![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
65 Cards in this Set
- Front
- Back
|
Pulmonary Circulation
|
Right heart pumps deoxygenated blood through the lungs where it becomes oxygenated.
|
|
|
Systemic Circulation
|
Left heart pumps oxygenated blood through the body
|
|
|
Follow a drop of deoxygenated blood from the capillaries to the lungs
|
venules of organs, veins of organs, vena cava, right atrium, right av valve, right ventricle, pulmonary semilunar valve, pulmonary arteries, lungs
|
|
|
Follow a drop of oxygenated blood from the lungs to the capillaries
|
pulmonary vein, left atrium, left av valve, left ventricle, aortic semilunar valve, aorta, arteries of each organ, arterioles of each organ
|
|
|
Pericardium
|
Sac that surrounds and protects the heart
|
|
|
Mediastinum
|
contains all of the thoracic viscera except the lungs
|
|
|
Myocardium
|
cardiac muscle cells
|
|
|
Endocardium
|
Innermost layer of tissue that lines the chambers of the heart
|
|
|
Name the two atrioventricular valves
|
Tricuspid Valve
Mitral/Bicuspid Valve |
|
|
Name the two semilunar valves
|
Pulmonic Valve
Aortic Valve |
|
|
Papillary muscles
|
prevent the valve leaflets from bending backwards into the atria during ventricular contractions
|
|
|
What is the period of ventricular contractions called?
|
systole
|
|
|
What is the period of ventricular relaxation called?
|
diastole
|
|
|
S1 is caused by
|
Closure of the AV valves
|
|
|
S2 is caused by
|
Closure of the semilunar valves
|
|
|
Isolvolumic Contraction
|
volume remains constant during this phase
|
|
|
ventricular ejection
|
contraction results in a rapid rise in ventricular pressure forces the aortic valve to open with a rapid ejection of blood.
|
|
|
stroke volume (SV)
|
the amount of blood ejected with contraction of the ventricle
|
|
|
end diastolic volume (EDV)
|
the volume of blood in the ventricle prior to ejection
|
|
|
end systolic volume (ESV)
|
the amount of blood that remains in the ventricles after ejection
|
|
|
ejection fraction=?
|
SV/EDV
|
|
|
isovolumic relaxation
|
begins with SL valve closure in response to falling ventricular pressure and ends when AV valves opens to allow to ventricular filling, ventricular blood volume remains constant during this phase
|
|
|
left anterior descending (LAD) coronary artery
|
supplies septum, anterior of the heart and apex
|
|
|
left circumflex coronary artery
|
supplies left atria and the lateral and posterior left ventricle. in 45% it supplies SA node
|
|
|
right posterior descending coronary artery
|
supplies the left inferior surface of the right and left ventricles
|
|
|
marginal right coronary arteries
|
supplies the right atrium and right ventricles. in 55% of people it supplies the SA node
|
|
|
Ohm's law
|
An increase in driving pressure increases flow, while an increase in resistance reduces flow
P= ABP-RAP |
|
|
Coronary driving pressure
|
equals aortic blood pressure minus right atrial pressure
|
|
|
working cardiac myocytes
|
mechanical pumping function
|
|
|
electric cardiac myocytes
|
transmit electrical impulses
|
|
|
__________ activity always precedes the __________event
|
electrical, mechanical
|
|
|
SA node
|
the primary pace maker
|
|
|
AV node
|
delays impulse and conducts to bundle of His
|
|
|
Bundle of His
|
the brief delay at the AV node allows for the atrial kick
|
|
|
purkinje fibers
|
electrical fibers
|
|
|
What are the 5 electrophysiologic properties of all myocardial cells?
|
1. automaticity
2. excitability 3. conductivity 4. contractility 5. refractoriness |
|
|
propagation of cardiac action potentials
|
membrane potential, depolarization, repolarization, refractory period
|
|
|
Phase 0
|
rapid depolarization
Na+ rapidly in K+ out Ca++ slowly in |
|
|
Phase 1
|
early rapid depolarization
Na+ channels partially close Cl- in K+ out |
|
|
Phase 2
|
plateau
Ca++ slowly in K+ slowly out |
|
|
Phase 3
|
final rapid repolarization
K+ quickly out Na+ and Ca++ channels close |
|
|
Phase 4
|
resting membrane potential
Na+/K+ pump= Na+ out, K+ in Ca+ out |
|
|
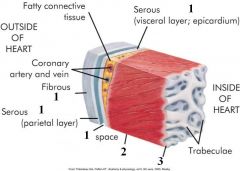
1- pericardium
2- myocardium 3- endocardium |
|

|
1: Diastole
2: Systole |
|

|
1: AV
2: SL |
|

|
1: SA Node
2: AV Node 3: Bundle of His 4: purkinje fibers |
|

|
P= atrial depolarization
PR interval= time for impulse to spread through the atria QRS complex= ventricle (R&L) depolarization T wave= ventricular repolarization ST segment= early part of repolarization of the right ventricles |
|

|
1. intercalated disk
2. sarcomere 3. sarcolemma 4. myofibril 5. mitochondria 6. |
|

|
0. rapid depolarization
1. early rapid repolarization 2. plateau 3. final rapid repolarization 4. resting membrane potential |
|
|
cardiac intervention
|
sympathetic nerves
parasympathetic nerves |
|
|
adrenergic receptor function
|
beta-adrenergic repectors
norepinephrine or epinephrine |
|
|
contractile apparatuses are formed from________&___________ and collectively make up___________
|
actin and myosin, sarcomeres
|
|
|
sliding filament/cross-bridge theory of muscle contraction
|
contraction of cardiac muscle by shortening or individual sarcomeres due to increased overlap of actin and myosin filaments
|
|
|
role of calcium in muscle contraction?
|
-contraction is dependent on adequate calcium ions in the cytoplasm
-muscle relaxation is due to removal of calcium from the cytoplasm |
|
|
SR calcium pumps (SERCAs) require
|
ATP!
|
|
|
preload
|
left ventricular end-diastolic volume
|
|
|
afterload
|
load muscle must move after it starts to contract
|
|
|
cardiac output
|
volume of blood ejected by each ventricle per minute (Average= 5L/min)
|
|
|
cardiac index
|
cardiac output divided by BSA (Average= 2.5-4.0L/min/m2 BSA)
|
|
|
stroke volume
|
volume ejected by each ventricle per beat.
dependent on: contractility, preload, afterload) |
|
|
ejection fraction
|
portion of blood ejected during systole (about 2/3 of the volume in the ventricle at the end of diastole)
|
|
|
what three factors is contractility dependent on?
|
1. amount of contractile proteins in the muscle cell
2. availability of ATP 3. availability free calcium ions in cytoplasm. |
|
|
Cardiovascular changes in the elderly
|
valves- become stiff
conduction- decreased LV- increased in size, noncompliant aorta- thick, stiff, less distensible |
|
|
what three factors is contractility dependent on?
|
1. amount of contractile proteins in the muscle cell
2. availability of ATP 3. availability free calcium ions in cytoplasm. |
|
|
Cardiovascular changes in the elderly
|
valves- become stiff
conduction- decreased LV- increased in size, noncompliant aorta- thick, stiff, less distensible |

