHEROSCLEROSIS - can become large before symptomatic - 5-10% risk of paraplegia - repair indications same as ascending AA - reimplant intercostal vessels below T8 to reduce risk of paraplegia |
|
|
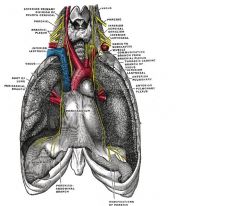
Pt is s/p aortic arch aneurysm repair near the L subclavian artery and deveops a pleural effusion.
Must r/o _ -Tx is _ |
Chylothorax s/p distal aortic arch procedure
-Around the thoracic duct, where it has crossed over to the L side -Can cause LEFT chylothorax -Milky white fluid c/ increases lymphocytes and TAGs (>110 ml/ul); Sudan red stains fast -Fluid resistant to infection -Thoracic duct runs on R chest until T5-> to L side Tx: Conservative x 3-4 wks (chest tube, octreotide, low fat diet or TPN) -Traumatic/ Iatrogenic injury + failure of conservative tx -> Ligation of thoracic duct on R side low in mediastinum 80% successful |
|
|
The _ runs along the R side + dumps into the SVC
|
AZYGOS vein runs posterior R thorax, arches over R main bronchus, + dumps into the SVC
-Transports deoxygenated blood from posterior walls of the thorax + abdomen +/- thoracic , bronchial, even gonadal veins. - formed by union of the ascending lumbar veins + R subcostal veins @ T12 level |
|
|
Pt has longstanding GERD, high grade dysplasia on EGD.
-Therapy is _ |
Barrett's espophagus:
-longstanding reflux -> sq metaplasia to columnar epithelium -50x risk of esophageal adenoca (1-2% risk total) -10-20% of pts c/ high grade dysplasia have undiagnosed esophegeal cancer already -Ass'd c/ p53 (tumor supressor gene) -Severe dysplasia => esophagectomy -Uncomplicated Barrett's is treated like GERD => PPI, Nissen -Nissen decreases esophagitis, progression of metaplasia (does NOT reverse metaplasia or prevent malignancy). Still need f/u EGD for lifetime |
|
|
Barrett's esophagus:
-what type of cell change? -_-_% risk of esophageal adenoca (_-_x risk of ca) -Ass'd c/ _ tumor supressor gene |
Barrett's espophagus:
-longstanding reflux -> sq metaplasia to columnar epithelium -50x risk of esophageal adenoca (1-2% risk total) -10-20% of pts c/ high grade dysplasia have undiagnosed esophegeal cancer already -Ass'd c/ p53 (tumor supressor gene) -Severe dysplasia => esophagectomy -Uncomplicated Barrett's is treated like GERD => PPI, Nissen -Nissen decreases esophagitis, progression of metaplasia (does NOT reverse metaplasia or prevent malignancy). Still need f/u EGD for lifetime |
|
|
Boerhaave's:
-How do you decide which side to do the thoracotomy on? |

Boerhaave's:
-Proximal 2/3 of thoracic esophagus => R thoracotomy -Distal 1/3 of thoracic esophagus (more likely) => L thoracotomy |
|
|
Alcoholic man is taken to the OR hypotensive, tachycardic , L effusion, and pneumothorax.
Suspect _ Most sensitive test is _ |
Boerhave's syndrome:
-Forceful vomiting -> esophageal perforation, usually in L posterolateral wall @ level T8 (inferior esophagus), 3-5 cm above GE junction -> chest pain -Hartman's sign = mediastinal crunching on ascultation -Early diagnosis, tx improve survival -Dx: gastrograffin swallow, followed by thin barium swallow (CT chest +PO/IV contrast is less sensitive) -Lower 1/3 => L thoracotomy, longitudinal myotomy to visualize full extent of injury, primary repair + chest tube -Upper 2/3 of esophagus => R thoracotomy -Esophagectomy for delated presentation, gross mediastinitis |
|
|
Most common location for esophageal perforation in Boerhave's syndrome is _
-Therefore the most common operative approachs is by _ |
Boerhave's syndrome:
-Forceful vomiting -> esophageal perforation, usually in L posterolateral wall @ level T8 (inferior esophagus), 3-5 cm above GE junction -> chest pain -Hartman's sign = mediastinal crunching on ascultation -Early diagnosis, tx improve survival (85% mortality if >36 hrs until dx) -Dx: gastrograffin swallow, followed by thin barium swallow (CT chest +PO/IV contrast is less sensitive) -Lower 1/3 => L thoracotomy, longitudinal myotomy to visualize full extent of injury, primary repair + chest tube -Upper 2/3 of esophagus => R thoracotomy -Esophagectomy for delated presentation, gross mediastinitis |
|
|
Pt is POD 6 after R pneumonectomy for lung cancer and develops fever, serosanguinous sputum
-CXR: lower air-fluid level on pneumonectomy side, but new ipsilateral infiltrate |
Broncho-pleural fistula:
-Serosanguinous sputum, change in air-fluid level on CXR, new infiltrate -Infiltrate is 2/2 aspiration of residual fluid in post-pneumonectomy air space into remaining lung -More common after pneumonectomy vs. lobectomy -Diagnose via bronchoscopy -Tx: thoracotomy, washout -> close stump -> muscle flap over bronchus -> drain + abx |
|
|
Is bronchopleural fistula more common after lobectomy or pneumonectomy?
|
Broncho-pleural fistula:
-Serosanguinous sputum, change in air-fluid level on CXR, new infiltrate -Infiltrate is 2/2 aspiration of residual fluid in post-pneumonectomy air space into remaining lung -More common after pneumonectomy vs. lobectomy -Diagnose via bronchoscopy -Tx: thoracotomy, washout -> close stump -> muscle flap over bronchus -> drain + abx |
|
|
What is a Blalock-Taussif (BT) shunt?
|
Tetrology of Fallot:
-#1 congenital cyanotic heart defect -Anterior + superior displacement of infundibular septum -> 1. malalignment VSD 2.) overriding aortic valve 3. Valvular + infundibular pulmonic stenosis 4.) LV outflow obstruction -> hypertrophic R ventricle -Tx: beta blocker -Operate if increased cyanosis -BLALOCK-TAUSSIG (BT) shunt can be used for palliation to delay repair |
|
|
The internal mammary arteries branch off the _ arteries, collateralize with the _ arteries
|
Internal mammary artery:
-off subclavians -best conduit for CABG: >90% 10-yr graft patency rate -collateralizes with SUPERIOR EPIGASTRIC artery |
|
|
pt is 7 days s/p MI and suddenly develops new murmur, hypotension requiring volume and pressors
-Suspect 2 major causes -Next step = _ |
New murmur or hypotension 7 days after MI;
-Possible ACUTE MITRAL VALVE INSUFF or POST-MI VSD -Get echo |
|
|
Biggest RF for mortality following CABG is _
|
Biggest RF for mortality following CABG = POST-OP CARDIOGENIC SHOCK
-Treat pt c/ shock after MI with PTCA, IABP, medical therapy, NOT CABG |
|
|
IMA graft to LAD has predicted patency of _% at 20 years
|
IMA graft to LAD has predicted patency of 90% at 20 years
|
|
|
SVG graft to a non-LAD coronary artery has predicted patency of _% at 20 years
|
SVG graft has predicted patency of 80% at 20 years
|
|
|
CABG indications (4)
|
CABG indications:
-intractable symptoms 3-vessel dz, 70% LAD + 1 other vessel, or 50% left main |
|
|
Most important determinent of O2 consumption is _
|
Most important determinent of O2 consumption = WALL TENSION
|
|
|
a left-sided chylothorax is most commonly caused by what type of surgery?
|
Distal aortic arch procedure (e.g. aneurysm repair near L SCA) = #1 cause of L Chylothorax
-Milky white fluid, high lymphocytes and TAGs (>110 ml/ul); Sudan red stains fast -Fluid resistant to infection -50% 2/2 trauma or iatrogenic injury, 50% 2/2 posterior mediasinal tumor (esp. lymphoma; 2/2 tumor burden in lymphatics) -Thoracic duct runs on R chest until T5-> to L side -Injury above T5-6 => L chylothorax -Injury below T5-6 => R chylothorax Tx: Conservative x 3-4 wks (chest tube, octreotide, low fat diet or TPN) -Traumatic/ Iatrogenic injury + failure of conservative tx -> Ligation of thoracic duct on R side low in mediastinum 80% successful -Malignant etiology + failure of conservative tx -> mechanical or talc pleurodesis (less successful) |
|
|
Chylothorax:
-Typical management is _ |
Chylothorax;
-Milky white fluid, high lymphocytes and TAGs (>110 ml/ul); Sudan red stains fast -Fluid resistant to infection -50% 2/2 trauma or iatrogenic injury -50% 2/2 posterior mediasinal tumor (esp. lymphoma; 2/2 tumor burden in lymphatics) -Thoracic duct runs on R chest until T5-> to L side -Injury above T5-6 => L chylothorax -Injury below T5-6 => R chylothorax Tx: Conservative x 3-4 wks (chest tube, octreotide, low fat diet or TPN) -Traumatic/ Iatrogenic injury + failure of conservative tx -> Ligation of thoracic duct on R side low in mediastinum 80% successful -Malignant etiology + failure of conservative tx -> mechanical or talc pleurodesis (less successful) |
|
|
Pt gets chylothorax after Ivor-Lewis esophagectomy.
Should be on the _ side Tx: _ |
Chylothorax s/p Ivor-Lewis
= abdominal incision + R thoracotomy -Can cause RIGHT chylothorax -Milky white fluid c/ increases lymphocytes and TAGs (>110 ml/ul); Sudan red stains fast -Fluid resistant to infection -Thoracic duct runs on R chest until T5-> to L side Tx: Conservative x 3-4 wks (chest tube, octreotide, low fat diet or TPN) -Traumatic/ Iatrogenic injury + failure of conservative tx -> Ligation of thoracic duct on R side low in mediastinum 80% successful |
|
|
Distal aortic arch procedures can present with a _-sided chylothorax
|

Chylothorax;
-Milky white fluid c/ increases lymphocytes and TAGs (>110 ml/ul); Sudan red stains fast -Fluid resistant to infection -50% 2/2 trauma or iatrogenic injury -50% 2/2 tumor (lymphoma most common, due to tumor burden in lymphatics) -Thoracic duct runs on R chest (i.e. damage during Ivor-Lewis) until T5-> to L side (i.e. damage during distal aortic arch procedures) -Injury above T5-6 => L chylothorax -Injury below T5-6 => R chylothorax Tx: Conservative x 3-4 wks (chest tube, octreotide, low fat diet or TPN) -Traumatic/ Iatrogenic injury + failure of conservative tx -> Ligation of thoracic duct on R side low in mediastinum 80% successful -Malignant etiology + failure of conservative tx -> mechanical or talc pleurodesis (less successful) |
|
|
4 accessory muscles for inspiration
|
Accessory muscles:
SCM Levators Serratus posterior Scalenes |
|
|
what are the 3 holes in the diaphragm and their T-levels?
|
Diaphragm holes:
T8: IVC T10: esophagus, vagi T12: thoracic duct, aorta |
|
|
Lady presents to clinic c/ dysphagia, regurgitation, weight loss, resp sx
-Manometry shows increased amplitude and duration of esphageal contractions, disorganized contractions, normal LES tone -This is consistnet c/ diagnosis of _ |
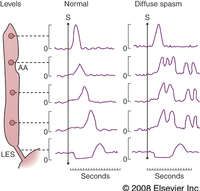
Diffuse esophageal spasm:
-Presentation: chest pain plus the other sx which are similar to achalasia -+/- psych history -Manometry: frequent dysorganized body contractions of high amplitude and duration, NORMAL LES TONE -Nutcracker esophagus presents c/ similar sx but high amplitude peristalsis -Tx: MEDICAL = CA CHANNEL BLOCKER, nitrates, antispasmodics, Heller myotomy = transect circular layer of upper and lower esophagus -Surgery better at resolving dysphagia than pain -Treatment less effective for DES than for achalasia |
|
Diffuse esophageal spasm:
-Tx is _ |
Diffuse esophageal spasm:
-Presentation: chest pain plus the other sx which are similar to achalasia -+/- psych history -Manometry: frequent dysorganized body contractions of high amplitude and duration, NORMAL LES TONE -Nutcracker esophagus presents c/ similar sx but high amplitude contractions -Tx: MEDICAL = CA CHANNEL BLOCKER, nitrates, antispasmodics, Heller myotomy = transect circular layer of upper and lower esophagus -Surgery better at resolving dysphagia than pain -Treatment less effective for DES than for achalasia |
|
|
Ductus arteriosus shunts blood from fetal _ -> _
|
Ductus arteriosus:
-L pulmonary artery -> descending aorta -Shunts blood from fetal lungs |
|
|
Ductus venosum shunts blood from fetal _ -> _
|
Ductus venosum:
-Portal vein -> IVC -Shunts blood from fetal liver |
|
|
Pt presents c/ dysphagia. -
Best initial test = _ |
Dysphagia or Odynophagia:
-Barium swallow = best initial test (EGD, CT not as sensitive) |
|
|
Lady presents to clinic c/ difficulty swallowing solids.
-1st step _ |
Barium swallow = 1st test for dysphagia or odynophagia
(EGD, CT less sensitive in picking up abnormalities) |
|
|
What is Eisenmenger's syndrome:
|
R -> L shunts cause cyanosis
-tetrology, transposition, truncus arteriosus -Cyanosis -> polycythemia, strokes, brain abscess, endocarditis, hypertrophic osteoarthropathy -Children squat to increae SVRI (SVR/BSA), decrease shunt -Eisenmengers: pt has L->R shunt -> pulm HTN -> to R->L shunt (generally irreversible) |
|
|
patient s/p Ivor-Lewis esophagectomy POD#6 develops fevers, increased WBC count.
After IV fluids and sending cx, next step = _ |
Suspected esophageal leak s/p esophagectomy => gastrograffin then thin barium swallow to diagnose leak
-Reexplore if non-contained leak indentified -If tiny leak, can repair + cover with intercostal muscle -If large leak, take down anastomosis, resect necrotic portion, place drains, perform esophagostomy, then possibly reconnect in 3 mo c/ colonic interposition |
|
|
Esophagus layers:
-no serosa -_= strongest layer (in small bowel, _ = strongest) |
Esophagus layers:
-no serosa -mucosa = strongest layer (in small bowel, submucosa = strongest) |
|
|
Upper esophageal sphincter pressure @ rest is ~_ mmHg
During early part of swallow is ~ _mmHg |
UES = cricopharyngeus
-At rest: ~70 mmHg Early swallow: ~ 15 mmHg -Zenker's diverticulum: cricopharyngeous doesn't relax c/ swallowing -> elevated UES pressures -> creates false diverticulum |
|
|
Lower esophageal sphincter pressure @ rest is ~_ mmHg
During swallow is ~ _mmHg |
LES pressure
-At rest: ~15 mmHg During swallow: ~ 0 mmHg -GERD: low LES pressure @ rest |
|
|
what swallowing disease increases the risk of esophageal cancer?
|
Achalasia increases the risk of esophageal cancer
|
|
|
Pt presents c/ dysphagia.
-Barium swallow shows mass -UGI shows smooth intrusion into the lumen -Differential includes 2 things... |
1. Leiomyoma
2. GIST (much less common) Don't biopsy, just enucleate from wall (this is tx for leiomyoma) |
|
|
You believe that a patient has an esophageal leiomyoma.
-Workup includes _ -During workup, do NOT do _ -Therapy is _ |
Esophageal leiomyoma:
-=1 benign esophageal tumor -Sx: dysphagia, pain, usually in lower 2/3 of esophagus -Submucosal (confined to muscularis propia, no mucosal component) -Dx: esophagram, endoscopy to r/o cancer -Do not biopsy => can form scar, make later resection difficult, increases likelihood of disrupting the mucosa ->5 cm or symptomatic => excision (enucleation) via thoracotomy |
|
|
45 yo male presents with recurrent dysphagia and now with retrosternal vague pressure. Upper endoscopy reveals a lesion in lower third of esophagus with grossly normal overlying mucosa. Biopsy reveals a normal mucosal histology. What is the best treatment for this patient?
|
Enucleation of mass. This patient likely has esophageal leiomyoma, a lesion occurring in 3-10% of population between 20-50 years of age. Submucosal enucleation if symptomatic or >5 cm. Generally biopsy is not recommended, as it may complicate the enucleation by scarring. Results are excellent.
|
|
|
Gastroenterologist is attempting balloon dilation for achalasia, but not able to complete it
-Pt c/o chest pain post-op, CXR shows L effusion -Gastrograffin study normal but thin barium swallow shows perforation proximal to LES into chest -Management consists of _ |
Esophageal perf into chest 2/2 dilation for achalasia
-must to L THORACOTOMY for free perforation into L chest -> myotomy to see extent of injury, buttress respair c/ intercostal muscle or pleura, then do short segment myotomy on other size to relieve obstruction -If contralateral myotomy nor done, obstruction neat LES will remain |
|
|
What is the blood supply to the cervical esophagus?
abdominal esophagus? What is arterial supply to gastric tube for esophageal reconstruction? |
Arterial supply to esophagus:
Cervical: inf thyroid A. Abdominal (inc. GE junction): L gastric A., inferior phrenic A's Gastric tube for reconstruction: RIGHT GASTROEPIPLOIC |
|
|
esophageal reconstruction:
-__ artery is main supply to stomach when used to replace esophagus |
esophageal reconstruction:
-R GASTROEPIPLOIC ARTERY = main supply to stomach when used to replace esophagus |
|
|
Patient is POD 6 s/p Ivor-Lewis and develops fever, increased WBC.
-Next step = _ |

Esophagectomy
-5% surgical mortality, 20% cure rate -Divide L gastric, short gastrics -> R gastroepiploic becomes the blood supply to stomach -Transhiatal: abdominal + neck incisions, may have lower mortality due to less fewer esophageal leaks c/ cervical anastomosis -Ivor-Lewis: abdominal incision + R thoracotomy, exposes whole esophagus, intrathoracic anastomosis -Suspect POST-OP LEAK => gsatrograffin swallow, followed by thin barium swallow |
|
|
Patient is POD 6 s/p Ivor-Lewis and develops fever, increased WBC.
-Gets gastrograffin study, followed by thin barium -> shows non-contained constrast leak @ level of anastomosis -Next step = _ |
Patient is POD 6 s/p Ivor-Lewis and develops fever, increased WBC.
-Gets gastrograffin study, followed by thin barium -> shows non-contained constrast leak @ level of anastomosis -RE-EXPLORE to find source of leak -If it's just a tiny hole at anastomosis with viable tissue surrounding, then repair + reinforce with pleura, pericardial fat, or intercostal muscle, and place drains -> NPO + J-tube feeds x 1 week -> repeat swallow study |
|
|
Patient is POD 6 s/p Ivor-Lewis and develops fever, increased WBC.
-Gets gastrograffin study, followed by thin barium -> shows non-contained constrast leak @ level of anastomosis -Re-explore, find large area of necrosis in stomach -Next step = _ |
Patient has leak after esophagectomy, large area of necrotic stomach on re-exploration.
-Take down anastomosis, resect necrotic portion of stomach, perform esophagostomy -Wait 3 MONTHS before re-anastomosis, likely c/ colonic interposition |
|
|
Esophagectomy:
-_%cure rate -_% mortality |
Esophagectomy
-5% surgical mortality, 20% cure rate -Divide L gastric, short gastrics -> R gastroepiploic becomes the blood supply to stomach -Transhiatal: abdominal + neck incisions, may have lower mortality due to less fewer esophageal leaks c/ cervical anastomosis -Ivor-Lewis: abdominal incision + R thoracotomy, exposes whole esophagus, intrathoracic anastomosis -3-hole: abdominal, thoracic, and cervical incisions -Requires pyloromyotomy -Colonic interposition: for young pts c/ benign dz, to preserve gsatric fx, 3 anastomoses required, blood supply depends on marginal vessels -Contrast study POD 7 to r/o leak -Post op stricture: most can be dilated -Palliative esophagectomy indicated in most circumstances |
|
|
what are the indications for neoadjuvant chemo/XRT for GE junction cancer?
|
GE junction cancer: neoadjuvant chemo/CXT needed if T3/4 or N+ (determined by EUS)
-Generally surgery 1st if T1/2 -Do staging c/ PET CT |
|
|
Pt has type _ hiatal hernia:
-Hole in diaphragm beside esophagus Tx is _ |
Type 2 hiatal hernia:
-Paraesophageal, 2/2 hole in diaphragm beside esophagus, normal GE junction -Sx: chest pain, dysphagia, early satiety -Tx: REPAIR 2/2 high risk of incarceration -Nissen needed to anchor stomach, since diaphragm repair can affect LES |
|
|
Most patients with significant reflux have a type _ hiatal hernia
|
Type 1 hiatal hernia:
-Most pts c/ significant GERD have a type 1 hiatal hernia -Most pts c/ type 1 hernia do NOT have GERD -=sliding hernia 2/2 hiatal dilation (most common) |
|
|
What is therapy for a type 2 hiatal hernia?
|
Type 2 hiatal hernia:
-Paraesophageal, 2/2 hole in diaphragm beside esophagus, normal GE junction -Sx: chest pain, dysphagia, early satiety -Tx: REPAIR 2/2 high risk of incarceration -Nissen needed to anchor stomach, since diaphragm repair can affect LES |
|
|
What is a type 4 hiatal hernia?
|
Type 4 hiatal hernia;
-Whole stomach in chest, plus another organ (e.g. colon, spleen) |
|
|
Cachetic pt presents c/ eyelid droop and tiny pupil
-Suspect _ -Mechanism is _ -Tx is _ |
Horner's syndrome 2/2 pancoast tumor = superior sulcus tumor:
-Invasion of sympathetic chain @ T1 -> ptosis, miosis, anhydrosis -Superior sulcus tumors that invade the sympathetic ganglia only or just the lowest root of the brachial plexus can be resected |
|
|
What is hypertrophic osteoarthropathy?
|
Hypertrophic osteoarthropathy
|
|
|
IABP:
-works by 2 mechanisms -inflates 40 msec before _ wave, deflates with the _ wave |

IABP:
-augments diastolic coronary blood flow, reduces afterload by inflating during diastole -inflates 40 msec before T wave; deflates with P wave |
|
|
the internal mammary arteries branch off the _ arteries
|
Internal mammary AKA internal thoracic artery:
-From subclavian artery (inferior surface of the 1st part of SCA, opposite the thyrocervical trunk). -Descends behind the upper six ribs within 2 cm of the sternal edge. -Gives origin to the pericardiacophrenic artery, mediastinal arteries, pericardial branches, sternal branches, anterior intercostal branches and perforating branches. -Divides into the MUSCLOPHRENIC and SUPERIOR EPIGASTRIC ARTERIES at the sixth intercostal space. |
|
|
normal LES pressure @ rest and during swallow are ...
|
LES pressure
-At rest: ~15 mmHg During swallow: ~ 0 mmHg -GERD: low LES pressure @ rest |
|
|
In a child with L-> R shunt, what do you look for to detect CHF?
|
L->R shunts:
-VSD, ASD, PDA -cause CHF -Failure to thrive, increased HR, tachypnea, hepatomegaly -HEPATOMEGALY = 1st sign of CHF in child |
|
|
The _ runs along the R side, crosses midline @ T4-5, dumps into L SC vein @ junction c/ IVC
|
THORACIC DUCT runs along the R side, crosses midline @ T4-5, dumps into L SC vein @ junction c/ IVC
|
|
|
The _ mainstem bronchus is longer than the _
|
LEFT mainstem bronchus is longer than RIGHT
|
|
|
_ pulmonary artery is longer than _ before 1st branch
|
RIGHT pulmonary artery is longer than LEFT before 1st branch
|
|
|
R lung volume = _%, L lung volume = _%
|
R lung volume = 55%, L lung volume = 45%
|
|
|
During quiet inspiration,
diaphragm does _% of work, intercostals _% |
During quiet inspiration,
diaphragm does 80%, intercostals 20% |
|
|
Parietal pleura produces _-_ L of pleural fluid/day
-cleared by _ |
Parietal pleura produces 1-2 L of pleural fluid/day
-cleared by lymphatics in visceral pleura |
|
|
Lung cancer staging:
T1 is <_ cm |
Lung cancer staging:
-T1 < 3cm; T2 >3 cm T3 =invades chest wall, pericardium, diaphragm, <2cm from carina T4 = unresectable = mediastinum, heart, great vessels, esophagus, trachea, vertebrae, malignant effusion |
|
|
Lung cancer staging:
T3 is __ |
Lung cancer staging:
-T1 < 3cm; T2 >3 cm T3 =invades chest wall, pericardium, diaphragm, <2cm from carina T4 = unresectable = mediastinum, heart, great vessels, esophagus, trachea, vertebrae, malignant effusion |
|
|
A 62-year-old, asymptomatic woman with a 60-pack-year smoking history presents with a new, 2x2-cm nodule in the left lower lobe of the lung not seen on a chest x-ray two years ago. A thorough history and physical examination is otherwise normal. The next step in management should be _
|
lobectomy
solitary pulmonary nodule (SPN) or coin lesion is a mass in the lung smaller than 3 centimeters in diameter. It can be an incidental finding found in up to 0.2% of chest X-rays[1] and around 1% of CT scans. most commonly represents a benign tumor such as a granuloma or hamartoma, but in around 20% of cases it represents a malignant cancer. 10 to 20% of patients with lung cancer are diagnosed in this way |
|
|
Pt presents c/ 3 cm RLL mass on CT chest, found to be adenoca
-Mediastinoscopy: R paratracheal node (+) -Next step = _ |
Mediastinoscopy:
-Paratracheal nodes = N2 => unresectable -Must do chemo-XRT -Some protocols allow resection of primary tumor following chemo-XRT + mediastinal LN dissection if good response |
|
|
Lung cancer with R mediastinal lymphadenopathy -
where is the cancer? |
L lung can drain to R mediastinum
(L -> R like reading) |
|
|
During mediastinoscopy, look out for 4 things on the left..
|
Mediastinoscopy:
-Left side: RLN, esophagus, aorta, main PA -Right side: azygous, SVC -Anterior: innominate vein, innominate artery, R PA |
|
|
During mediastinoscopy, look out for 2 things on the right..
|

Mediastinoscopy:
-Left side: RLN, esophagus, aorta, main PA -Right side: azygous, SVC -Anterior: innominate vein, innominate artery, R PA |
|
|
During mediastinoscopy, look out for 3 things anteriorly..
|

Mediastinoscopy:
-Left side: RLN, esophagus, aorta, main PA -Right side: azygous, SVC -Anterior: innominate vein, innominate artery, R PA |
|
|
Patient c/ myasthenia gravis c/o progressive sx despite optimal medical tx (steroids, plasmapheresis, Tensilon)
-Appropriate management is _ |
Myasthenia gravis:
-Fatigue, weakness, diplopia, ptosis -Ab's to acetylcholine R's -Tx: anticholinesterase meds -80% improve after thymectomy -Getting worse despite optimal medical tx (steroids, plasmapheresis, Tensilon) => THYMECTOMY (even if thymus is normal or hypotrophic) -10% of myasthenia gravis pts have thymomas, but 50% of pts c/ thymomas have myasthenia gravis |
|
|
Pt presents c/ neck mass and c/o fatigue and double vision
-Suspect _ -Tx is _ |
Myasthenia gravis:
-Fatigue, weakness, diplopia, ptosis -Ab's to acetylcholine R's -Tx: anticholinesterase meds -80% improve after thymectomy -Getting worse despite optimal medical tx (steroids, plasmapheresis, Tensilon) => THYMECTOMY (even if thymus is normal or hypotrophic) -10% of myasthenia gravis pts have thymomas, but 50% of pts c/ thymomas have myasthenia gravis |
|
|
_ = #1 determinant of myocardial O2 consumption
|
WALL TENSION = #1 determinant of myocardial O2 consumption
|
|
|
What non-small cell lung ca is known for higher local recurrence rates?
|
Squamous cell ca:
-Usually central -Higher rates of LOCAL RECURRENCE -Paraneoplastic syn: PTH-rp release |
|
|
what is treatment of Paget von Schrotter's disease?
|
Paget von Schrotter's dz = acute SCV thrombosis after repetitive activity, e.g. pitchers
-Tx: THROMBOLYTIC to open the vein -> usually proceed to 1st rib resection during that hospitalization |
|
|
Cachetic pt presents c/ claw hand
-Suspect _ -Mechanism is _ -Tx is _ |
Brachial plexus invasion by pancoast tumor = superior sulcus tumor
-ULNAR nerve sx most commonly -Superior sulcus tumors that invade the sympathetic ganglia only or just the lowest root of the brachial plexus can be resected |
|
|
Pancoast tumor:
-involves sympathetic chain (Horner's syndrome) and/or _ nerve |
Pancoast tumor:
-involves sympathetic chain @ T1 (Horner's syndrome) and/or ulnar nerve |
|
|
indications for resection of pancoast tumor
|

Pancoast tumor can be resected if:
- invading only the sympathetic chain ganglia OR -only the lowest nerve root of the brachial plexus |
|
|
paraesophageal hernia:
-Tx is _ |
paraesophageal hernia:
-always operate 2/2 risk of incarceration, strangulation |
|
|
PDA: operative indication
|
PDA:
operate (by L thoracotomy) if not closed by 6 months with indomethacin - L to R shunt - use PGE1 to keep it open if transposition of great vessels - |
|
|
Pre-op PFTs: required FEV1s
>_L for pneumonectomy >_L for lobectomy >_L for wedge -need post-op predicted FEV1>_ |
Pre-op PFTs: required FEV1s
>2L for pneumonectomy >1L for lobectomy >0.6L for wedge -need post-op predicted FEV1> 800 cc |
|
|
Pulm fx testing before lung resection:
-Need predicted post-op FEV1 >_ (or ar least _% of predicted value) -If it’s close, get a _ to determine _ |
Pre-op pulm fx testing:
-Need predicted post-op FEV1 of at least 800 cc (or ar least 40% of predicted value) -If it’s close, get V/Q scan (use the perfusion portion) to determine contribution of that lung portion to overall FEV1 (if low, may still be able to resect) -R lung 55%, L lung 45% |
|
|
Pulm fx testing before lung resection:
-Need predicted post-op DLCO>_-_ mL/min/mmHg CO (at least _% of predicted value) |
Pulm fx testing before lung resection:
-Need predicted post-op DLCO >11-12 mL/min/mmHg CO (at least 50% of predicted value) (this # depends on pulm capillary surface area, Hgb content, alveolar architecture) |
|
|
Phrenic nerve runs anterior or posterior to hilum?
|
Phrenic nerve runs ANTERIOR to hilum
-Also anterior to the anterior scalene |
|
|
Type _ pneumocytes do gas exchange
|
Type 1 pneumocytes do gas exchange
|
|
|
Type _ pneumocytes make surfactant
|
Type 2 pneumocytes make surfactant
|
|
|
To be a candidate for pneumonectomy, pt must have FEV-1 >_ cc to give a reasonable chance of not being ventilator-dependent
-Preduct this based on PFTs and test _ |
To be a candidate for pneumonectomy, pt must have FEV-1 >800 cc to give a reasonable chance of not being ventilator-dependent
-R lung = 55% of ventilation -L lung = 45% of ventilation -Use PEFUSION portion of V/Q scan to predict (i.e. if pt has FEV1 1200 but L lung only gets 10% of pefusion, you can still remove the lung) |
|
|
How do you use a V/Q scan to predict pulmonary function following pneumonectomy
|
To be a candidate for pneumonectomy, pt must have FEV-1 >800 cc to give a reasonable chance of not being ventilator-dependent
-R lung = 55% of ventilation -L lung = 45% of ventilation -Use PEFUSION portion of V/Q scan to predict (i.e. if pt has FEV1 1200 but L lung only gets 10% of pefusion, you can still remove the lung) |
|
|
What do the pores of Kahn do?
|
Pores of Kahn direct air exchange b/w alveoli
|
|
|
What are 3 things that cause pseudo-achalasia?
|
Pseudo-achalasia:
-70% caused by esophageal or gastric malignancy -30% caused by strictures -If pt presents c/ dysphyagia and barium swallow shows distal tapering + failure of LES relaxation, must do EGD to r/o pseudoachalasia |
|
|
How is PVR calaculated?
|
(PA pressure - wedge) x 80 = CO x PVR
(delta P = flow x resistance) |
|
|
Pt c/ scleroderma presents c/ dysphagia
-Best therapy is _ |
Scleroderma dysphagia;
-Loss of LES tone, strictures, fibrous replacement of smooth muscle -> dysphagia -Tx: esophagectomy -Nissen may be effective in some |
|
|
what lung cancer produces ACTH, ADH?
|
Small cell lung cancer:
-20% of lung cancer neuroendocrine in origin. ACTH, ADH ->95% unresectable @ time of diagnosis, get CHEMO-XRT = CISPLATIN, ETOPOSIDE. -Very poor prognosis. 50% 5-yr survival for T1N0M0 -Paraneoplastic syn: ACTH > ADH |
|
|
Paraneoplastic syndromes are most common in _ type of lung cancer
|
Small cell lung cancer:
-20% of lung cancer neuroendocrine in origin. ACTH, ADH ->95% unresectable @ time of diagnosis, get CHEMO-XRT = CISPLATIN, ETOPOSIDE. -Very poor prognosis. 50% 5-yr survival for T1N0M0 -Paraneoplastic syn: ACTH > ADH |
|
|
Small cell lung cancer:
-Typical therapy is _ -5-yr survival if T1N0M0 is _% -<_% 5-yr survival overall |
Small cell lung cancer:
-20% of lung cancer neuroendocrine in origin. ACTH, ADH ->95% unresectable @ time of diagnosis, get CHEMO-XRT = CISPLATIN, ETOPOSIDE. -Very poor prognosis. 50% 5-yr survival for T1N0M0 -Paraneoplastic syn: ACTH > ADH |
|
|
Spontaneous pneumothorax:
-_:1 male predilection -__% recur; _% those recur again -Indications for thoracoscopy |
Spontaneous pneumothorax:
-10:1 male predilection -50% recur, then 75% of those recur again -Do thoracoscopy for 2nd or continued air leak |
|
|
what lung cancer produces PTH-rp?
|
Squamous cell ca:
-Usually central -Higher rates of LOCAL RECURRENCE -Paraneoplastic syn: PTH-rp release |
|
|
A 78 yo male with history of heavy smoking presents with a nodule on right lower lobe. Bronchoscopy reveals squamous cell carcinoma. The most likely symptom of this patient at presentation was
|
The most common symptom at presentation is coughing (75%).
Other symptoms: dyspnea (60%), chest pain (50%), hemoptysis (30%), and weight loss (20-70%). |
|
|
Cachetic pt presents c/ swollen face, arms, hands.
-Suspect _ -Tx is _ |
SVC syndrome:
-Swelling of upper extremities, face -90% of cases are 2/2 lung cancer invading SVC = a T4 tumor = unresectable due to mediastinal invasion -Tx = XRT (resection if a very small portion of SVC involved, e.g. incidental finding during thoracotomy) |
|
|
SVC syndrome:
-_% are 2/2 lung cancer -Tx is _ |
SVC syndrome:
-Swelling of upper extremities, face -90% of cases are 2/2 lung cancer invading SVC = a T4 tumor = unresectable due to mediastinal invasion -Tx = XRT (resection if a very small portion of SVC involved, e.g. incidental finding during thoracotomy) |
|
|
Swallowing function:
-_ initiates swallow, which elicits primary peristalsis -_ then elicits secondary peristalsis. -Sphincters are contracted @ rest -Normal LES _ cm, tone _-_ mmHg |
Swallowing fx:
-Central input initiates swallow, which elicits primary peristalsis -Distension then elicits secondary peristalsis. -Sphincters are contracted @ rest -Normal LES 4 cm, tone 15-25 mmHg |
|
|
Swallowing function:
-soft palate closes nasopharynx -> _ -> larynx closes -> __ -> pharyngeal contraction |
Swallowing fucntion:
-soft palate closes nasopharynx -> larynx up -> larynx closes -> UES relaxes -> pharyngeal contraction |
|
|
Takayasu arteritis:
-population is _ -involves vessels ... -Diagnosed by _ |
Takayasu arteritis:
-young female -involves thoracic and ab aorta and PA -Diagnosed by angio |
|
|
#1 congenital cyanotic heart disease is _
|
Tetrology of Fallot:
-#1 congenital cyanotic heart defect -Anterior + superior displacement of infundibular septum -> 1. malalignment VSD 2.) overriding aortic valve 3. Valvular + infundibular pulmonic stenosis 4.) LV outflow obstruction -> hypertrophic R ventricle -Tx: beta blocker -Operate if increased cyanosis -Blalock-Taussig (BT) shunt can be used for palliation to delay repair |
|
|
what are the components of tetrology of fallot?
|
The tetralogy of Fallot is the most common cyanotic heart defect.
VSD, RV hypertrophy, overriding aorta, and pulmonary stenosis. |
|
|
how does squatting help a Tet spell?
|
The tetralogy of Fallot is the most common cyanotic heart defect.
VSD, RV hypertrophy, overriding aorta, and pulmonary stenosis. -Squatting increases SVR -> L to R shunt -> increases pulm blood flow |
|
|
Thoracic duct runs along the _ side of chest until T_-T_ vertebra, then crosses over to the _ side
|
Chylothorax;
-Milky white fluid c/ increases lymphocytes and TAGs (>110 ml/ul); Sudan red stains fast -Fluid resistant to infection -50% 2/2 trauma or iatrogenic injury -50% 2/2 tumor (lymphoma most common, due to tumor burden in lymphatics) -Thoracic duct enters chest on R c/ aorta @ T12 (i.e. damage during Ivor-Lewis) -> to L side @ T4-5 -> joins IJ/L SC junction -Injury above T5 => L chylothorax -Injury below T5 => R chylothorax Tx: Conservative x 3-4 wks (chest tube, octreotide, low fat diet or TPN) -Traumatic/ Iatrogenic injury + failure of conservative tx -> Ligation of thoracic duct on R side low in mediastinum 80% successful -Malignant etiology + failure of conservative tx -> mechanical or talc pleurodesis (less successful) |
|
|
Thoracic duct injury:
-Tx = _ |
Thoracic duct injury:
-Chylothorax = milky white fluid c/ increases lymphocytes and TAGs (>110 ml/ul); Sudan red stains fast -Thoracic duct runs on R chest (i.e. damage during Ivor-Lewis) until T5-> to L side -Injury above T5-6 => L chylothorax -Injury below T5-6 => R chylothorax -Tx: drainage/NPO x 2 wks -if not resolved, then R thoracotomy + ligate duct |
|
|
What is the rate of symptom resolution adter surgery for thoracic outlet syndrome?
|

60% success rate (complete symptom resolution) after surgery for throacic outlet syndrome
|
|
|
during supra-clavicular approach for thoracic outlet syndrome surgery, phrenic nerve is located where in relation to the scalene muscles?
|
Thoracic outlet syndrome:
-Brachial plexus (usually C8-T1) = most commonly affected -PHRENIC NERVE RUNS ANTERIOR TO ANT SCALENE -Long thoracic nerve is posterior to middle scalene -Branchial plexus + SCA go through a triangle = superior to 1st rib, posterior to ant scalene, anterior to middle scalene. SCV also over 1st rib but anterior to ant scalene. -#1 anatomic abnormality = cervical rib -Sx: NEURO (brachial plexus, esp. ULNAR nerve)> vascular sx (1-3%) affecting the back and neck. -Adson's test: turn head to ipsilateral side -> compresses SCA -> decreases radial pulse -Tinsel's test: tapping reproduces sx -Dx: CXR, C spine x-ray, angiography if thought to be vascular etiology, EMG |
|
|
during supra-clavicular approach for thoracic outlet syndrome surgery, long thoracic is located where in relation to the scalene muscles?
|

Thoracic outlet syndrome:
-Brachial plexus (usually C8-T1) = most commonly affected -Phrenic nerve and SCV are anterior to anterior scalene. -LONG THORACIC NERVE: POSTERIOR TO MIDDLE SCALENE -Branchial plexus + SCA go through a triangle = superior to 1st rib, posterior to ant scalene, anterior to middle scalene. -#1 anatomic abnormality = CERVICAL RIB -Sx: NEURO (brachial plexus, esp. ULNAR nerve)> vascular sx (1-3%) affecting the back and neck. -Adson's test: turn head to ipsilateral side -> compresses SCA -> decreases radial pulse -Tinsel's test: tapping reproduces sx -Dx: CXR, C spine x-ray, angiography if thought to be vascular etiology, EMG |
|
|
Most common anatomic structure involved in thoracic outlet syndrome is _
|
Thoracic outlet syndrome:
-BRACHIAL PLEXUS (usually C8-T1) = most commonly affected -Phrenic nerve is anterior to anterior scalene -Long thoracic nerve is posterior to middle scalene -Branchial plexus + SCA go through a triangle = superior to 1st rib, posterior to ant scalene, anterior to middle scalene. SCV also over 1st rib but anterior to ant scalene. -#1 anatomic abnormality = CERVICAL RIB -Sx: NEURO (brachial plexus, esp. ULNAR nerve)> vascular sx (1-3%) affecting the back and neck. -Adson's test: turn head to ipsilateral side -> compresses SCA -> decreases radial pulse -Tinsel's test: tapping reproduces sx -Dx: CXR, C spine x-ray, angiography if thought to be vascular etiology, EMG |
|
|
thoracic aorta aneurysm:
-Operative indications (2) |
Thoracic aortic aneurysm:
-operate if >6 cm or symptomatic (more specifically: acutely symptomatic, 7 cm, 6 cm + Marfans, diameter 2x normal, rapid increase in size) |
|
|
Thymoma:
-do all need to be resected? __ of myasthenia gravis patients have thymomas -_% of myasthenia gravis patients experience improvement with resection |

Thymoma:
-indication for resection -10% of myastenia gravis have thymomas -resecting thymus (even if no thymoma) in M.G. experience improvement |
|
|
Tissue valves - 2 main indications
|
Tissue valves:
-shorter lasting but no anticoag needed -Population: may become pregnant, contraindication to coumadin, all mitral valves |
|
|
V/Q ratio is highest in the _ portion of lungs
|
V/Q ratio:
-Highest @ apex (when pt seated): alveoli are most open @ apex, but gravity brings most of the blood to lower lobes -When pts posterior for prolonged periods, anterior portions get more expanded and gravity brings blood posteriorly |
|
|
Vagus nerve runs anterior or posterior to hilum?
|
Vagus nerve runs POSTERIOR to hilum
|
|
|
#1 congenital heart defect is _
|
VSD:
-#1 congenital heart defect -L-R shunt -50% close on their own, most by 6 mo -Large VSDs cause sx after 4-6 wks, 2/2 decreased PVR -Sx: CHF, FTT, tachypnea, tachycardia -Medical tx: diuretics, digoxin Repair if: -FTT 2/2 CHF (#1 reason) -Age 5 if doesn't close spontaneously -PVR > 4-6 Woods units -PVR > 10-12 Woods units = CONTRAINDICATION (use vasodilators to see if it is reversible -> if so, then repair) |
|
|
VSD:
-__% close on their own (most by __ months) -operate if ... |
VSD:
-#1 congenital heart defect -L-R shunt -50% close on their own, most by 6 mo -Large VSDs cause sx after 4-6 wks, 2/2 decreased PVR -Sx: CHF, FTT, tachypnea, tachycardia -Medical tx: diuretics, digoxin Repair if: -FTT 2/2 CHF (#1 reason) -Age 5 if doesn't close spontaneously -PVR > 4-6 Woods units -PVR > 10-12 Woods units = CONTRAINDICATION (use vasodilators to see if it is reversible -> if so, then repair) |
|
|
Post-MI VSD:
-Day _-_ -_% of MIs -__ murmur |
Post-MI VSD:
-Day 2-7 -2% of MIs -Pan-systolic murmur |
|
|
62 year old male presents to ER one week after MI with dyspnea. Chest auscultation reveals a pan-systolic murmur. Transthoracic echocardiography is most likely to reveal what?
|
Ventricular Septal Defects present day 2-7 after myocardial infarction (in 2% of MI's) as pan-systolic murmur heard during chest auscultation. Pan-systolic murmur heard after MI may also suggest mitral regurgitation from a ruptured papillary muscle.
|
|
|
Woods units are …
|
Woods units = units of vascular resistance frequently used by pediatric cardiologists
|
|
|
Pt c/o dysphagia.
-Elevated UES pressure while swallowing |
Zenker's diverticulum:
-2/2 high UES (cricopharyngeus) pressure during swallowing (normal 70 mmHh @ rest, 15 mmHg in early swallow) -False diverticulum, pulsion-type, (posterior) in Killian's traingle, b/w oblique + horizontal fibers of cricopharyngeus and pharyngeal constrictors -Sx: upper esophageal dysphagia, choking, halitosis -Dx: barium swallow, manometry -Risk for perforation c/ EGD and Zenkers -Tx: CRICOPHARYNGOMYOTOMY and diverticulectomy/pexy if possible (diverticulum itself can be resected or suspended upward so that it drains into the esophagus) -L cervical incision; leave drains in; esophagogram POD 1 -Almost all have hiatal hernia also many have GERD |
|
|
Zenker's diverticulum:
-2/2 ___ -Location -Tx is _ |
Zenker's diverticulum:
-2/2 high UES (cricopharyngeus) pressure during swallowing (normal 70 mmHh @ rest, 15 mmHg in early swallow) -False diverticulum, pulsion-type, (posterior) in Killian's traingle, b/w oblique + horizontal fibers of cricopharyngeus and pharyngeal constrictors -Sx: upper esophageal dysphagia, choking, halitosis -Dx: barium swallow, manometry -Risk for perforation c/ EGD and Zenkers -Tx: CRICOPHARYNGOMYOTOMY and diverticulectomy/pexy if possible (diverticulum itself can be resected or suspended upward so that it drains into the esophagus) -L cervical incision; leave drains in; esophagogram POD 1 -Almost all have hiatal hernia also many have GERD |
|
|
Pt presents c/ neck mass and c/o fatigue and double vision
-Suspect _ -Tx is _ |
Myasthenia gravis:
-Fatigue, weakness, diplopia, ptosis -Ab's to acetylcholine R's -Tx: anticholinesterase meds -80% improve after thymectomy -Getting worse despite optimal medical tx (steroids, plasmapheresis, Tensilon) => THYMECTOMY (even if thymus is normal or hypotrophic) -10% of myasthenia gravis pts have thymomas, but 50% of pts c/ thymomas have myasthenia gravis |

