![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
22 Cards in this Set
- Front
- Back
|
How much calcium is there in the body?
Where is it distributed? |
25000 mmol (1kg)
99% is in mineral phase in bone (mechanical strength) Much higher conc outside cell extracellular ionised Ca ~1.2 mmol/L Intracellular cytosolic 10-4 - 10-3 mmol/L |
|
|
What biological roles does calcium have?
|
Biological roles:
muscle contraction intracellular messenger nerve excitability blood coagulation enzymes of metabolism |
|
|
How is calcium distributed in serum?
|
47% free (unbound/ionised)
47% bound to albumin 6% complexed Note: Feedback mechanisms are regulated by the free fraction Normal 2.2-2.6 mmol/L |
|
|
How is serum calcium measured?
|
We can measure either:
-free calcium -total calcium (bound+free) If a patient has a low albumin concentration, TOTAL [Calcium] will also be low but the FREE [Calcium] may be normal In practise we measure total calcium (what serum total calcium would have been if the albumin had been normal) Ca (adj) = Ca(tot) + [0.02(45-alb)] |
|
|
How is calcium homeostatis maintained (organs and hormones)?
|
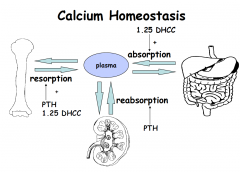
Main organs involved
–kidney –gut –bone –parathyroid glands (calcium sensing receptors) Metabolic control – main hormones –parathyroid hormone (PTH) - resorption and reabsorption –1,25 dihydroxyvitamin D (AKA dihydroxycholecalciferol - 1.25DHCC or calcitriol) - absorption |
|
|
How much calcium is needed in the diet?
|
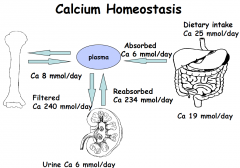
25mmol/day of which 6mmol is absorbed
|
|
|
Where is calcium absorbed along the GIT?
|
Mainly in duodenum and jejenum by two mechanisms
-cell mediated active transport controlled by 1.25 DHCC -passive diffusion depending on Ca conc Proportion of ingested Ca absorbed varies from 20-60% 1.25DHCC increases fractional absorption -if dietary intake falls -during growth, pregnancy and lactation |
|
|
What happens to calcium in the kidney?
|
65 % reabsorbed in proximal tubule - coupled to bulk transport of solutes such as Na and water
Increased by PTH: -20% reabsorbed in cortical thick ascending loop of Henle -15% in DCT |
|
|
What is PTH and from where is it released?
|
84 AA polypeptide produced by parathyroid glands
-Secretion regulated by FREE calcium sensed by calcium sensing receptors on parathyroid cells (quick response) -Main ligand is calcium -Serve as calciostat for calcium homeostasis -As Ca increases PTH decreases, as Ca decreases PTH increases |
|
|
Where are calcium sensing receptors found in the body?
|
-G protein coupled receptor found in:
-parathyroid cells - mediates effects of EC ionised Ca on PTH release -Renal tubule - mediates effect of high peritubular ionised [Ca] to inhibit Ca reabsorption Activators used clinically to reduce PTH secretion in patients with renal failure and parathyroid cancer Disorders of this receptor can produce abnormalities in serum calcium concentrations |
|
|
What is the relationship between ionised Ca and PTH?
|

Steep, inverse sigmoidal curve
•Small change in iCa causes significant change in PTH •Midpoint gives sensitivity of parathyroid gland (CSR) to iCa •Disorders of the CSR recognised. |
|
|
What are the effects of PTH?
|
•Stimulates renal tubular calcium REABSORPTION
•Promotes bone RESORPTION •Stimulates formation of 1,25 DHCC in kidney, which enhances calcium ABSORPTION from gut |
|
|
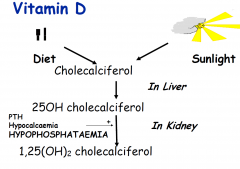
How is vitamin D synthesised
|
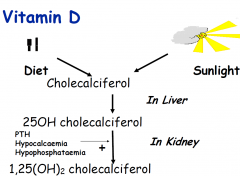
?
|
|
|
What are two major causes of hypocalcaemia?
|
PTH problem
–Hypoparathyroidism – neck surgery, idiopathic, magnesium deficiency Vitamin D problem –Deficiency – malabsorption, little exposure to sunlight –Renal disease – kidneys fail to make the active form DHCC |
|
|
What are two major causes of hypercalcaemia?
|
PTH problem
–Hyperparathyroidism – adenoma of parathyroid gland –Calcium increase and PTH increase Malignancy – PTH related peptide – lung cancer, breast cancer, multiple myeloma –Calcium increase and PTH suppressed Vitamin D problem –Inappropriate dosage |
|
|
Why does the body require phosphate?
|
skeletal development and bone mineralisation
Composition of cell membranes, nucleotide structure, cell signalling |
|
|
Where is phosphate located in the body?
|
85% of total body PO4 mineralised matrix of bone
•Rest predominantly intracellular – bound to lipids and proteins – organic –Cell membranes, nucleic acids, enzyme cofactors, glycolytic intermediates, ATP •Only 1% in EC fluids - 30% is inorganic – routinely measured |
|
|
Phosphate transport in/out of cells
|
Phosphate shifts between organic phosphate pool and inorganic pool
Phosphate shifts in and out of cells e.g. Insulin-mediated entry of glucose into cells after meals results in phosphate shifting into cells So serum [PO4] # true PO4 stores |
|
|
What are the main organs involved in phosphate homeostasis?
|
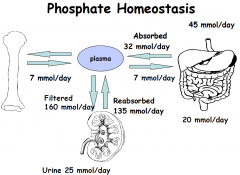
Kidney
Gut Bone |
|
|
What are the main hormones involved in phosphate homeostasis?
|
–Parathyroid hormone (PTH)
–Fibroblast Growth Factor 23 (FGF 23) –1.25 dihydroxyvitamin D (1.25DHCC) •ABSORPTION in intestine less rigidly regulated than Ca – entire small intestine – increased by 1.25 DHCC •Plentiful in diet |
|
|
What is the role of the kidney in phosphate homeostasis?
|
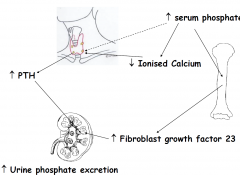
•15-20% phosphate is protein bound, rest filtered by kidney
•75% of filtered phosphate is reabsorbed in PCT and 5-20% in DCT •PTH and FGF23 INHIBIT the reabsorption of phosphate by renal tubule |
|
|
Other points that influence serum phosphate
|
Several factors influence serum values:
•Marked diurnal variation rhythm, nadir before noon, peak after MN - peak to nadir amplitude ~30% •Dietary effects – rises post-prandially then falls due to effect of rise in insulin •Marked age-related changes. Highest values in infancy when growth velocity high |

