![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
20 Cards in this Set
- Front
- Back
- 3rd side (hint)
|
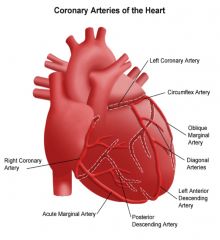
Identify the major coronary arteries
|
|
Left coronary artery
Right coronary artery Left anterior descending artery LAD Posterior descending artery (posterior interventricular artery) Left circumflex artery Right marginal artery |
|
|
Define collateral circulation?
And its significance in ischaemic heart disease. |
Coronary arteries can join and provide a collateral circulation to the cardiac muscle, bypassing occluded vessels and assisting in perfusing the myocardium.
Particulary in older people with established ischaemic heart disease, which means they have the capacity to tolerate occluded vessels. |
|
|
|
Hypertension as it applies to left ventricular haemodynamics
(in relation to afterload) |
Hypertension creates a situation where the right ventrical is pumping the usual volume of blood (at a faster rate) through the lungs and into the left ventricle which, because of its high aortic afterload, cannot pump the same volume of blood out and so the lungs become congested.
Contributing to left ventricular failure and pulmonary oedema. |
|
|
|
Define hypertension?
|
Hypertension exist if Diastolic pressure is greater than 95mmHg
|
|
|
|
4 properties of cardiac muscle?
|
1. Excitability
The cells ability of being responsive to a stimuli. 2. Automaticity The capability for self depolarization. 3. Conductivity A cells ability to conduct an impulse from one cell to another. 4. Contractility The ability to shorten or develop tension |
|
|
|
Intrinsic depolarisation rates of the SA node, AV node & Ventricular Cells?
|
SA node 60-80 per minute
AV node 40-60 per minute Ventricular cells 15-40 per minute |
|
|
|
Briefly describe all elements of
The Cardiac Cycle? |
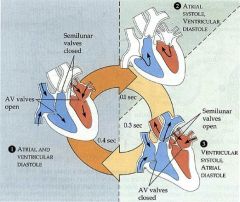
Section 1 - Atria and ventricles are both resting (passively filling)
Section 2 - Atria contract, ventricles still resting Discuss atrial kick (30% of ventricular filling) - the priming force contributed by atrial contraction immediately before ventricular systole, that acts to increase the efficiency of ventricular ejection due to acutely increased preload Section 3 - Ventricles contracting, atria resting (passively filling) |
|
|
|
How long does Atrial systole/diastole & Ventricular systole/diastole last?
|
0.1 sec Atria systole
0.3 sec Ventricular systole 0.7 sec Atria diastole 0.5 sec ventricular diastole |
|
|
|
Three important functions of the ventricular diastole?
|
Ventricular Filling
Ventricular Resting Ventricular Perfusion |
|
|
|
The dangers of sustained tachycardias with reference to the 3 important occurrences of diastole?
|
Cardiac cycle time is reduced to a tachycardia.
Reduced Ventricular filling time, reduced preload, reduced cardiac output. Reduced Ventricular resting time, reduced strength, reduced contractility, reduced cardiac output. Reduced ventricular perfusion, increased ischaemia and pain, reduced contractility, reduced cadiac output. |
|
|
|
The primary function of ventricular systole?
|
Contraction of the ventricles, forcing blood into the aorta and pulmonary arteries
|
|
|
|
The starling mechanism?
How can this mechanism be compromised or enhanced by pathophysiology factors and paramedic interventions? |
The greater the myocardium is stretched , the greater the force of it's contraction to a point.
|
|
|
|
Define Preload?
|
The tension in a chamber of the heart at the end of diastole.
Just befor it is about to contract. |
|
|
|
Define After-Load?
|
After-Load is the pressure against which the heart must pump.
It is a result of peripheral vascular resistance. If referring to left and right ventricular after-load, we are talking about diastolic pressure in the aorta and pulmonary artery respectively. |
|
|
|
The main parasympathetic nerve that controls the heart?
|
Through the Vagus nerve.
The 10th cranial nerve As a continuous restraining influence on the heart. |
|
|
|
The main sympathetic nerves that control heart rate?
|
Nerve fibres called ganglia, originating in the thoracic region of the spinal cord.
|
|
|
|
Function of the cardiac skeleton?
|
The fibrous or fibrocartliaginous framework that supports and gives attachment to the cardiac muscle fibres and valves, and the roots or the aorta and pulmonary trunk.
|
|
|
|
Factors that may compromise coronary perfusion?
|
Heart Rate (tachycardia)
Collateral circulation Electrical disturbances (VT,VF,PVC's) Ischaemia from coronary vessel occlusion |
|
|
|
Explain the term 'functional syncytium' as it applies to the heart's conductive system
|
Syn (with or together)
+ cyt (cell) + ium (biological structure) The atria make up one syncytium while the ventricles make up the other. |
Cardiac muscle cells are mechanically, chemically, and electrically connected to one another, thus, the entire tissue resembles a single, enormous muscle cell. For this reason, cardiac
muscle has been called a functional syncytium. This is also true of smooth muscle. |
|
|
The cardiac haemodynamic problems often associated with bradycardias?
|
Bradycardia can be a serious problem if the heart doesn't pump enough oxygen-rich blood to the bodies vital organs.
Reduced filling pressure = reduced stroke volume and essentially Cardiac output. |
|

