![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
140 Cards in this Set
- Front
- Back
|
What is the most common symptom that causes pts to seek medical care?
|
Chest pain
|
|
|
What is the cardinal manifestation of myocardial ischemia?
|
Chest pain
|
|
|
What is the chest pain of chronic stable angina described as?
|
Pressure-like or squeezing discomfort that is located behind the sternum or precordially
|
|
|
What is the pain from chronic stable angina precipitated by? when will it resolve?
|
precipitated by exertion or emotional upset and may resolve spontaneously w/in 15 minutes or following the administration of sublingual nitroglycerin
|
|
|
What is the pattern of pain seen in chronic stable angina? what is the intensity of pain?
|
Discomfort/pain may radiate to the jaw and/or along the ulnar nerve innervation of the left arm, the intensity is variable but less severe than the pain experienced during a MI
|
|
|
A pt walks into your clinic. When you ask him what brought him in that day he says he felt a pressure-like or squeezing discomfort behind his sternum that radiated to his jaw and left arm when his daughter told him she was engaged and her fiance had not asked the father's permission. After asking how long the pain lasted he said it resolved w/in 15 minutes. What's the dx?
|
Chronic stable angina
|
|
|
What is the difference in chest pain b/e chronic stable angina and a MI?
|
Although they have similar patterns pain from a MI is much more intense and prolonged, lasting as long as 30 minutes and is NOT RELIEVED BY ADMINISTRATION OF NITROGLYCERIN
|
|
|
How is the pain from a MI typically characterized?
|

As crushing or vise-like like a whale is sitting on your chest and has associated symptoms (nausea, diaphoresis, severe anxiety and shortness of breath)
|
|
|
How can you distinguish a MI from chronic stable angina?
|
An MI's pain is more intense, lasts longer and is NOT relieved by administering sublingual nitroglycerin. The pain is crushing/vise-like and is accompanied w/ associated symptoms like nausea, diaphoresis (excessive sweating), severe anxiety and shortness of breath
|
|
|
What are the most common causes of chest pain?
|
Non-cardiac conditions
|
|
|
What is costochondritis?
|
An inflammatory condition that produces anterior chest pain similar in quality to angina pectoris
|
|
|
When is the pain from costochondritis worse? how can you reproduce the pain?
|
During inspiration and movement; you can reproduce the pain by applying firm pressure over the inflamed costochondral junctions
|
|
|
What is reflux esophagitis? what is the pain pattern?
|

"Heart burn"
Retrosternal chest pain that is caused by reflux of esophageal contents into the esophagus that irritates the lining |
|
|
What is pain from reflux esophagitis described as? what precipitates the pain? what relieves pain?
|
Pressure-like or burning that is precipitated by a large meal; pain is relieved by antacids
|
|
|
What is Pleuritic chest pain?
|
Inflammation of the pleura
|
|
|
What is pain from pleuritic chest pain described as? what improves the pain? what worses the pain?
|
An intense pain that is made worse by deep breathing and improved by holding the breath
|
|
|
What accompanies pleuritic chest pain?
|
fever, cough and shortness of breath
|
|
|
What are the common causes of pleuritic chest pain?
|
Pneumonia and pulmonary infarction
|
|
|
A patient comes into your clinic. During the examination he describes a intense vise-like retrosternal pain that lasted for ~30minutes. He also describes that the pain was so intense it made him nauseous, he sweated intensely and was short of breath. The pain was not relieved following administration of nitroglycerin. What's the dx?
|
Myocardial infarction
|
|
|
A pt walks into your clinic. During the examination he describes a chest pain that intensified when he inspired and when he moved. During your physical examination you press firmly over the constochondral junctions and the patient yells in pain. What's the dx?
|
Constochondritis
|
|
|
A patient walks into your clinic. During the examination she describes a retrosternal burning chest pain after eating a large meal. What's the dx?
|
Reflux esophagitis
|
|
|
A patient walks into your clinic. During the examination the pt describes a pleuritic pain that intensifies when she inspires deeply but improves when she holds her breath. After the meeting you read in her chart that she recently had pneumonia. What's the dx?
|
Pleuritic chest pain
|
|
|
What is acute dyspnea manifested in?
|
Can be either a manifestation of cardiac dz or pulmonary dz
|
|
|
What typically causes subacute/chronic dyspnea?
|
Chronic lung dz
|
|
|
What is the most common cardiac cause of subacute/chronic dyspnea?
|
Congestive heart failure from systolic/diastolic dysfunction
|
|
|
What is orthopnea? How do pts relieve this symptom?
|
Dyspnea that develops after assuming a recumbent position, pts usually sleep sitting upright in a chair
|
|
|
What quantifies the severity of orthopnea?
|
The number of pillows the pt sleeps on at night
|
|
|
What is paroxysmal nocturnal dyspnea? (PND)
|
The sudden onset of dyspnea during sleep. Pts suddenly awaken completely out of breath
|
|
|
What respiratory symptom is more specific for cardiac problems than respiratory problems?
|
Paroxysmal Nocturnal Dyspnea
|
|
|
What are palpitations?
|
A sensation that patients have when they suddenly become aware of an irregularity or abnormality in their own heart beat
|
|
|
What dz'es do palpitations indicate?
|
May indicate nothing more than anxiety or caffeine sensitivity but may ALSO indicate serious underlying heart dz such as myocardial ischemia or life-threatening conduction disturbances
|
|
|
What non-cardiac symptoms indicate coronary artery dz?
|
Physical signs of hyperlipidemia including xanthelasma, cutaneous and tendon xanthomas and (possibly) corneal arcus in young adults
|
|
|
What do nicotine stained fingernails indicate? what is this a major risk factor for?
|
Indicate a hx of cigarette smoking which is a known risk factor for coronary artery dz
|
|
|
What is obesity a strong risk factor for?
|
coronary artery dz
|
|
|
What do diagonal ear lobe creases indicate?
|
Associated w/ coronary artery dz
|
|
|
What is cyanosis? what does it indicate?
|

A blue discoloration of the nail beds and mucous membranes that may indicate a right-left intracardiac shunt through a atrial or ventricular septal defect in the presence of pulmonary HTN
|
|
|
What is differential cyanosis? what does it indicate?
|
Cyanosis of the toes sparing the fingers; indicates pulmonary HTN and right->left shunting through a patent ductus arteriosus distal to subclavian artery
|
|
|
What is reverse differential cyanosis? when does it occur?
|
Cyanosis of the fingers w/ sparing of the toes, occurs in transposition of the great arteries in association w/ a patent ductus arteriosus and pulmonary HTN
|
|
|
What causes digital clubbing? what dz commonly causes this?
|
occurs in pulmonary/cardiac dz'es where venous blood mixes w/ arterial blood. Commonly caused by congenital heart dz associated w/ right->left intracardiac shunt
|
|
|
What cardiac abnormality is Marfan's syndrome associated with? what hand/wrist sign do these pts exhibit?
|
A thoracic aortic aneurysm and aortic regurgitation, pt's w/ marfan's have a positive thumb and wrist sign
|
|
|
What cardiac abnormality are hyperextensible joints associated with? what dz are these symptoms associated with?
|
Associated w/ mitral valve prolapse, these abnormalities are features of Ehlers-Danlose syndrome
|
|
|
What are delayed pulse and diminished BP in the legs features of?
|
Coarctation of the Aorta
|
|
|
What are Roth's spots, Osler's nodes and Janeway's lesions indicative of?
|
The presence of infectious endocarditis
|
|
|
What causes Angina?
|
Chest pain caused by the heart not getting enough oxygen, so basically angina is when your heart gets a cramp.
|
|
|
Why is pain poorly localized when it concerns the organs?
|
B/c it is visceral pain which has a poorly localized distribution of pain
|
|
|
What causes differential clubbing?
|
A patent ductus arteriosus (PDA) that causes megakaryocytes to get stuck in distal capillaries. When they get stuck in the capillaries they release growth factors, so b/c the PDA is distal to the left subclavian the fingers are normal but the toes have clubbing
|
|
|
What are conjunctival petechiae? what do they indicate?
|

Petechiae in the conjunctiva of the heart, indicate heart valve misfunction so listen for murmurs
|
|
|
What are janeway lesions indicative of? osler's lesions?
|
Heart valve infection
|
|

What is a roth spot? what does it indicate classically?
|
endocarditis (heart infection)
|
|
|
What bundle branch depolarizes first?
|
The left bundle depolarizes first; so LV contracts first also -> this also causes the mitral valve to close first
|
|
|
Which valve opens first the pulmonic or aortic? why?
|
The pulmonic valve opens first b/c the isovolemic contractio phase is shorter due to the lower pressure in pulmonary artery
|
|
|
Which valve closes first pulmonic or aortic? which ventricle finishes ejecting first?
|
Aortic valve closes first and LV ventricle finishes ejecting first
|
|
|
Which valve opens first, mitral or tricuspid?
|
Tricuspid valve opens first
|
|
|
What is the normal central venous pressure?
|
4-7mmHg
|
|
|
What is the normal right ventricle pressure?
|
Sys: 15-30mmHg
Dias: 0-7mmHg |
|
|
What is the normal left atrial filling pressure?
|
4-12mmHg
|
|
|
What is the normal left ventricular pressure?
|
Sys: 90-120mmHg
Dias: 4-12mmHg |
|
|
What is the normal pulmonary artery pressure?
|
Sys: 15-30mmHg
Dias: 8-15mmHg |
|
|
What is the normal aortic pressure?
|
Systolic: 90-120mmHg
Diastolic: 60-80mmHg |
|
|
What ventricle is activated first electrically?
|
Left ventricle
|
|
|
What ventricle begins rapid ejection first? why?
|
Right ventricle b/c it has a much lower afterload to overcome
|
|
|
What is the order of valves opening and closing in systole?
|
1. mitral valve closes; b/c left ventricle is activated electrically first
2. tricuspid valve closes 3. pulmonic valve opens; b/c right ventricle has lower afterload to overcome 4. aortic valve opens |
|
|
What is the order of valves closing and opening in diastole?
|
1. aortic valve closes
2. pulmonic valve closes 3. tricuspid valve opens 4. mitral valve opens |
|
|
What happens to the time spent in systole and diastole as the HR increases?
|
the relative proportion of time spent in diastole compared to the time spent in systole decreases
|
|
|
What are the reasons to examine jugular venous pulsations?
|
1. determining the amount of central venous pressure
2. evaluating the mechanical events in the right atrium and ventricle |
|
|
What is the chief determinant of RV preload?
|
central venous pressure
|
|
|
What is the central venous pressure?
|
The mean right atrial pressure that, in the absence of tricuspid stenosis equals RV EDP
|
|
|
How can CVP be measured during a physical exam?
|
By the Jugular venous pressure
|
|
|
What is the JVP?
|
The vertical distance in centimeters b/e the mid right atrium and the top of the jugular venous column of blood in the neck
|
|
|
What is used to determine the mid right atrium during the physical exam?
|
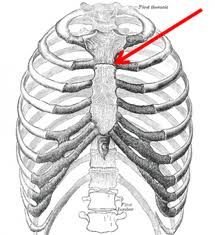
The sternal angle of louis
|
|
|
What causes the JVP to vary?
|
Body position, there is considerable variability in the JVP based on body position
|
|
|
Why is the top of the venous column not visible in adults when they are sitting upright?
|
B/c the JVP is only 4-7 cm H2O
|
|
|
What happens to JVP when the top of the venous column is >3cm above the sternal angle of louis?
|
The JVP is abnormally elevated
|
|
|
What should be used to determine JVP?
|
The right internal jugular vein
|
|
|
Why is the right internal jugular vein not immediately visible grossly? how must venous pressure be inferred?
|
B/c the right internal jugular vein is deep to the SCM, so venous pressure must be inferred from the surface movements of the SCM
|
|
|
What does an elevated JVP increase the likelihood of in the absence of tricuspid stenosis?
|
increases the likelihood that right ventricular filling pressure (RV EDP) is elevated
|
|
|
What is the most common cause of elevated RVEDP?
|
right ventricular failure due to left ventricular failure or chronic lung dz
|
|
|
What does an elevated JVP in the presence of pitting edema imply?
|
That either heart failure or chronic lung dz is responsible for the ankle edema
|
|
|
What should be used to assess jugular pulse waveforms?
|
Right internal jugular vein
|
|
|
What do the waveforms of the jugular venous pulse tracing reflect?
|
Mechanical events in the right atrium and ventricle
|
|
|
What produces the "a" wave in a JVP?
|
atrial contraction in late diastole
|
|
|
What does the "a" wave of the JVP correspond to on the EKG?
|
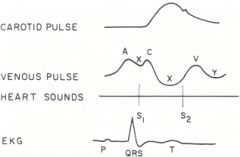
The "a" wave follows the P wave of the EKG and peaks just before the 1st heart sound
|
|
|
What is the x descent? what causes it?
|
A composite of an early x descent produced by right atrial relaxation? and a later x descent produced by movement of the tricuspid valve cusps into the RV during RV ejection
|
|
|
When does the x' descent occur?
|
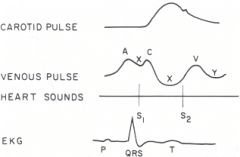
occurs during ventricular systole and ends just prior to the 2nd heart sound
|
|
|
When does systolic collapse of the JVP occur?
|
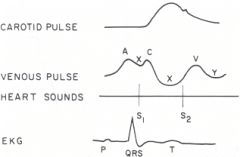
During the x' descent, at the same time the carotid pulsation is moving outward
|
|
|
What produces the v-wave on a JVP?
|
Produced by right atrial filling when the tricuspid valve is closed during isovolumetric contraction
|
|
|
When does the v-wave begin and end?
|
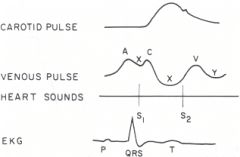
begins just prior to the 2nd heart sound and ends just immediately after the 2nd heart sound
|
|
|
What produces the y-descent?
|
tricuspid valve opening during the filling phase of ventricular diastole
|
|
|
What heart sound does the y-descent correspond to?
|
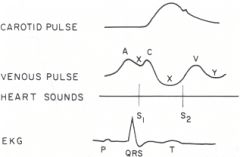
y-descent occurs immediately after the second heart sound
|
|
|
What generates the diastolic collapse of the venous pulsation?
|
The "y"-descent; which is caused by tricuspid valve opening during ventricular filling
|
|
|
When do giant "a" waves occur?
|
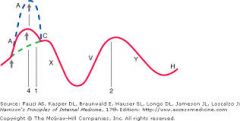
When there is increased resistance to right atrial emptying
|
|
|
When do giant 'a' waves commonly occur?
|
1. tricuspid stenosis
2. right ventricular hypertrophy 3. pulmonary hypertension 4. pulmonic stenosis |
|
|
When do cannon 'a' waves occur?
|
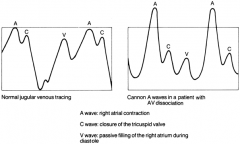
When right atrial contraction occurs simultaneously w/ right ventricular contraction, BUT the tricuspid valve is closed so the full force of atrial contraction is directed upward into the jugular veins
|
|
|
When do cannon 'a' waves occur during cardiac rhythm?
|
They are systolic in timing and occur intermittenly
|
|
|
What do cannon a waves indicate the presence of when arterial pulse is regular?
|
The presence of atrioventricular dissociation due to 3rd degree heart block or ventricular tachycardia
|
|
|
If arterial pulse is irregular what do cannon a waves indicate the presence of?
|
premature ventricular contractions (PVCs)
|
|
|
When do cannon a waves occur in patients w/ premature ventricular contractions?
|
When the PVC coincides w/ a atrial contraction
|
|
|
What would show up on a JVP tracing if there is no atrial contraction?
|
An absence of the a wave
|
|
|
What is the most common cause for absence of the a wave on a JVP?
|
atrial fibrillation
|
|
|
How would atrial fibrillation show up on a JVP tracing?
|
As an absence of the a wave
|
|
|
What causes a giant v wave?
|
Produced when the RV volume is ejected into the right atrium during tricuspid regurgitation
|
|
|
What do giant v waves occur with?
|
Occur regularly and synchronously w/ the carotid pulse and are much larger than normal a and v waves
|
|
|
what effect do giant v waves have on jugular pulse?
|
Giant v waves produce a systolic pulsation of the jugular pulse
|
|
|
How can you tell whether a v wave is severe, moderate, mild or normal?
|
The larger the size of the v wave the more severe the condition
|
|
|
What does a slow y descent shortly after the 2nd heart sound indicate?
|
Obstruction to right atrial emptying, characteristic of tricuspid stenosis
|
|
|
What is a slow y descent shortly after the 2nd heart sound characteristic of?
|
tricuspid stenosis
|
|
|
When does a rapid y descent occur?
|
in obstructive pericarditis
|
|
|
What is recognized as a prominent collapse of the venous pulse?
|
A rapid y descent caused by obstructive pericarditis
|
|
|
What effect does inspiration have on venous return? what affect does this have on JVP?
|
inspiration increases venous return, so as a result blood is siphoned away from the jugular veins during inspiration and JVP decreases
|
|
|
What is a kussmaul sign?
|
A paradoxical increase in jugular venous pressure that occurs during inspiration
|
|
|
When does the kussmaul sign develop?
|
Whenever the right atrium and right ventricle are unable to expand to accommodate the increase in venous return that occurs during inspiration
|
|
|
What conditions cause kussmaul signs?
|
Occurs in constrictive pericarditis, restrictive cardiomyopathy, RV failure, RV infarction and tricuspid stenosis
|
|
|
Does kussmaul sign occur in cardiac tamponade?
|
Nope
|
|
|
How do you perform the abdominojugular test (AJT)?
|
By applying firm pressure (25-35mmHg) w/ the flat of the hand to the mid-abdomen for 10 seconds. The firm pressure increases venous return to the heart and briefly increases JVP. However, the JVP returns to normal in 2-3 seconds even though the abdominal pressure is continued for 10 seconds
|
|
|
What is a positive abdominojugular test (AJT)?
|
When abdominal compression causes a sustained increase in JVP of 4cm H2O for as long as abdominal compression is maintained
|
|
|
What does a positive AJT indicate?
|
that the right atrium and/or right ventricle are incapable of expanding in response to increased venous return
|
|
|
What pathologies cause a positive AJT?
|
RV infarction, RV hypertrophy, tricuspid regurgitation and constrictive pericarditis
|
|
|
How could LV failure cause a positive AJT?
|
When LVEDP is > 15mmHg. LV failure causes increased sympathetic activity which decreases venous compliance, so abdominal compression forces blood into the non-compliant venous system and causes a sustained increase in JVP for as long as compression is maintained
|
|
|
What does a positive AJT in the presence of dyspnea indicate?
|
That left ventricular failure is most likely responsible for the dyspnea/positive AJT
|
|
|
What does a negative AJT in the presence of dyspnea indicate?
|
That a non-cardiac problem is most likely responsible for the dyspnea
|
|
|
What is precordial palpation used for?
|
Used to assess cardiac motion transmitted to the chest wall
|
|
|
What is the apical impulse?
|
The cardiac impulse that is palpable farthest to the left of the sternum
|
|
|
What produces the apical impulse?
|
Produced by anterior and counter-clockwise movement of the anterior wall of the left ventricle against the inner chest wall.
|
|
|
When should the apical impulse be assessed?
|

When the patient is supine and when the pt is turned into a left lateral decubitus position
|
|
|
What are the dimensions of a normal apical impulse?
|
1. roughly the size of a dime
2. confined to 5th intercostal space 3. located medial to the midclavicular line 4. occurs synchronously w/ S1; moves outward during the first third of systole and precedes the carotid pulsation |
|
|
When does concentric ventricular hypertrophy occur?
|
When a ventricle is required to pump against an excessively high pressure (pressure overload)
|
|
|
What pathology can be caused by pressure overload?
|
concentric ventricular hypertrophy
|
|
|
What kind of pathology are aortic stenosis and systematic hypertension?
|
Pressure overload conditions that can lead to left ventricular hypertrophy
|
|
|
What are the features of a sustained apical pulse?
|
1. <3cm in size and confined to 1 or 2 intercostal spaces (so not that different from normal)
2. located medial to the midclavicular line or at the midclavicular line 3. peaks in 2nd half of systole and may not retract until after S2 4. occurs synchronously w/ the carotid pulsation 5. amplitude is normal or slightly increased |
|
|
What is the most diagnostic feature of a sustained apical pulse?
|
The long duration of the pulse and the fact that it peaks at S2-ish rather than S1-ish
|
|
|
When do ventricular dilation and eccentric hypertrophy develop?
|
When a ventricle is required to eject a larger volume of blood than normal (volume overload)
|
|
|
What genre of impulse deficit do chronic aortic regurgitation and chronic mitral regurgitation fall under?
|
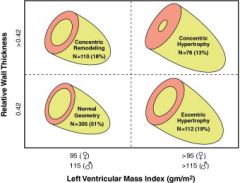
volume overload conditions that cause ventricular dilation and eccentric hypertrophy
|
|
|
What is the apical impulse that is caused by ventricular dilation and eccentric hypertrophy?
|
Hyperdynamic (thrust)
|
|
|
What are the characteristics of hyperdynamic (thrust) apical impulses?
|
1. 4-5cm in size and confined to 2 or more intercostal spaces (much larger than normal)
2. located LATERAL to midclavicular line 3. begins at S1 and retracts by the middle half of S1 (mostly normal) 4. occurs synchronously w/ carotid pulse 5. has an increased amplitude and force that is difficult to obliterate w/ applied pressure |
|
|
What happens to the apical impulse when the pt is in the left later decubitus position?
|
It moves the apical impulse laterally by 1-5 cm
|
|
|
What does a sustained apical impulse in the left lateral decubitus position indicate?
|
Still indicates the presence of concentric LV hypertrophy
|
|
|
What does an apical impulse in the left lateral decubitus position that is >4cm in size indicate?
|
LV dilation
|
|
|
What is RV pressure overload?
|
produces an outward impulse just to the left of the sternum that occurs roughly at the same time as the apical impulse
|
|
|
What is RV volume overload?
|
generates a hyperdynamic, high amplitude impulse along the lower left sternal border or at the xiphoid
|
|
|
What is a thrill?
|
Loud murmurs that are palpable on the chest wall
|

