![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
56 Cards in this Set
- Front
- Back
|
Infant mortality rate in US in blacks vs overall
|
blacks: 13.4 / 1000 Live Births
overall: 6.78 / 1000 live births disparity in IMR |
|
|
At what age is the highest risk for infant mortality - due to SIDS or due to other
|
SIDS: highest at 1 month, then 2nd peak at 3 months
other: peak at 2 months |
|
|
top 9 causes of death <1 year olds
|
Top 2 are much more common than rest
1) perinatal 36% 2) anomalies 26% 3) SIDS 6% 4) injury 5) infection 6) lung 7) CV 8) GI 9) other |
|
|
Top 10 causes of death in 0-17 yo
|
1) Injury 25%
2) perinatal 22% 3) anomalies 18% 4) SIDS 6% 5) infection 6) lung 7) Neuro 8) CV 9) GI 9) other |
|
|
Definition - Sudden Infant Death Syndrome (SIDS)
|
Sudden infant death syndrome (SIDS) is the sudden death of an infant under one year of age with onset of the fatal episode apparently occurring during sleep
that remains unexplained after the performance of a complete autopsy, examination of the death scene and review of the clinical history. |
|
|
incidence of SIDS
|
incidence has been decreasing over past 20yrs from 2.3 / 1000 (1985) to 0.67 / 1000 (2005)
2,200 infant deaths in 2005 whites consistently higher than blacks |
|
|
classic characteristics of SIDS
|
>1 month but < 6 months (peak 2-4 months)
Previously healthy, no family history Mild upper respiratory tract infection (viral) Death occurs during sleep (midnight - 6 am) Male White Winter (same incidence every day of the week) |
|
|
Maternal Risk Factors Associated With SIDS
|
-Young, unmarried, multiparity
-Lower socioeconomic group, poor, under educated ***Significant association between poverty and SIDS -Poor prenatal care, poor weight gain, anemia -Smoking or drug use during pregnancy -Lack of breast feeding (recently determined to be less important) |
|
|
prenatal care: within the US where are the lowest rates
|
<82% in southern states, Nevada, DC
>90% (best) in North Dakota and mid-eastern states for blacks specifically: <67% in Nevada, New Mexico, Oklahoma, Arkansas, Minnesota, Wisconsin, Penn, West Virginia, DC 76-83% (best): pacific states, central and some north east states |
|
|
Perinatal Risk Factors Associated With SIDS
|
Prematurity, low birth weight, multiples
Monozygous twins > dizygous twins Male African-American or Native American Low Apgar scores, respiratory distress Poor feeding, vomiting or diarrhea Previous SIDS death in sibling |
|
|
Postnatal Risk Factors Associated With SIDS
|
Prone sleeping position
***Especially during first episode of prone sleeping Soft or excessive bedding Hyperthermia or hypothermia No or late immunizations Co-sleeping (adult, larger sibling, multiple) May represent accidental smothering Environmental smoking |
|
|
what sleeping position is risky for SIDS
|
• Prone sleeping — Sleeping on the stomach, which increases the risk of SIDS by as much as 12-fold. Parents are urged to have their babies sleep supine, or on their backs, until they're 1 year old.
|
|
|
Pathogenesis of SIDS?
|
Problems with respiratory control
**Chronic hypoxia/suffocation theory ***Pre and postnatal hypoxia, pulmonary hypoplasia, delayed brain stem development Cardiovascular abnormalities **Arrhythmogenic theory (long QT) Visceral dyskinesis **Spasm/reflux/dysphagia theory Infection **Precocious immune response in presence of hypoxia, abnormal cytokine production (complement and IL-10) It is unlikely that a single etiology is responsible for SIDS. Genetically predisposed infant – plus something else End point – hypoxia, coma, death |
|
|
Theory of chronic hypoxia as cause of SIDS
|
acute hypoxia at birth --> chronic hypoxia inducing physiology or environment --> blunted hypoxic ventilatory response -- transitory hypoxia -- delayed fetal resetting + delayed response to hypercarbia + reduced sensitivity to hypoxia ---> failed auto-resuscitation --> SIDS at 3months
|
|
|
Brainstem hypothesis in SIDS
|
1) genetic factors + environmental --> abnormal medulla (50% of SIDS) = vulnerable infant
2) this causes decreased CO2 sensitivity, arousal deficit, respiratory pattern abnormality, altered BP recovery, altered temperature control, altered airway reflexes ---> convergence of these faulty reflexes - often the critical period or with an exogenous stressor --> SIDS |
|
|
How does the 5HT system in the Medulla work? What happens if there is less 5HT the medulla?
|
1) The baroreceptor in the aortic arch send a signal to the Solitary nucleus in the medulla (via X)
1b) other inputs are from the heart/BP/temperature 2) this causes an efferent signal to diaphragm via Raphe nucleus (5HT) In a case of SIDS: A) Decreased serotonergic receptors: Males have fewer 5-HT1A receptors than females B) Increased serotonergic neurons - make and release serotonin C) Increased number of immature serotonergic neurons D) Insufficient amounts of serotonin transporter protein |
|
|
what's different in HR and RR in SIDS? cry?
|
higher HR ~ 150 (vs 130)
faster respiration with lower volume Higher pitched cry, hyper adductory vocal folds |
|
|
Long-QT Syndrome
|
LQTS affects 1/5,000
6 identified chromosomal loci and 5 cardiac ion channel genes SCN5A accounts for 5-10% of cases Sodium channel gene Mutation found in 2% of SIDS patients Associated with sleep |
|
|
SIDS Recurrence Risk
|
SIDS recurs in only 1-2% of siblings
Twins are at increased risk and have been reported to have simultaneous or subsequent SIDS deaths All familial cases should be thoroughly evaluated for specific etiologies other than SIDS, particularly homicide |
|
|
Autopsy Findings in SIDS
|
No pathology that explains death
Internal exam Petechiae on thymus, pericardium and lungs prominent lymphoid tissue lung congestion and edema blood in heart is liquid bladder is empty No pathology that explains death Microscopic examination: -Retention of fetal fat around adrenal glands --Recent studies have not confirmed increased Hgb F -Increased hematopoiesis in liver -Gliosis in respiratory centers of brain -Thickened pulmonary arteries, edema, hemorrhage -Mild bacterial or viral pneumonia, gastroenteritis Increased neuropeptides produced by pulmonary neuroendocrine cells |
|
|
Apparent Life-Threatening Event (ALTE)
|
ALTE is an episode that is frightening
to an observer and is characterized by some combination of apnea, color change, marked change in muscle tone, choking or gagging. In some instances the observer fears that the infant has died or would have died if there had not been intervention. |
|
|
Clinical - ALTE
|
Incidence 0.5-3%
Rare survivors have neurologic injury 40% will have recurrent episodes 2% will subsequently die Only 1% of SIDS deaths are preceded by an ALTE episode Etiology will be identified in 50-90% of cases |
|
|
Etiology of ALTE
|
Morphologic causes
CNS; malformations, encephalitis, meningitis, IVH Respiratory; infection, aspiration pneumonia, airway obstruction GI; enteritis, gastroesophageal reflux Metabolic; hypoglycemia, hypocalcemia Cardiovascular; malformations, cardiomyopathy Functional causes (may not have pathology) Apnea Gastroesophageal reflux Bradycardia, arrhythmia Seizure disorders |
|
|
Sudden Unexpected Infant Death
|
Refers to an otherwise healthy infant/child who dies of unknown causes and is not otherwise a SIDS case, usually older
Many will be explained by autopsy Those remaining cases will be, cause of death undetermined (unclassified sudden infant death) Manner of death natural, unnatural (accident or homicide [5-10%]) |
|
|
"Natural Causes" of Infant Death
|
Pulmonary lesions (asthma..)
Cardiac problems (myocarditis..) Undiagnosed metabolic abnormalities (CF, diabetes, MCAD deficiency) Acute infections (Waterhouse-Friderichsen syndrome = hemorrhagic adrenalits) Sickle cell crisis Dehydration |
|
|
Fatty Acid Oxidation Abnormalities: which is most common in infants
|
Medium chain acyl CoA dehydrogenase deficiency (MCAD), other forms less common
Normal at birth Acute illness with decreased oral intake results in hypoketotic hypoglycemia, neutral lipid accumulates in liver, steatosis, hepatic encephalopathy and death Autosomal recessive, F>M May account for 4% of sudden unexpected deaths |
|
|
Accidental Infant Death vs Suffocation
|
Accidental Infant Death:
Poisoning Asphyxia Drowning MVA Suicide Suffocation: Suffocation may be accidental or intentional. Suffocation occurs in children less than 3 years of age, most are less than 12 months of age. 2-10% of deaths determined to be SIDS, may be due to suffocation. The autopsy findings in suffocation and SIDS are nearly identical, making scene investigation very important. |
|
|
Neonaticide
|
The risk of homicide on the first day of life is 10x greater than at any other time.
Unwanted or illegitimate birth, the obvious sexual activity, mental illness, difficult relationship with parents, immaturity and a culture that promotes self-destructive impulses 42 states have “safe haven” laws Incidence, 0.002% of all live born male > female black > white 85% committed by the mother 50% single 35% had other children mean age 19 years (14-35 years) 50% no prenatal care, 25% denied being pregnant Asphyxiation/strangulation 41%, drowning 26% |
|
|
“Battered Child Syndrome”
|
50% occur < 3 years, 25% < 1 year but more likely to be fatal
Head injury is leading cause of death, followed by abdominal trauma Occurs during episodes of crying, toilet training, and resentment towards spouse or child |
|
|
“Shaken Baby Syndrome”
|
Violent backward and forward movement of the unsupported head
“Shaken baby impact syndrome” may be even more dangerous as the head is rapidly stopped usually against a solid object--acceleration and deceleration injury Pathology Subdural/subarrachnoid hemorrhage Retinal hemorrhage Increased intraocular pressure transmitted from the intracranial cavity through the optic nerve sheath Shearing injury to vessels Subdural and retinal hemorrhages are much more common in abusive head trauma than in accidental trauma |
|
|
Munchausen’s Syndrome by Proxy
|
Fabricated or induced illness with repeated presentations for medical attention
Child with history of apnea, cyanosis, or seizures Ultimately the child may be severely damaged or may die Premeditated, usually by the mother who often has a medical background Video monitoring during hospitalization |
|

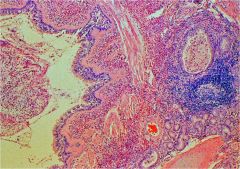
what is this syndrome?
|

Waterhouse-Friderichsen syndrome (WFS) or hemorrhagic adrenalitis is a disease of the adrenal glands most commonly caused by the bacterium Neisseria meningitidis. The infection leads to massive hemorrhage into one or (usually) both adrenal glands.[1] It is characterized by overwhelming bacterial infection meningococcemia, low blood pressure and shock, disseminated intravascular coagulation (DIC) with widespread purpura, and rapidly developing adrenocortical insufficiency.
|
|
Dx?
|
Asthma - a cause of pulm path in infant death
|
|
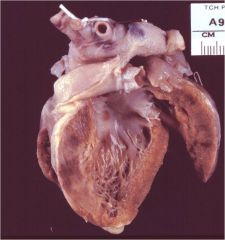
Dx?
|
Myocarditis - a cause of infant death
In medicine (cardiology), myocarditis is inflammation of heart muscle (myocardium). It resembles a heart attack but coronary arteries are not blocked. Myocarditis is most often due to infection by common viruses, such as parvovirus B19, less commonly non-viral pathogens such as Borrelia burgdorferi (Lyme disease) or Trypanosoma cruzi, or as a hypersensitivity response to drugs |
|
|
SIDS triad
|
|
|
|
SIDS triad?
|
|
|
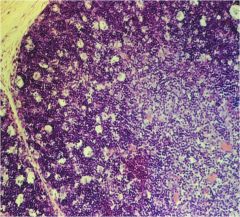
Dx?
|
In SIDS, Thymus can be nl or starry sky - here
|
|
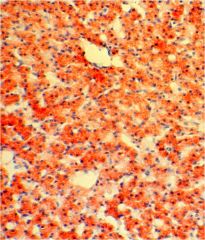
Dx?
|
cause of infant death - a metabolic disorder - in this case: defects in the enzyme complex known as medium-chain acyl dehydrogenase (MCAD) and reduced activity of this complex. This complex oxidizes medium chain fatty acids (Fatty acids having 6-12 carbons) while reducing FAD+ to FADH2
It is recognized as one of the more rare causes of sudden infant death syndrome (SIDS), although it may be better described as a mimic, rather than a cause, of SIDS. |
|
|
MIC?
|
Minimum inhibitory concentrations indicate the minimal concentration of antibiotic that will inhibit bacterial growth.
Minimum inhibitory concentrations for most antibiotics are commonly characterized as either MIC50 or MIC90. These values indicate the percentage of isolates of a particular bacterium that will be inhibited with different concen-trations of a drug. The MIC50 value indicates the concentration of antibiotic that will inhibit the growth of 50% of isolates, whereas an MIC90 indicates the concentration of antibiotic needed to inhibit 90% of isolates. |
|
|
pharmacokinetics and dynamics of Abx?
|
PK = effect in humans - consider serum concentration profile and penetration to site of infection
PD = effect in bacteria - consider potency (MIC) and mechanism of killing |
|
|
time- and concentration-dependent anti-biotics
|
For drugs that are concentration dependent, Peak/MIC or AUC/MIC are pre-dictors of clinical and microbiologic outcome.
For agents that are time dependent, it is necessary to prolong the duration of exposure, so the absolute concentration is not important. What is important in these drugs is the duration of contact time—the time that the concentration remains above the MIC (time above the MIC). |
|
|
Time above MIC (or time-dependent activity) is the parameter that best defines the activity of which antibiotics?
|
penicillins, cephalosporins, monobactams, carbapenems
|
|
|
The area under the curve AUC>MIC or the Peak>MIC (or concentration-dependent) are the parameters that best reflect the activity of which antibiotics?
|
aminoglycosides, fluoroquinolones, azalides, macrolides, clindamycin, oxazolidinones, and ketolides
|
|
|
what are the organisms we treat with natural penicillins 1st line?
|
Group A and B Streptococcus, susceptible S. pneumoniae, N. meningitidis, Actinomyces israelii and Treponema pallidum
|
|
|
What Abx are resistant to S.aureus beta-lactamase?
|
Nafcillin/oxacillin
|
|
|
Does Nafcillin/oxacillin affect enterococci?
|
NO
Enterococcus is not inhibited by nafcillin or other penicillinase- resistant penicillins |
|
|
ß-lactamase + H. influenzae
antibitiotic?? |
ß-lactamase inhibitors bind irreversibly to some ß-lactamases. Amoxicillin-clavulanate has excellent activity for ß-lactamase + H. influenzae
Amoxicillin-clavulanate is the drug of choice for animal and human bites due to activity against P. multocida, Eikenella sp. S. aureus and anaerobes |
|
|
drug of choice for animal and human bites due to activity against
P. multocida, Eikenella sp. S. aureus and anaerobes |
Amoxicillin-clavulanate
|
|
|
Treatment of GAS Pharyngitis
|
Group AStrep Pharyngitis:
Although penicillin V is the drug of choice for treatment of GAS pharyngitis, amoxicillin equally is effective. A clinical isolate of GAS resistant to penicillin never has been documented. Orally administered amoxicillin given as a single daily dose (50 mg/kg, maximum 1000 mg) for 10 days is as effective as orally administered penicillin V or amoxicillin given multiple times per day for 10 days. For some patients who are allergic to penicillin, a 10-day course of a narrow-spectrum (first-generation) oral cephalosporin is indicated. Patients with immediate or type I hypersensitivity to penicillin should not be treated with a cephalosporin. Erythromycin, clarithromycin, or azithromycin is acceptable for patients allergic to penicillins. |
|
|
Etiology of Acute Otitis Media
|
47% H. influenzae (40% with b-lactamase)
33% S. pneumo (47% penicillin resistant strains) 8% M. cat (100% with b-lactamase) 4% S. pyogenes 3% S. aureus |
|
|
Acute Otitis Media with Temperature >39°C and/or Severe Otalgia:
antibiotic? |
Amoxicillin-clavulanate, 90 mg/kg per day of amoxicillin, with 6.4 mg/kg per day of clavulanate
If penicillin allergy: Ceftriaxone, 1 or 3 days |
|
|
Acute Otitis Media without Temperature >39°C and/or Severe Otalgia:
antibiotic? |
Amoxicillin
80–90 mg/kg per day Penicillin allergy: Non-type I: cefdinir, cefuroxime, cefpodoxime; type I: azithromycin, clarithromycin |
|
|
Extended Spectrum Antipseudomonas
|
In general piperacillin is more active than ticarcillin for Pseudomonas sp ( as well as Burkholderia cepacia)
Addition of beta-lactamase inhibitor (clavulanate or tazobactam) does not increase activity against Pseudomonas sp. ßeta-lactamase inhibitors extend the activity of piperacillin and ticarcillin against most ß-lactamase producing E. coli, Klebsiella sp, methicillin-susceptible S. aureus and anaerobes |
|
|
Cephalosporins - Spectrum of Activity
Selected Features of 1st Generation 1) activity against MSSA and GAS 2) activity against Enterococcus 3) activity against Listeria 4) activity against MRSA 5) activity against bacterial meningitis 6) surgical prophylaxis?? |
Activity primarily for methicillin-susceptible
S. aureus and Group A streptococcus No cephalosporin is active against Enterococcus sp or Listeria moncytogenes Not active against methicillin-resistant staphylococci Do not penetrate into CSF adequately for routine treatment of bacterial meningitis Cefazolin useful for surgical prophylaxis due to its activity against S. aureus and S. pyogenes |
|
|
Cephalosporins - Spectrum of Activity-Selected Features of 2nd Generation
1) activity against GN enterics / Gram positives in comparison to 1st generation 2) activity against H.influenza / Moraxella 3) activity against URI / LRI 4) activity against bacterial meningitis? |
More active than 1st generation agents against Gram-negative enterics but less active against Gram-positive organisms
Useful activity against H. influenzae and Moraxella catarrhalis (Cefuroxime) Useful for treatment of upper and lower respiratory infections; IV and oral formulations Do not penetrate into CSF adequately for routine treatment of bacterial meningitis |
|
|
Cephalosporins - Spectrum of Activity-Selected Features of 3rd and 4th Generations
1) activity against GN enterics / Gram positives in comparison to 1st/2nd generation 2) activity against bacterial meningitis? 3) activity against Shigella resistant to ampicillin or bactrim 4) activity against pseudomonas? |
Improved activity for gram-negative but less active against gram positive (except streptococci) than 1st or 2nd generation cephalosporins except for S. pneumoniae (cefotaxime or ceftriaxone)
Penetrate well into CSF and are first line agents for treatment of bacterial meningitis. (cefotaxime/ceftriaxone) Cefixime, cefpodoxime and cefdinir remain active against Shigella spp resistant to ampicillin or TMP-SMX Ceftazidime and cefepime have important activity against Pseudomonas spp |

