![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
129 Cards in this Set
- Front
- Back
|
What are the two cell lines of the hematopoetic system?
|
Myeloid and Lymphoid lines
|
|
|
Choose myeloid or lymphoid...
...Erythroblast |
Myeloid
|
|
|
Choose myeloid or lymphoid...
...Plasma Cell |
Lymphoid
|
|
|
Choose myeloid or lymphoid...
...Neutrophil |
Myeloid
|
|
|
Choose myeloid or lymphoid...
...Monocyte |
Myeloid
|
|
|
Choose myeloid or lymphoid...
...T-cell |
Lymphoid
|
|
|
Choose myeloid or lymphoid...
...Eosinophil |
Myeloid
|
|
|
Choose myeloid or lymphoid...
...Basophil |
Myeloid
|
|
|
Choose myeloid or lymphoid...
...Mast Cell |
Myeloid
|
|
|
What are some very general causes of cytopenias in peripheral blood?
|
Increased demand/decreased supply.
Decreased hematopoesis. Hoarding (sequestration of platelets in spleen - rare) |
|
|
What are some complications/implications for -cytosis for each cell line?
|
Thrombocytosis = thrombi
Leukocytosis = bacterial infxn; leukemia Lymphocytosis = viral infxn; leukemia Erythrocytosis = increased viscosity; heart and circulatory issues (hypertension) |
|
|
What region(s) of adult long bones has active marrow?
|
at the ends
thin line at diaphysis |
|
|
What tissue can easily be sampled to ascertain the status of bone marrow?
|
blood
|
|
|
Choose myeloid or lymphoid...
...NK cell. |
Lymphoid.
|
|
|
Choose myeloid or lymphoid...
...platlets. |
Myeloid.
|
|
|
What is the production time and half life of a neutrophil?
|
6D production;
6-8hr half life |
|
|
What is the production time and half life of a monocyte?
|
1.5D production;
20h half life |
|
|
What is the production time and half life of a erythrocyte?
|
4D production;
half life of months |
|
|
What is the production time and half life of a platelet?
|
4D production;
10d half life |
|
|
What is the term describing band neutrophils outnumbering segmented neutrophils?
|
Degenerative left shift.
|
|
|
What is the term describing when there are increased band neutrophils?
|
Left shift
|
|
|
What does MCV stand for?
A low MCV is called_________ Normal MCV is called _________ A high MCV is called _________ |
Mean corpuscular volume;
Microcytic Normocytic Macrocytic |
|
|
What does MCH stand for?
|
Mean Corpuscular Hemoglobin
|
|
|
What does MCHC stand for?
|
Mean Corpuscular Hemoglobin Concentration
|
|
|
What cell type should be seen in regenerative anemias?
|
Reticulocytes
|
|
|
What stain is used to visualize reticulocytes?
|
New Methlyene Blue stain
|
|
|
What are some causes of intravascular hemolysis?
|
Osmolarity disturbances
Parasites (protozoal) Toxins Immune mediated (complement) Hemolytic bacteria (clostridium; lepto) Oxidative injury DIC (RBCs hit clots) |
|
|
What are some causes of extravascular hemolysis?
|
Pretty much same as intravascular; just occurs outside of vessel
Lysis can occur in macrophage or endothelial cell |
|
|
What is a major cause of extravascular hemolysis?
|
Immune mediated (tagged by Ab then engulfed by macrophage)
|
|
|
What are terms used to denote hemoglobin content?
|
Hypochromic
Normochromic Hyperchromic |
|
|
What do you look for in horses with regenerative anemia?
|
look for RBC size increase; you WON'T see reticulocytes!
|
|
|
What is pink to red plasma indicative of?
|
hemolysis
|
|
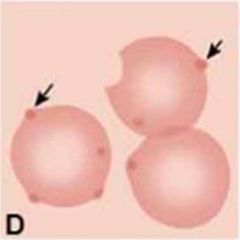
What are the arrows denoting on these RBCs? What is the cause of these?
|

Heinz bodies;
denatured Hb due to oxidative stress |
|
|
What is the proposed toxin in Red Maple Toxicity? What animal does it affect? What organs?
|
Gallic acid causes anemia and nephrotoxicity in horses.
|
|
|
What kind of hemolysis does Anaplasmosis cause?
|
Extravascular hemolysis.
|
|
|
What kind of hemolysis does Babesiosis cause?
|
Intra and extravascular.
|
|
|
What are three possible causes of red to dark red/brown urine? What should plasma look like in each case?
|
Moglobinuria (normal plasma)
Hemoglobinuria (pink/red plasma) Hematuria (normal plasma) |
|
|
At what level does Hb "spill over" into the urine with intravascular hemolysis?
|
150 mg/dl
|
|
|
How does Cu toxicity cause hemolysis? Is it intravascular or extravascular?
|
Oxidative stress on RBCs causes intravascular hemolysis
|
|
|
Where are good regions to sample bone marrow in adult animals?
|
Ends of long bones
Flat bones Sternum & ribs, neck of femur, iliac crest |
|
|
What is the normal ratio of myeloid:erythroid cells in a bone marrow aspirate?
|
2:1 myeloid:erythroid
|
|
|
What are some causes of hypoplasia or aplasia of bone marrow?
|
Viral insults (FeLV, BVDV, Parvo)
Immune-mediated Chemical insults (chemotherapy) Radiation Disease continuum (may sample in type of hypocellularity during "cleanup") |
|
|
T or F:
Bone marrow hyperplasia is a common change. |
True!
|
|

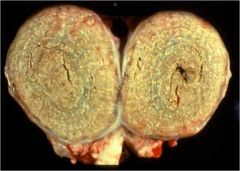
What is the process here?
|

Focus of suppurative osteomyelitis.
|
|
|
What are some rare findings upon examination of a bone marrow aspirate?
|
Lymphocyte clusters
Plasma cells Fibrosis |
|
|
Displacement of marrow cells due to alterations in architecture is known as...
What are common causes of this? |
...myelophthisis;
caused by myelofibrosis or myeloproliferative disease |
|
|
Non-leukemic maturation abnormalities in marrow cells is known as...
What is the outcome of this state? |
...myelodysplasia;
Outcome is marrow failure or neoplasm. |
|
|
This liver protein blocks iron absorption from gut and iron release from storage sites.
|
Hepcidin
|
|
|
What substances upregulate ferritin? What is the result of this upregulation?
|
TNFa and IFNy;
more Fe storage and erythropoesis inhibition |
|
|
What are causes/factors involved in non-regenerative anemia?
|
Fe deficiency
Fe storage (hepcidin; ferritin) Steroid overabundance Lack of stem cells Myelofibrosis/myeloproliferative/myelodysplastic diseases |
|
|
Malignant cells in circulation =
|
Leukemia
|
|
|
What are the types of primary neoplasia affecting bone marrow?
|
Myeloproliferative neoplasia
Lymphoproliferative neoplasia Stromal tumors (more of regular 'ol bone tumors) |
|
|
What is the difference between acute and chronic myelo/lymphoproliferative neoplasia?
|
Acute involves younger cells (more blastic), is more aggressive, shorter clinical course and more responsive to treatment
|
|
|
What causes “punch-out” radiolucent lesions in radiographs?
|
Plasma cell myeloma
|
|
|
What organ(s) are often enlarged in myeloproliferative disease?
|
Spleen and liver
|
|
|
What marker is used to denote T-cells? B-cells?
|
CD3 = T
CD79a = B |
|
|
What develops in the follicular centers of lymph nodes?
|
B cells
|
|
|
What are some causes of small lymph nodes?
|
Atrophy (aging, cachexia, starving)
Hypoplasia (lack of stimulation) Necrosis Immunodeficiency cause |
|
|
What are some causes of lymph node necrosis?
|
Viral (FeLV, BVDV, EHV)
Drugs Severe sepsis |
|
|
What are some causes of big-ass lymph nodes?
|
Hyperplasia
Neoplasia Inflammation Circulatory disturbances (edema) |
|
|
What are hyperplastic causes of lymph node enlargement?
|
Antigenic stimulation (eg: immunization)
Hyperplasia of MPS elements (more filtering or storage) |
|

Name this disease!
Name the agent! What other diseases does this agent cause? |
Caseous lymphadenitis;
Corynebacterium pseudotuberculosis; also causes Pigeon Breast and contagious acne in horses |
|
|
Chronic, suppurative lymphadenitis in a horse is known as...
What is the pathogen? |
STRANGLES;
Streptococcus equi |
|
|
What are signs of chronic lymphadenitis?
|
Lymph node is "fixed" in tissues
Fibrosis May be abscesses present |
|
|
What is the general treatment for any suppurative lymphadenitis? What are common pathogens causing this?
|
Drain the sucka!
Strep. zooepidemicus, Strep. equi, Arcanobacterium pyogenes |
|
|
What agents cause granulomatous lymphadenitis?
What are the characteristic cells? |
Fungi
Mycobacterium Foreign body Parasites Porcine Circovirus (Macrophages and multinucleate giant cells) |
|
|
What kind of lymphadenitis is associated with salmon poisoning, leishmaniasis, and Ehrlichiosis?
|
Histiocytic lymphadenitis
|
|
|
What would a FNA of a hyperplastic lymph node look like?
|
pretty normal
|
|
|
Where does metastatic neoplasia first occur in a lymph node?
|
subcapsular sinus
|
|
|
Regarding staging of neoplasms using a lymph node, what does 1 and 2 mean?
|
1 = lymph node involved but freely movable
2 = enlarged and fixed |
|
|
What are the medullary changes seen in stimulated lymph nodes? What are the names for these changes?
|
B cells migrate to medullary cords = Medullary plasmacytosis
Increased histiocytes in medulla = Sinus histiocytosis |
|
|
What is the most common category of malignancy in the animal kingdom? Which animals is this the MOST common in?
|
Lymphoproliferative disease;
#1 in cats, pigs, sheep, calves #2 in cows common in horses and dogs |
|
|
Why is lymphoma so common?
|
Lymphocytes constantly changing genes to deal w/antigens; leads to mutations.
|
|
|
What are the three classification systems for lymphoma?
|
Anatomic
Histologic Immunophenotype |
|
|
T or F:
Abnormal leukograms in dogs commonly accompany lymphoma. |
False! Often have normal leukograms (80% of dogs do)
|
|
|
What will cytology of a lymph node with lymphoma look like? Histo?
|
Cyto - don't get normal mix of lymphocytes
Histo - uniform population of cells |
|
|
What are the 5 clinical stages of lymphoma?
|
1 - single node involved
2 - 2 or more lnn. in a region 3 - generalized lymphadenopathy 4 - liver and/or spleen involved 5 - bone marrow involved |
|
|
What is the common presentation of canine lymphoma?
|
multicentric enlarged lymph nodes; no leukemia
possibly paraneoplastic effect (hypercalcemia) |
|
|
What is the common presentation of feline lymphoma?
|
alimentary site most common (also nasopharyngeal)
non-regenerative, normochromic, normocytic anemia Typically FeLV |
|
|
What are the two types of Bovine Lymphoma? What is the cause of each?
|
Enzootic - viral (Bovine Leukemia Virus)
Sporadic (not viral) |
|
|
What is the presentation of enzootic bovine lymphoma?
|
multicentric, multifocal LN involvement
persistent lymphocytosis in 30% of animals |
|
|
What are tumor sites for enzootic bovine lymphoma?
|
lymph nodes
heart (right atrium) abomasum (bleeding ulcer) uterus spinal cord (lameness) |
|
|
What are the types of sporadic bovine lymphoma?
|
Calf type - leukemia
Juvenile type - thymic Skin type - adult; slowly progressive |
|
|
What are causes of lymphoma in chickens? What is the pathogen? What cell type is affected?
|
Marek's Disease (herpesvirus) - T-cells
Lymphoid Leukosis (retrovirus) - B-cells |
|
|
What is the test for EIA? What protein is tested for?
|
ELISA and Coggins test; look for p26
|
|
|
What is the main pathogenesis of acute EIA?
|
Lentivirus infection multiplies in tissue macrophages; humoral immunity activated; Ag/Ab complexes; fever/anemia/complement; Fe sequesteration (more anemia); virus controlled until new variant
|
|
|
What are functions of the spleen?
|
Filters blood
White pulp contributes to immune system Fe and blood storage Extramedullary hematopoiesis |
|
|
A brown splenic color change is common in which species? What pigment is responsible?
|
Common in dogs;
caused by hemosiderin |
|
|
What should be found in a blood smear of an EIA infected horse?
|
Sideroleukocytes
|
|

What do you call the plaques depicted here? What is the significance?
|

Siderofibrotic or siderocalcitic plaques;
incidental findings, may be healed lesions from bleeding |
|
|
What are some possible causes for misshapen or small spleen?
|
Congenital anamolies (hyposplenism - rare)
Atrophy Starvation Age-related change Immunodeficiency (reduced wht pulp) Contraction (trauma) Chronic pooling causes ischemia |
|
|
What are some general causes for diffuse splenomegaly?
|
Increased RBCs
Hyperplasia Lymphoma Circulatory disturbances (torsion) Amyloid Inflammation (diffuse) |
|
|
What are some causes of splenic hyperplasia?
|
Extramedullary hematopoesis
Increased lymphatic tissue (due to antigenic stimulation) |
|
|
What are causes of splenomegaly due to increased RBCs?
|
Massive congestion
Barbituate anesthesia |
|
|
Hypersplenism is common in which animal? What process causes hypersplenism?
|
Domestic ferrets;
Spleen sequesters subpopulation of RBCs, causes peripheral cytopenia |
|
|
What are some processes resulting in nodular splenomegaly?
|
Circulatory (incomplete contraction, hematoma)
Focal inflammation Nodular hyperplasia Neoplasia (primary and secondary) |
|
|
What are common causes of nodular splenic hyperplasia?
|
Extramedullary hematopoiesis
Lymphoid hyperplasia |
|
|
How does acute splenitis manifest? How will the cut surface look? What is a pathogen that causes this?
|
Coagulation cascade activated --> blood pooling in spleen;
Cut surface = ooze thick tarry blood Anthrax causes this |
|
|
What is the classic anthrax-caused lesion of the spleen?
|
Blackberry jam lesion
|
|
|
What condition do humans develop with anthrax infection?
|
Hemorrhagic meningitis
|
|
|
What transmissible diseases will cause a hemorrhagic spleen?
|
Yersinia pestis; Y. pseudotuberculosis; Francisella tularensis
|
|
|
What are reservoirs for Francisella tularensis? For Yersinia pestis?
|
F. tularensis = rodent/beaver
Y. pestis = rodent/lagamorph |
|
|
A red, soft splenic tumor would likely be a(n)...
|
Hemangioma/Hemangiosarcoma
|
|
|
A meaty cream to white splenic tumor would likely be a(n)...
|
Lymphoma
|
|
|
A very firm, light colored splenic tumor would likely be a(n)...
|
Leiomyoma/Leiomyosarcoma
|
|
|
What is the function of the thymus?
|
To train retarded T-cells
|
|
|
What are some causes for a small thymus?
|
age
hypoplasia malnutrition toxins |
|
|
What are some causes of a big thymus? Which causes are pretty unlikely?
|
hemorrhage
congenital cysts (rare) inflammation (rare) neoplasia hyperplasia (rare) |
|
|
What are the two types of primary neoplasia possible in the thymus? What species are linked with each?
|
Thymoma (old goats)
lymphoma (cows and young cats) |
|
|
What condition is sometimes linked with a thymoma?
|
Myasthenia gravis
|
|
|
This condition of horses involves deficiencies in B and T cells.
|
Combined Immunodeficiency Disease
|
|
|
What would the expected presentation/findings of a CID horse be?
|
Young arab horse.
Lots of secondary infections. Small, underpopulated lymph nodes, spleen, and thymus. |
|
|
What are common secondary infections in a CID horse?
|
Cryptosporidia
Pneumocystis carnii in lungs |
|
|
Besides CID, what are some other primary immunodeficiencies discussed in class?
|
Chediak-Higashi syndrome
Leukocyte adhesion deficiency Equine aggamaglobinunimea |
|
|
What primary immunodeficiency involves granule defects?
|
Chediak-Higashi syndrome
|
|
|
What primary immunodeficiency involves neutrophilia? What species is this common in?
|
Leukocyte adhesion deficiency; common in Holsteins and Irish Setters
|
|
|
What primary immunodeficiency involves B and T-cell deficiencies? What species is this common in?
|
Combined Immunodeficiency Disease;
mice, bassets, Corgis, Jack Russels, Arabs |
|
|
What primary immunodeficiency involves a B-cell deficiency?
|
Equine agammaglobuminemia
|
|
|
What are some causes of acquired immunodeficiencies?
|
virus
radiation toxins drugs |
|
|
What does MPS stand for (regarding hematopoetic pathology)?
|
Mononuclear Phagocytic System
|
|
|
What domestic species commonly has histiocytic neoplasia?
|
Dogs
|
|
|
T or F:
Histiocytic neoplasia is common in all domestic animal species. |
False! Mostly just dawgs.
|
|
|
What cells can be involved in histiocytic neoplasia?
|
Monocyte
Macrophage Langerhans Cell Dendritic Cell Histiocyte |
|
|
Monocytes in the tissues are known as...
|
...Macrophage
|
|
|
A dendritic cell in the skin is...
|
...a Langerhans cell
|
|
|
A large phagocytic interstitial cell of the reticuloendothelial system; a macrophage of the CT is...
|
...a Histiocyte
|
|
|
What is another name for a benign langerhans tumor? What is its common presentation?
|
Cutaneous histiocytoma; young dogs
|
|
|
What is another name for a non-neoplastic langerhans cell proliferation? What is its common presentation?
|
Cutaneous histiocytosis; Bernese Mtn. Dogs
|
|
|
What malignant neoplasia of macrophages or dendritic cells often involves the spleen? What is a common histological finding?
|
Histiocytic sarcoma; commonly see erythrophagocytosis (macrophage form)
|

