![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
96 Cards in this Set
- Front
- Back
|
Rank opioids from most to least lipid soluble.
|
• The order of opioid lipid-solubility ranked from most to least:
› sufentanil (1778) › fentanyl (955) › alfentanil (145) › meperidine (39) › remifentanil (17.9) › morphine (1.9) |
|
|
Which opioid should not be given with a neuraxial technique? Why?
|
• Remifentanil should not be administered intrathecally or epidurally, as the safety of the buffering vehicle has not been determined. The buffering vehicle is glycine, which is an inhibitory neurotransmitter.
|
|
|
What is the more common name of 2-(0-chloropheny1)-2-methylaminoc yclohexanone hydrochloride?
|
• 2-(0-chloropheny1)-2-methylamino cyclohexanone hydrochloride is ketarnine.
• Tip: the "one" is from the ketone group; the name ketarnine emerged from "keto-amine. |
|
|
What is another name for 2,6 diisopropylphenol?
|
Propofol is 2,6-diisopropylphenol
|
|
|
What is the maximal safe dose of cocaine when applied nasally or topically?
|
• The maximum dose of cocaine is 200 mg for a 70 kg individual, or 3 mg/kg (Barash).
• Stoelting states 150 mg is the single maximum does of cocaine. NB: be aware of the conflict with Omoigui's Anesthesia Drug Handbook, which states 1.5 mg/kg is the "maximal safe dose of cocaine". |
|
|
Benzocaine is ideally suited for what clinical use, in light of its weak acid nature and pK, 3.5?
|
• Since benzocaine is almost completely ionized at pH 7.4, it is ideally suited for topical anesthesia of mucous membranes prior to tracheal intubation, endoscopy, transesophageal echocardiography, and bronchoscopy.
|
|
|
Identify the recommended dose of benzocaine for topical anesthesia. What potentially life-threatening complication may ensue if the usual dosing is exceeded?
|
• A brief spray of 20% benzocaine delivers the recommended dose of 200 to 300 mg. If dosing exceeds 200 to 300 mg, methemoglobinemia may occur.
|
|
|
List the local anesthetics and their concentrations that comprise EMLA cream (eutectic mixture of local anesthetics).
|
combination of 2.5% prilocaine and 2.5% lidocaine cream (5% total concentration) is called a eutectic mixture of local anesthetics (EMLA), because the melting point of the combined drugs is lower than prilocaine or lidocaine alone.
• ("Eutectic" means equal proportions of solid crystals of prilocaine and lidocaine, and this mixture remains a liquid at room temperature.) |
|
|
Which ester local anesthetic is a weak acid? What is the pK, of this unusual local anesthetic?
|
• Benzocaine (ethyl arninobenzoate) is unique among clinically useful local anesthetics because it is a weak acid and has a pK, of 3.5.
• Recall that all other clinically useful locals are weak bases, with pK, ranging from 7.6 to 9.1. |
|
|
What form-mostly ionized or mostly nonionized-exists when benzocaine encounters physiologic pH?
|
• Benzocaine, a weak acid with a pKa = 3.5, will be almost exclusively ionized at physiologic pH 7.4.
• Recall that a weak acid placed into a relatively basic environment (3.5 3 7.4, pH > p&) becomes more ionized. A handy mnemonic: "like into unlike = more ionized", that is, weak acid into a basic environment = more ionized. NB: Stoelting incorrectly states that benzocaine is mostly nonionized at physiologic pH. |
|
|
Which local anesthetics are chiral drugs (possessing an asymmetric carbon center)?
|
• The pipecoloxylidide local anesthetics (mepivacaine, bupivacaine, ropivacaine, levobupivacaine) are chiral drugs because their molecules possess an asymmetric carbon atom. As such, these drugs may have a left (S) or right (R) handed configuration. Molecules that are stereospecific superimposable mirror images of each other and called enantiomers. Enantiomers are optically active--they rotate plane polarized light.
|
|
|
Which two local anesthetics are administered as racemic mixtures (50:50 mixture of enantiomers)?
|
• Mepivacaine and bupivacaine are available for clinical use as racemic mixtures (50:50 mixture) of the enantiomers. The enantiomers of a chiral drug may vary in their
|
|
|
Identify the two local anesthetics that are pure S enantiomers. What is the advantage of these local anesthetics?
|
• Ropivacaine and levobupivacaine have been developed as pure S enantiomers (they are not racemic mixtures).
• These S enantiomers produce less neurotoxicity and cardiotoxicity than racemic mixtures or the R enantiomers of local anesthetics, perhaps reflecting decreased potency at sodium ion channels. • S=”safe” • R=RACEMIC=”risky” |
|
|
Name the two active metabolites produced by lidocaine metabolism.
|
• Monoethylglycinexylidide (MEGX) and glycine xylidide (GX) are the active products of lidocaine metabolism by liver microsomal P450 system.
|
|
|
Postoperative muscle pain due to skeletal muscle fasciculations is a common problem after succinylcholine administration. How may you minimize the postoperative skeletal muscle pain following succinylcholine administration?
|
• In order to minimize fasciculations associated with succinylcholine and subsequent postoperative skeletal muscle pain, a defasciculating dose (10% to 15% of intubating dose) of nondepolarizing muscle blocker may be administered 5 minutes prior to the succinylcholine administration.
|
|
|
What is the appropriate premedication dose of atropine for the adult with severe bradycardia?
|
• As a premedication, atropine is administered intravenously or intramuscularly in a range of 0.01-0.02 mg/kg up to the usual adult dose of 0.4-0.6 mg/kg.
• Larger intravenous doses up to 2 mg may be required to completely block the cardiac vagal nerves in treating severe bradycardia. Omoigui states: "0.5-1.0 mg IV/IM/SC, repeat every 3 to 5 minutes as indicated." |
|
|
Which of the 4 common anticholinesterase agents is not a quaternary ammonium?
|
• Physostigmine is a tertiary amine.
• Edrophonium, neostigmine, and pyridostigmine are all quaternary amines. • Remember: physostigmine is not used to reverse neuromuscular blockade because the dose required to achieve this effect is excessive. Nonetheless, physostigmine is an anticholinesterase. |
|
|
Rank order the anticholinesterase and anticholinergic agents based on onset (in minutes), from fastest to slowest.
|
• The order of onset (in minutes) for anticholinergic and anticholinesterase agents, from fastest to slowest is: atropine (1-2 min), glycopyrrolate (2 min), edrophonium (5-10 min), neostigmine (5-15), and pyridostigmine (10-20).
• Onset(F-S): AGENP |
|
|
Rank order anticholinesterase and anticholinergic agents based on duration (in minutes), from shortest to longest.
|
• The order of duration (in minutes) for anticholinergic and anticholinesterase agents, from shortest to longest, is: edrophonium (30-60 min) < neostigmine (45-90 min) < atropine (60-120 min) = pyridostigmine (60- 120) < glycopyrrolate (120-240).
• DOA (S-L): ENAPG |
|
|
Give 6 contraindications/cautions to esmolol administration.
|
• Esmolol is contraindicated-or should be used with caution (textbook variations)-in the following 6 patients:
› (1) with sinus bradycardia › (2) with AV heart blocks, especially greater than first degree › (3) with chronic obstructive pulmonary disease › (4) hypotensive › (5) with cardiogenic shock › 6) with cardiac failure. |
|
|
The alpha-2 adrenergic receptor agonist clonidine, acts where centrally to produce what therapeutic effect?
|
• Stimulation of alpha-2A receptors of inhibitory neurons in the vasomotor center of the medulla in the brain stem inhibits sympathetic nervous system outflow. This action decreases blood pressure.
|
|
|
Alpha-2 adrenergic receptor agonists antagonize the sympathetic nervous system peripherally. How?
|
• Alpha-2 receptors are found peripherally in the surface membrane of the norepinephrine-containing presynaptic nerve terminals of sympathetic postganglionic neurons.
• Stimulation of these receptors decreases the release of norepinephrine from the presynaptic nerve terminal. This decreased release of norepinephrine contributes modestly to the clonidine-induced decrease in blood pressure. |
|
|
The patient administered sodium nitroprusside continuously (by drip) presents with the following arterial blood gases (ABGs): pH = 7.21, PaC02 = 32 mm Hg, Pa02 = 104 mm Hg, base excess = -10 mEq/L. What is your next action? Explain the arterial blood gases.
|
• Turn off the nitroprusside drip.
• These ABGs suggest cyanide toxicity. • The base excess of -10 mEq/L (base deficit of 10 mEq/L) demonstrates that the acidosis is metabolic. The low PaC02 of 32 mm Hg demonstrates partial respiratory compensation of the metabolic acidosis. |
|
|
What is your concern with giving phenytoin (Dilantin) to the hyperglycemic patient?
|
• Phenytoin (Dilantin) partially inhibits (blunts) insulin release and may lead to increased blood glucose levels in patients who are hyperglycemic.
|
|
|
During, what time frame should warfarin be discontinued prior to surgery?
|
• Warfarin should be discontinued 3-5 days prior to surgery
|
|
|
Name the three clinically useful GPIIb/IIIa antagonists (inhibitors) and describe their mechanism of action.
|
• The three clinically approved GPIIb/IIIa antagonists are:
› (1) abciximab (ReoPro), a monoclonal antibody; › (2) eptifibatide (Integrilin), a synthetic peptide analog › (3) tirofiban (Aggrastat), a nonpeptide analog. • All three GPIIb/IIIa inhibitors competitively occupy the fibrinogen binding site, thus preventing platelet aggregation. These drugs are thus antiplatelet agents. |
|
|
What is the route of administration of the GPIIb/IIIa inhibitors (abciximab, eptifibatide, and tirofiban)?
|
• All three GPIIb/IIIa inhibitors must be administered intravenously; there are no current oral preparations of these agents.
|
|
|
What are the indications for GPIIb/IIIa inhibitors?
|
• The GPIIb/IIIa antagonists have been used principally for the management of acute coronary syndromes and percutaneous coronary interventions (PCI).
|
|
|
What are the elimination half-times for the anti-GPIIb/IIIa agents? Are their effects reversible?
|
• The antiplatelet effects of all three anti-GPIIb/IIIa agents are reversible.
• The elimination half-time for › eptifibatide and tirofiban are 2-4 hrs. › abciximab has an elimination half-time of 12-24 hours |
|
|
In preparation for surgery, when should the last dose of low molecular weight heparin (LMWH) be given?
|
• The last does of low-molecular-weight heparin (LMWH) should be given 12 hours before the procedure.
|
|
|
After the surgical procedure, when should heparin be restarted?
|
• Heparin should be restarted 12 hours after the surgical procedure, even in high-risk patients, because the risk for severe hemorrhage is substantial.
|
|
|
Following a dose of low-molecular-weight heparin, when can a neuraxial intervention be performed?
|
• Neuraxial interventions should be delayed 10-12 hours after a dose of low-molecular-weight heparin.
|
|
|
If a neuraxial catheter is in place and a dose of heparin is given, how long should you wait before removing the catheter? How long should you wait before administering the next dose of heparin?
|
• Neuraxial catheter removal is acceptable 2 to 4 hours after heparin dosing AND with normal PTT or ACT.
• Wait 1 hour after catheter removal to administer a repeat dose of heparin. |
|
|
If a neuraxial catheter is in place and a dose of low molecular weight heparin (LMWH) is given, how long should you wait before removing the catheter? How long should you wait before administering the next dose of LMWH?
|
• Neuraxial catheter removal is acceptable 10 to 12 hours after the last dose of low-molecular-weight heparin.
• Wait 2 hours after catheter removal to administer the next dose of LMWH. |
|
|
List eight (8) deleterious effects of methylene blue administration.
|
› (1) destruction of RBCs with prolonged use
› (2) hypertension › (3) urinary bladder irritation › (4) nausea › (5) diaphoresis › (6) may inhibit nitrate-induced coronary artery relaxation › (7) interferes with pulse oximetry for 1-2 minutes › (8) can cause hemolysis in patients with glucose-6-phosphate dehydrogenase deficiency. |
|
|
What diuretic can cause ototoxicity (deafness), especially in patient with renal insufficiency?
|
• Loop diuretics, especially furosemide, may cause ototoxicity particularly in patients with renal insufficiency. This transient or permanent side effect is most likely to occur with prolonged increases in the plasma concentration of these drugs in the presence of other ototoxic drugs.
|
|
|
Bleomycin is toxic to what body organ? Why does bleomycin accumulate in this organ?
|
• Bleomycin, an antibiotic/chemotherapeutic, is toxic to the pulmonary system. Bleomycin is concentrated preferentially in the lung because the enzyme that inactivates bleomycin (hydrolase) is relatively deficient in lung tissue.
|
|
|
Describe phospholipase A2 (PLA2).
|
• Phospholipase A2 (PLA2) is the rate-limiting enzyme that catalyzes the liberation of arachidonic acid from membrane phospholipids. The liberation of arachidonic acid is the first step in the production of prostaglandins, leukotrienes, and thromboxanes (and other substances, too).
|
|
|
How do corticosteroids alter phospholipase A2 (PLA2), ultimately leading to reduced inflammation?
|
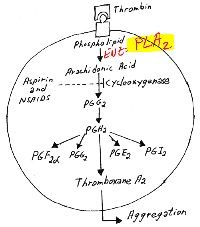
• Steroids decrease inflammation by inducing the biosynthesis of a PLA2 inhibitor and preventing subsequent prostaglandin generation.
|
|
|
Statins {atorvastatin (Lipitor), fluvastatin (Lescol), lovastatin (Mevacor), pravastatin (Pravachol), and simvastatin (Zocor)} are some of the most commonly-prescribed drugs in the general population. How do statins work?
|
• Statins are drugs that act as inhibitors of HMG-CoA reductase, the rate limiting enzyme in cholesterol accompanied by decreases (up to 60%) in LDL ("bad") cholesterol. (HMG-CoA is hydroxymethylglutaryl coenzyme A)
|
|
|
What are the two most-feared side effects of statin administration? What laboratory tests should be requested for the patient taking statins?
|
• The two most-feared side effects of statin therapy are
› 1) liver dysfunction with elevated haptic enzymes, › (2) severe myopathy with the possibility of rhabdomyolysis, myoglobinuria, and acute renal failure. • Liver function tests should be performed, up through the morning of the surgery. CPK (CK) levels should be monitored, especially if the patient complains of myalgias. |
|
|
What was the first immunosuppressive drug to be used clinically? What is the mechanism of action of this drug?
|
• Azathioprine (Imuran) was introduced in 1962. Azathioprine is an antimetabolite immunosuppressant and works by inhibiting DNA synthesis in proliferating cells.
|
|
|
Identify the side effects of azathioprine administration.
|
• Since azathioprine inhibits DNA synthesis in proliferating cells, side effects extend to normally proliferating cells, such as the lining of the gastrointestinal tract, bone marrow, and skin. Repression of bone marrow cell cycling can cause pancytopenia and azathioprine has been associated with a significant increase in skin cancer.
|
|
|
The "modern transplant era" began with the introduction of calcineurin inhibitors (1979, and 1983). Identify two main calcineurin inhibitors and describe their mechanisms of action.
|
• Cyclosporine (Sandimmunew, Neoral) and tacrolimus (Prograf, FK506) are calcineurin inhibitors. Inhibition of calcineurin prevents T- lymphocyte proliferation and cytokine production, particularly interluekin-2 (IL-2) production.
|
|
|
Caineurin is involved in diverse cellular processes in addition to immune function; therefore inhibition of calcineurin has many side effects. List the side effects of a calcineurin inhibitor, such as cyclosporine or tacrolimus.
|
• Inhibition of calcineurin has many significant side effects including hypertension, hyperlipidemia, ischemic vascular disease, diabetes, nephrotoxicity, and central neurologic effects. Tacrolimus causes up regulation of cytochrome P450 3A4 isoform.
|
|
|
What effect does hypothermia have on gas solubility?
|
• As a liquid is cooled, more gas dissolves in the liquid; therefore hypothermia will cause an increase in gas solubility.
|
|
|
What is Dalton's law?
|
• Dalton's law of partial pressures states that the total pressure (TP) of a group of gases is equal to the sum of their individual partial pressures. Mathematically, P total = P1 + P2 + P3.
|
|
|
If atmospheric pressure is 710 mmHg, and the 02:N20 delivery is 2L:4L (6L total flow), what partial pressure of O2 and what partial pressure of N20 are delivered to the patient? Whose law permits these calculations?
|
• One-third (216 = 33.3%) of the delivered gas is 02, and two-thirds (416 = 66.7%) is N20. PO2 = 0.333 x 710 mmHg = 236 mmHg; PN2O= 0.667 x 710 mmHg = 474 mmHg.
• Dalton's law of partial pressures permits these calculations to be made. |
|
|
What happens to the temperature of a liquid as vaporization occurs?
|
• Since vaporization requires energy, the temperature of a liquid decreases as vaporization proceeds. As the liquid temperature falls, a gradient is established between the liquid and the surrounding environment. Energy flows from the warmer area (surroundings) to the cooler area (liquid) -- this flow of thermal energy is called heat. At some point, an equilibrium is reached at which the energy lost (heat) to vaporization is matched by the energy supplied from the surroundings (heat).
|
|
|
What is heat of vaporization? What is the latent heat of vaporization?
|
• The phase change from the liquid state to the gaseous state is called vaporization. It takes energy for the molecules in a liquid phase to break away and enter the gaseous phase.
• A liquid's heat of vaporization is the number of calories (a measure of energy) necessary to convert 1 mL liquid into a vapor. • The latent heat of vaporization is more precisely defined as the number of calories required to change 1 g of liquid into vapor without a temperature change |
|
|
Describe what may happen to vapor pressure if a carrier gas flows through the vaporizer container.
|
• As a flow of gas (carrier gas) passes through the vaporizer container, molecules of vapor are carried away. This causes the equilibrium to shift so that more molecules enter the vapor phase. Unless some means of supplying heat is available, the liquid will cool. As the temperature drops, so does the vapor pressure of the liquid, and the carrier gas will pick up fewer molecules so that there is a decrease in concentration in the gas flowing out of the container.
|
|
|
Your geriatric patient has severe shortness of breath and wheezing, along with inspiratory and expiratory stridor. Further examination reveals a proximal tracheal compression by a tumor. Identify the airflow pattern within the trachea at the obstruction.
|
• Orifice-flow - -a type of turbulent flow -- occurs at severe constrictions, such as a nearly closed larynx, trachea, or kinked endotracheal tube. Orifice flow can occur when the diameter of tube is greater than tube length.
|
|
|
A full E-cylinder at 800 psi is connected to a delivery system set to provide 2 L/min. How long will the E-cylinder supply provide this flow rate?
|
• A full E-cylinder contains 625 liters at 2200 psi. As a first approximation, there is about 113 the original volume remaining, since 800 psi is about 113 of 2200 psi. Since the volume-pressure relationship is essentially linear, there should be about 113 the original volume as well, or approximately 208 liters of gas remains in the cylinder. A volume of 208 L running at 2 L/min will provide approximately 104 minutes of gas at this flow rate.
|
|
|
Identify the four (4) components of the anesthesia gas machine that are exposed to high pressures (cylinder pressure).
|
• The four components of the anesthesia gas machine that are exposed to high-pressure (cylinder pressure) are:
› (1) hanger yoke › (2) yoke block with check valves › (3) cylinder pressure gauge › (4) cylinder pressure regulators |
|
|
Identify the eight (8) components of the anesthesia gas machine that are exposed to intermediate pressures (pipeline pressure, 50 psi)
|
• The eight components of the anesthesia gas machine that are exposed to intermediate pressures (pipeline pressure, 50 psi) are:
› (1) pipeline inlets › (2) check valves › (3) pressure gauges › (4) ventilator power inlet › (5) oxygen pressure-failure device › (6) flow meter valve › (7) oxygen second-stage regulator › (8) flush valve |
|
|
Identify the four (4) components of the anesthesia gas machine that are exposed to low pressures (distal to flow meter needle valve)
|
• The four components of the anesthesia gas machine that are exposed to low pressures are all distal to the flow meter needle valve.
• The components are: › (1) flow meter tubes › (2) vaporizers › (3) check valves › (4) common gas outlet |
|
|
What system prevents filling a vaporizer with the incorrect agent?
|
• The keyed filling port system on modern vaporizers prevents filling with the incorrect agent.
|
|
|
What is the function of an auxiliary flow meter on the gas machine? What is the advantage of an auxiliary flow meter?
|
• Auxiliary flow meters are useful for attaching supplemental oxygen delivery devices, such as a nasal cannula, to the gas machine.
• The auxiliary flow meter is advantageous because the breathing circuit and gas delivery hose remain intact while supplemental oxygen is delivered to a spontaneously breathing patient. Another advantage is that an oxygen source is readily available for the Ambu bag if the patient needs to be ventilated manually for any reason during the case. |
|
|
What is the primary disadvantage of an auxiliary flow meter?
|
• If pipeline supply has lost pressure or has been contaminated, the auxiliary flow meter becomes unavailable.
• Another disadvantage is that the fraction of inspired inspiration cannot be varied with the auxiliary flow meter. |
|
|
Which vaporizer is a "dual-circuit" gas vapor blender? To what feature does the "dual-circuit" apply?
|
• The Tec 6 vaporizer is an electrically heated, thermostatically controlled, constant-temperature, pressurized, electromechanically coupled dual circuit, gas-vapor blender.
• The pressure in the vapor circuit is electronically regulated to equal the pressure in the fresh gas circuit. |
|
|
What is the main function of the check valve(s) in a gas machine?
|
• Check valves, also called unidirectional or one-way valves, prevent retrograde flow (back flow) during positive pressure ventilation, therefore minimizing the effects of downstream intermittent pressure fluctuations on inhaled anesthetic concentration.
|
|
|
Describe the purpose of the fail-safe valve on the anesthesia machine.
|
• The fail-safe valve prevents the delivery of hypoxic gas mixtures from the machine in the event of failure of the oxygen supply.
• The fail-safe valve goes by many other names-the oxygen failure safety valve, oxygen failure safety device, low-pressure guardian system, oxygen failure protection device, pressure sensor shutoff system or valve, pressure sensor system, and nitrous oxide shutoff valve. |
|
|
What are your actions when the oxygen low pressure alarm sounds?
|
• When the oxygen low-pressure alarm sounds-indicating profound loss of 02 pipeline pressure—fully open the E cylinder, disconnect the pipeline, and consider use of low fresh gas flows
|
|
|
What is the proportioning system on the anesthesia workstation?
|
• A proportioning system on the anesthesia workstation is a hypoxia prevention safety device. Manufacturers equip anesthesia workstations with proportioning systems in an attempt to prevent creation and delivery of a hypoxic mixture.
• Nitrous oxide and oxygen are mechanically and/or pneumatically linked so that the minimum oxygen concentration at the common gas outlet is between 23 to 25% depending on manufacturer. |
|
|
How does the Link-25 proportioning system work?
|
• The Link-25 system is found on conventional Datex-Ohmeda machines. The heart of the system is the mechanical integration of the nitrous oxide and oxygen flow control valves.
• It allows independent adjustment of either valve, yet automatically intercedes to maintain a minimum 25% oxygen concentration with a maximum nitrous oxide-oxygen flow ratio of 3:1 • The Link-25 automatically increases oxygen flow to prevent delivery of a hypoxic mixture. A 14-tooth sprocket is attached to the nitrous oxide flow control valve and a 28-tooth sprocket is attached to the oxygen flow control valve. A chain physically links the sprockets. When the nitrous oxide flow control valve is turned through two revolutions, or 28 teeth, the oxygen flow control valve will revolve once because of the 2:1 gear ratio. • The final 3:1 flow ratio results because the nitrous oxide flow control valve is supplied by approximately 26 psig, whereas the oxygen flow control valve is supplied by 14 psig. Thus, the combination of the mechanical and pneumatic aspects of the system yields the final oxygen concentration. • The Link-25 proportioning system can be thought of as a system that increases oxygen flow when necessary to prevent delivery of a fresh gas mixture with oxygen concentration of less than 25%. |
|
|
List five (5) conditions that can "fool" the proportion-limiting systems.
|
• The following five situations can lead to delivery of hypoxic gas mixtures on workstations equipped with proportioning systems:
› (1) wrong supply gas › (2) defective pneumatics or mechanics › (3) leaks downstream › (4) inert gas administration › (5) dilution of inspired oxygen concentration by volatile inhaled anesthetics |
|
|
What type of gas can lead to delivery of a hypoxic mixture on a workstation equipped with a proportioning system? What is mandatory when such a gas is present?
|
• An inert, third gas, such as He, N2 or C02, can cause delivery of a hypoxic mixture because contemporary proportioning systems link only nitrous oxide and oxygen.
• Use of an oxygen analyzer is mandatory (or preferentially a multigas analyzer, when available) if the operator uses a third gas. |
|
|
What oxygen sources and delivery pressures are acceptable for transtracheal jet ventilation? What sources and pressures are not adequate for transtracheal jet ventilation?
|
• There are several options for the oxygen source and delivery pressures used with transtracheal ventilation. If a high-pressure system is available-- for example, a metered and adjustable oxygen source with a hand controlled valve and a Luer-lock connector --15 to 30psi of oxygen (central hospital supply or regulated cylinder) can be delivered directly through the catheter, with insufflations of 1 to 1.5 seconds at a rate of 12 insufflations per minute. If a 16-gauge catheter has been placed, this system will deliver a tidal volume of 400 to 700 mL. At a delivered pressure of 50 psi, a 16-guage delivers 500 mL of oxygen
|
|
|
What is a double-circuit ventilator?
|
• Double-circuit ventilators (bellows in a box, bag in a bottle), in which one circuit contains patient gas and the other circuit contains drive gas, are used most commonly on modern anesthesia workstations.
• The bellows is housed in a pressure chamber, and the inside of the bellows is connected to the breathing system. The double-circuit separates breathing system gas from driving gas. Generally, these conventional ventilators are pneumatically driven. |
|
|
Consider a ventilator in pressure control mode: what parameter fluctuates with each cycle? What patient parameters determine this fluctuation?
|
• In pressure control mode, the ventilator is set so that the inspiratory pressure is greater than the positive end-expiratory pressure. In this mode, tidal volume fluctuates (varies) with alterations in patient pulmonary compliance, pulmonary resistance, and with patient-ventilator asynchrony.
|
|
|
Identify four (4) reasons why positive pressure ventilation of 25 cm Hz0 would not be sufficient to ventilate an individual.
|
• Positive pressure ventilation at 25 cm Hz0 would not be enough pressure to ventilate if:
› (1) the upper airway is obstructed › (2) the patient has sufficient muscle tone to prevent chest expansion › (3) the individual has decreased pulmonary compliance, or › (4) the individual has increased pulmonary resistance |
|
|
What is the suggested protocol to wean a patient from synchronized intermittent mandatory ventilation (SIMV)?
|
• To wean a patient from synchronized intermittent mandatory ventilation (SIMV), progressively decrease the number of breaths (by 1-2 breaths/minute) as long as the arterial C02 tension and respiratory rate remain acceptable (generally < 45-50 mm Hg and less than 30 breaths per minute).
|
|
|
What is the most common site for breathing circuit disconnection?
|
• Although disconnections can occur anywhere in the breathing system, the most common site is between the breathing system and tracheal tube connector or heat-moisture exchanger (HME).
|
|
|
Rank the relative efficiency of Mapleson systems with respect to prevention of rebreathing during spontaneous ventilation.
|
• With respect to prevention of rebreathing during spontaneous ventilation, the relative efficiency of Mapleson systems is A > DFE > CB.
|
|
|
Rank the relative efficiency of Mapleson systems with respect to prevention of rebreathing during controlled ventilation.
|
• With respect to prevention of rebreathing during controlled ventilation, the relative efficiency of Mapleson systems is DFE > BC > A.
|
|
|
You are scheduled to provide anesthesia to a patient with a known susceptibility to malignant hyperthermia. How will you prepare the gas machine in anticipation of this case?
|
• The concern in this situation is the presence of trace amounts of volatile agents in the rubber and plastic components of the gas machine and in the ventilator and C02 absorber.
• The following 3 actions should be taken to prepare the gas machine for the patient with a known susceptibility to malignant hyperthermia. › (1) The gas machine should be thoroughly flushed with 100% oxygen for at least 10 minutes to remove residual traces of volatile agents from rubber and plastic components in the machine. › (2) The breathing circuits and CO2 canister should be replaced. › (3) Vaporizers should be drained, inactivated, or removed. |
|
|
When is a nasopharyngeal airway preferable to an oropharyngeal airway?
|
• A nasopharyngeal airway (nasal airway, nasal trumpet) is better tolerated than an oral airway if the patient has intact airway reflexes.
• A nasal airway is preferable if the patient's teeth are loose or in poor condition, if there is trauma or pathology of the oral cavity and can be used when the mouth cannot be opened. |
|
|
List four (4) contraindications to using a nasopharyngeal airway.
|
• Contraindications to a nasopharyngeal airway include
› (1) anticoagulation › (2) basilar skull fracture › (3) pathology, sepsis, or deformity of the nasal cavity or nasopharynx, and › (4) a history of nosebleeds requiring medical treatment |
|
|
What is the purpose of an oral airway? List five (5) uses for an oral airway.
|
• Any airway creates an artificial, patent passage to the hypopharynx.
• Oral airways are used to › (1) prevent the patient from biting an oral tracheal tube › (2) protect the patient from biting the tongue › (3) facilitate oropharyngeal suctioning › (4) obtain a better mask fit › (5) provide a pathway for inserting devices into the esophagus or pharynx. |
|
|
When is an oral airway indicated? Contraindicated?
|
• An oral airway is indicated for an obstructed upper airway in an unconscious patient and when there is need for a bite block in an unconscious patient.
• An oral airway is contraindicated in the awake or lightly anesthetized patient--the patient may cough or develop laryngospasm during airway insertion if laryngeal reflexes are intact. |
|
|
What is the purpose of the laryngoscope flange?
|
• The flange projects off the left side of the laryngoscope and serves to sweep the tongue out of the way and to guide instrumentations along the laryngoscope blade.
|
|
|
Into what shape should a lighted intubation stylet ("lightwand") be molded? What approximate angle is the bend of this shape?
|
• For oral intubation, a "J" or "hockey stick" bend of approximately 75- to 120-degrees just proximal to the cuff is recommended. Care should be taken not to bend the stylet at the point at which the bulb meets the shaft.
|
|
|
List potential uses for an airway exchange catheter.
|
• An airway exchange catheter (guiding catheter, director, stylet catheter, catheter. catheter guide, elastic stylet, tracheal tube replacement obturator, tube changer or exchanger, ventilation or exchange bougie, jet-style catheter, jet stylet, intubation catheter, intubating introducer) can be used for a number of purposes including: tracheal tube or supraglottic device exchange, replacing and existing tube, changing a tracheal tube from oral to nasal, intubation, extubation, to provide ventilation during microlaryngeal surgery, to provide a useful guide to the trachea during flexible endoscopy, and facilitating passage of a tracheal tube over a fiberscope.
|
|
|
What features are advantageous for an airway exchange catheter? What do these features afford during extubation?
|
• Airway exchange catheters have a central lumen, and rounded, atraumatic ends. The catheters are graduated from the distal end. The proximal end is fitted with either a 15-mm or a Luer-lock Rapi-Fit adapter, which can be quickly removed and replaced for ETT removal or exchange. With these adapters an oxygen source can be used to provide insufflated or jet ventilated oxygen if the patient fails extubation and/or if reintubation over the catheter fails.
|
|
|
What is an Eschmann introducer?
|
• The Eschmann introducer is a 60-cm, stylet-like device that has a 5-mm external diameter and a 35-degree bend 2.5 cm from the end that is inserted into the trachea. Its structure is designed to provide a combination of stiffness and flexibility. It is more commonly known as the gum elastic bougie, (although it is not gum, elastic, or a bougie, according to Miller!).
• It is an extremely useful instrument when laryngoscopic view is poor or the tube cannot be otherwise guided into the glottis. It is also useful in limiting the degree of necessary neck movement during intubation with potential cervical spine injuries and to lessen the risk of dental damage. The introducer can be manipulated under the epiglottis, its angled segment directed anteriorly toward the larynx. Once it has entered the larynx and trachea, a distinctive "clicking" feel is elicited as the tip passes over the cartilaginous structures. |
|
|
Inspiratory pressure should be limited to what value when providing positive pressure ventilation by a manual resuscitator (bag-valve mask, for example)?
|
• When providing positive-pressure ventilation with a manual resuscitator, such as a bag-valve mask, it is imperative to limit the positive pressure to 25 cm H20 to avoid inflating the stomach, which increases the risk of
regurgitation. |
|
|
What is the most common complication to a patient being jet ventilated?
|
• Tracheal mucosal damage and thickened secretions blocking the airways, which result from inadequate humidification of the delivered gas, remains a major problem during high frequency jet ventilation.
|
|
|
How is sterilization differentiated from disinfection?
|
• Disinfection is a process capable of destroying most microorganisms but, as ordinarily used, not bacterial spores.
• Sterilization is a process capable of removing or destroying all viable forms of microbial life, including bacterial spores, to an acceptable sterility assurance level. |
|
|
The Centers for Disease Control and Prevention (CDC) has classified three (3) levels of disinfection: name and describe the three levels of disinfection as categorized by the CDC.
|
• The three levels of disinfection, as adopted by the Centers for Disease Control and Prevention (CDC) are as follows.
› (1) High-level Disinfection: A procedure that kills all organisms with the exception of bacterial spores and certain species, such as the Creutzfeldt-Jakob prion. Most high-level disinfectants can produce sterilization with sufficient contact time. › (2) Intermediate-level Disinfection: A procedure that kills vegetative bacteria, including acid-fast Mycobacterium tuberculosis, most fungi, and viruses but not bacterial spores. › (3) Low-level Disinfection: A procedure that kills most vegetative bacteria (but not M, tuberculosis), some fungi, and viruses but no spores. |
|
|
Describe Pasteurization.
|
• Pasteurization is a high-level disinfection process in which the equipment is immersed in water at an elevated temperature (but below 100°C) for a specified time.
• A typical sequence is 30 minutes at a temperature of 70°C. |
|
|
List anesthetic equipment that may be disinfected by pasteurization
|
• Pasteurization has been used for breathing tubes, reservoir bags, tracheal tubes, face masks, airways, laryngoscope blades, stylets, bite blocks, Y-pieces, elbows, adaptors, and ventilator bellows.
|
|
|
Describe steam sterilization (autoclaving).
|
• Steam sterilization (autoclaving) utilizes saturated steam under pressure.
• It is the most widely used and inexpensive of the sterilization techniques. • At sea level, water boils at 100°C. When it is boiled within a closed vessel at increased pressure, the temperature at which it boils and that of the steam it forms will exceed 100°C. • The increase in temperature depends on the pressure within the chamber. Pressure per se has little or no sterilizing effect. It is the moist heat at a suitable temperature, as regulated by the pressure in the chamber, which brings about sterilization. • Increasing the temperature dramatically reduces the time needed to achieve sterilization. › The minimum time for sterilization by steam at 121 °C is 15 minutes. › If the temperature is 126°C the time is reduced to 10 minutes. › Time for sterilization by steam is 3.5 minutes at 134C, and › Only a few seconds at 150°C. |
|
|
Describe chemical disinfection/sterilization and then list seven (7) chemical disinfectants.
|
• Chemical (cold) disinfection/sterilization involves immersing an item in a solution that contains a disinfectant. This method is especially useful for heat-sensitive equipment.
• It can be accomplished by automated equipment, which typically provides a cycle of cleaning, rinsing, disinfection, rinsing, and sometimes drying. • Seven common chemical disinfectants are: › (1) quaternary ammonium compounds › (2) alcohols › (3) glutaraldehydes (Cidex, Cetylcide) › (4) hydrogen peroxide-based solutions › (5) formaldehyde and other aldehydes › (6) phenolic compounds › (7) chlorine (hypochlorite, bleach). |
|
|
Of the 7 chemical disinfectants listed in above, which ones will destroy gram- positive bacteria? Gram-negative bacteria?
|
• All seven chemical disinfectants will destroy BOTH gram-positive and gram-negative bacteria.
|
|
|
Of the 7 chemical disinfectants listed above, which ones will destroy spores?
|
• Only glutaraldehyde (Cidex) and hydrogen peroxide-based solutions will destroy spores.
|
|
|
When is ethylene oxide indicated?
|
• Ethylene oxide is indicated for those objects requiring sterilization that cannot be heated in a steam autoclave
|

