![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
156 Cards in this Set
- Front
- Back
|
What is the first identifiable stage in RBC erythropoiesis? |
Rubriblast
|
|
|
Which developmental stages in erythropoiesis are normally anuclear?
|
Erythrocyte |
|
|
What is the difference between a Polychromatophilic RBC and a Reticulocyte?
|
Reticulocyte is stained with new methylene blue stain; Polychromatophilic RBC is stained with a Wright's stain |
|
|
A retained nuclear fragment in a normally anuclear erythrocyte is a __________________.
|
Howell-Jolly Body
|
|
|
In which stage of erythropoiesis does hemoglobin development begin?
|
Rubricyte
|
|
|
What is the trigger for erythropoietin production? What organ produces this?
|
Hypoxia is detected by the JGA in the kidney to release erythropoietin
|
|
|
What are 5 conditions where nucleated RBCs may be seen?
|
Regenerative anemia |
|
|
What factors influence RBC deformability? |
surface:volume ratio |
|
|
T or F: |
Tru dat! |
|
|
What metabolic pathway protects Hgb from oxidative stress? What molecule provides this protection? What happens if there's a problem with the pathway? |
Pentose Phosphate Pathway produces NADPH which protects from oxidative stress
Heinz bodies form |
|
|
Which pathway prevents overaccumulation of methemeglobin? |
Methemeglobin reductase pathway |
|
|
Choose left shift or right shift...
...due to increased Hgb affinity for oxygen. |
left shift
|
|
|
Choose left shift or right shift...
...results in increased availability of oxygen to the tissues. |
right shift
|
|
|
Choose left shift or right shift...
...due to decreased Hgb affinity for oxygen. |
right shift
|
|
|
Choose left shift or right shift...
...results in reduced oxygen availability to the tissues. |
left shift
|
|
|
Choose left shift or right shift...
...increased pH |
left shift
|
|
|
Choose left shift or right shift...
...decreased pH |
right shift |
|
|
Choose left shift or right shift...
...increased temperature |
right shift
|
|
|
Choose left shift or right shift...
...decreased temperature |
left shift
|
|
|
Choose left shift or right shift... |
left shift |
|
|
Choose left shift or right shift...
...increased DPG (diphosphoglycerate) |
right shift
|
|
|
Choose left shift or right shift...
...decreased CO2. |
left shift
|
|
|
Choose left shift or right shift...
...increased CO2. |
right shift
|
|
|
Which organ is chiefly responsible for Fe storage?
|
Liver
|
|
|
Body Fe regulated by rate of ________; not ________.
|
Body Fe regulated by rate of absorption; not excretion |
|
|
What regulates the rate of Fe absorption?
|
Fe stores and erythropoiesis rate
|
|
|
What are the four methods of evaluating Fe levels?
|
Serum Fe |
|
|
transferrin + iron =
|
serum iron |
|
|
total iron binding capacity is the same as...
|
...serum transferrin |
|
|
how much transferrin is bound to iron is also known as...
|
...% saturation of transferrin
|
|
|
the circulating storage pool of Fe is... |
...serum ferritin |
|
|
What is the most common cause of hypoferremia?
|
chronic low-level blood loss |
|
|
Which of the following would be expected clinical data in cases of hypoferremia due to chronic blood loss?
Low serum Fe Low TIBC Low serum ferritin |
Low serum Fe
Low serum ferritin (should see HIGH OR NORMAL TIBC) |
|
|
Which of the following would be expected clinical data in cases of hypoferremia due to inflammation?
Low serum Fe Low TIBC Low serum ferritin |
Low serum Fe
Low TIBC (should see HIGH serum ferritin) |
|
|
What is a clinical measurement of transferrin?
|
TIBC (total iron binding capacity)
|
|
|
What triggers erythrocyte breakdown?
|
Changes in cell membrane (less deformable)
Cell enzymes |
|
|
What cells remove most RBCs from circulation? Where are these cells located? |
Macrophages in spleen |
|
|
What is the relative proportion of intra vs. extravascular hemolysis in a non-pathogenic system?
|
10% intravascular
90% extravascular |
|
|
What are two good clinical indicators of increased intravascular hemolysis?
|
Hemeglobinuria |
|
|
Name a ton of tests that can be used for erythron evaluation! |
RBC count
PCV Hgb measurement Morphology Retic count Coomb's test Indices (MCH, MCHC, & etc) |
|
|
T or F:
PCV = Hematocrit |
False! The values are usually the same or similar but they are arrived in a different manner (PCV via capillary tube and Hematocrit via instrumental counting) |
|
|
What is a good rule of thumb in estimating target hemoglobin concentration?
|
Hgb in g/dl should be ~1/3 the hematocrit % in mammals.
|
|
|
Name two findings that will impact the accuracy of the hemoglobin concentration.
|
Lipemia
Heinz bodies |
|
|
What are the 2 methods for conducting a RBC count?
|
Flow cytometry (light scatter)
Impedence cytometry |
|
|
Which two RBC indices provide indications of RBC population cell size?
|
MCV (mean corpuscular volume)
RDW (red cell distribution width) |
|
|
Which two RBC indices provide indications of RBC population hemoglobin? How do these differ?
|
MCH (mean corpuscular hemoglobin) - uses Hgb and RBC count
MCHC (mean corpuscular hemoglobin concentration) - uses Hgb and PCV |
|
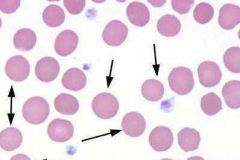
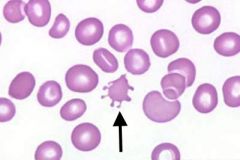
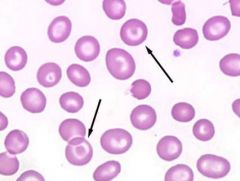
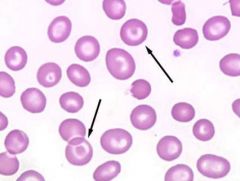
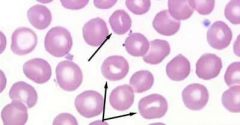
What RBC morphology is indicated by the arrows? What condition(s) are associated with these cells?
|
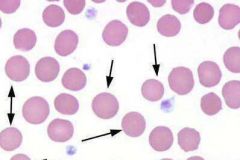
Spherocytes;
Indicative of immune-mediated hemolytic anemia |
|

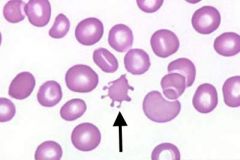
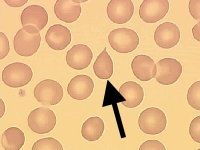
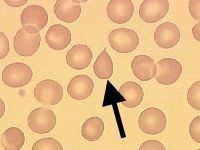
What kind of RBC is indicated by the arrow? What condition(s) are associated with this? |

Schistocytes;
DIC, Vasculitis, and Hemangiosarcoma |
|
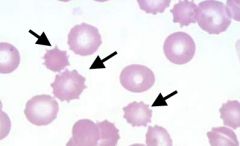
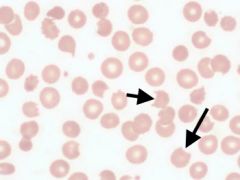
What kind of RBC is indicated by the arrows? What condition(s) are associated with this?
|
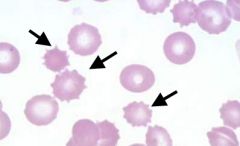
Echinocytes; |
|
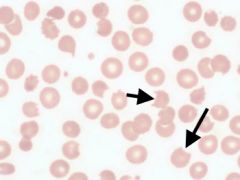
What kind of RBC is indicated by the arrow? What condition(s) are associated with this?
|
Acanthocyte; |
|
What kind of RBC is indicated by the arrows? What condition(s) are associated with this?
|
Keratocytes (blister and helmet cells); |
|
What kind of RBC is indicated by the arrow? What condition(s) are associated with this?
|
Codocytes (target cells); |
|
What kind of RBC is indicated by the arrow? What condition(s) are associated with this? |
Dacryocyte;
Artifact or myelopathy |
|
What kind of RBC is indicated by the arrow? What condition(s) are associated with this?
|
Stomatocyte; |
|
|
What are the two types of Reticulocytes? Which one is unique to cats? |
Punctate (cats) |
|
|
What index takes into account reticulocyte production/maturation time? What value is considered regenerative?
|
RPI (reticulocyte production index); RPI>2 = regenerative |
|
|
T or F: |
True!
Hemolytic recycles raw materials. |
|
|
How long does it take to make a reticulocyte? When are peak values usually found?
|
48-72h production time;
7d peak |
|
|
T or F:
Dogs generally have more reticulocytes than cats. |
True!
<1% dogs; <0.4% cats |
|
|
T or F: |
False!
It can also indicate inadequate response time (haven't made any yet). |
|
|
Which test is used to test for immune-mediated hemolytic anemia? |
Coomb's test
|
|
|
T or F:
Macrocytic hypochromic anemia is a common finding in iron-deficiency anemia. |
False!
This is typical of regenerative anemia! |
|
|
In terms of laboratory data, how can anemia from internal hemorrhage be discerned from anemia due to external hemorrhage?
|
External hemorrhage would also be hypoproteinemic
|
|
|
In a case of hemolytic anemia, predict the values of the following indices: |
PCV - low
Reticulocytes - high Protein - normal |
|
|
List some possible causes of hemolytic anemia.
|
Immune-mediated |
|
|
What are some examples of parasite-induced hemolytic anemia?
|
Mycoplasma haemofelis
M. haemolamae M. haemominitum Babesia canis Anaplasma marginale |
|
|
What are some examples of hemolytic anemia due to oxidative damage?
|
Garlic/onion toxicity
Red maple toxicity Cu toxicosis Acetaminophen toxicity |
|
|
Which of the following is lacking with ineffective or reduced erythropoiesis?
a) stem, progenitor, and precursor cells b) stimulating/growth factors c) nutrients (eg: Fe) d) microenvironment |
One or more are lacking.
|
|
|
What are some differentials for normocytic, normochromic anemia with normal neutrophils and platelets?
|
Renal failure (no erythropoietin)
Anemia of chronic disease/inflammation FeLV-associated anemia Immune-mediated |
|
|
What are some differentials for normocytic, normochromic anemia with decreased neutrophils and platelets (pancytopenia)?
|
Infectious anemia
Radiation Toxins/drugs idiopathic Myelophthsis anemia |
|
|
What are the two major lines of leukocytes?
|
Lymphoid and Myeloid |
|
|
What cytokines stimulate neutrophil production?
|
GM-CSF, G-CSF, and IL-3
|
|
|
What are the stages of neutrophil development?
|
Myeloblast, promyelocyte, myelocyte, metamyelocyte, band nutrophil, segmented neutrophil
|
|
|
What are the two pools of neutrophil population?
|
Marginated and circulation
|
|
|
How long do neutrophils spend in circulation?
|
~10h
|
|
|
What are neutrophils called in fish, birds, and reptiles?
|
heterophil
|
|
|
Macrophages in circulation are called…
|
monocytes
|
|
|
How long does it take for monocytes to mature? How long do they circulate?
|
24-36h; 24h circulation
|
|
|
Which leukocyte can have stormy blue cytoplasm, vacuoles, and/or pseudopods?
|
monocytes
|
|
|
What cytokine stimulates eosinophil produciton?
|
IL-5
|
|
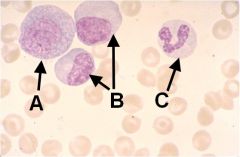
Identify these cells (note, they are all various stages of the same type of cell).
|
A - Promyelocyte; B - Myelocyte; C - Seg. Neutrophil
|
|
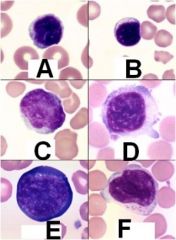
What type of cell is depicted here? ID the species of A-D. ID the specific subtype of E and F.
|
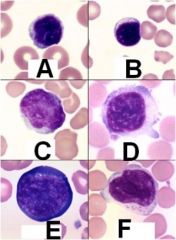
A - Canine Lymphocyte; B - Feline Lymphocyte; C - Equine Lymphocyte; D - Bovine Lymphocyte; E - Reactive Lymphocyte; F - Granular (NK cell) lymphocyte
|
|
|
What is the production time for eosinophils? How long do they remain in circulation?
|
2-6d production; 1hr circulation
|
|
|
What is unique about horse eosinophils?
|
large granules (raspberry eosinophil)
|
|
|
What is unique about cat eosinophils?
|
rod-shaped granules
|
|
|
Which species can have vacuolated eosinophils?
|
Dogs (greyhounds)
|
|
|
What is the production time for basophils? How long do they last in circulation? How long in the tissue? |
2.5d production; 6h in circulation; 2wks in tissues
|
|
|
T or F: Eosinophils and basophils are stimulated by the same chemokines.
|
False! Eosinophils are stimulated by IL-5; Basophils by IL-3
|
|
|
Which species has indistinct basophil granules?
|
Canine
|
|
|
Which species has lavender/gray basophil granules?
|
Feline
|
|
|
What are the smallest leukocytes?
|
Lymphocytes
|
|
|
Describe a reactive lymphocyte.
|
Larger and bluer than normal lymphocyte
|
|
|
What structure indicates that a lymphocyte is antibody producing? What type of lymphocyte is this?
|
White golgi body indicates Ab production of PLASMA CELL
|
|
|
What are lymphocytes with magenta granules?
|
NK cells
|
|
|
Which leukocyte is mostly nucleus?
|
Lymphocytes
|
|
|
What can distort a leukogram?
|
Nucleated RBCs
|
|
|
Which type of neutrophil has a kidney shaped nucleus?
|
Metamyelocyte
|
|
|
What is the difference between a left shift and a degenerative left shift?
|
Both have significant #s of immature neutrophils; in degenerative L shift, immatures outnumber matures
|
|
|
What is the prognosis for animals exhibiting a degenerative left shift?
|
Piss poor
|
|
|
Why is a degenerative left shift not bad in ruminants?
|
They have small marrow pool so initial response appears degenerative.
|
|
|
Marked neutrophilia coupled with a left shift describes…
|
Leukemoid reaction
|
|
|
What are causes of neutrophilia?
|
Physiologic,
corticosteroids, inflammatory, hemolysis or hemorrhage, Myeloproliferative dz |
|
|
Release of epinephrine causes what type of neutrophilia? In which species is this common?
|
Epi releases marginated neutrophils (physiologic neutrophilia); common in foals and cats; also releases lymphocytes
|
|
|
What are the hallmarks of a stress leukogram?
|
Neutrophilia, lymphopenia, eosionpenia, monocytosis
|
|
|
What can cause neutropenia due to increased margination?
|
Endotoxemia (gram neg bacteria)
|
|
|
What are causes of neutropenia?
|
increased margination; increased demand; decreased production; immune mediated; myelophthisis
|
|
|
What are causes of monocytosis?
|
Stress leukogram; chronic/acute inflammation
|
|
|
What are causes of eosinophilia?
|
Parasitic infection; hypersensitivity; idiopathic; tumor; hypoadrenocorticism
|
|
|
What are causes of eosinopenia?
|
Stress leukogram!
|
|
|
What are causes of basophilia?
|
similar to eosinophilia!
|
|
|
What is the difference between a basophil and a mast cell?
|
Basophil has a lobed nuc; mast cell has a round nuc.
|
|
|
What are causes of lymphocytosis? |
Physiologic; antigenic stimulation; Bovine Leukemia Virus
|
|
|
What infectious agents can result in lymphocytosis?
|
Rickettsial disease (erlichia); Bovine Leukemia Virus
|
|
|
What are causes of lymphopenia?
|
Stress leukogram; immunosuppression; immunodeficiency; lymph loss (uncommon)
|
|
|
What causes the presence of toxic neutrophils?
|
inflammatory mediators affecting bone marrow
|
|
|
What are some hallmarks of toxic neutrophils?
|
Increased basophilia to cytoplasm; toxic granules; Dohle bodies
|
|
|
What are Dohle bodies?
|
Bluish aggregates of RER found in toxic neutrophils
|
|
|
What are examples of vacuolation defects in neutrophils?
|
Chediak-Higashi Syndrome; neutrophil anamoly of Birman cats; storage diseases
|
|
|
What neutrophil abnormality can be mistaken for a left shift?
|
Pelger-Huet Anamoly
|
|
|
What are causes of neutrophil hypersegmentation?
|
Old blood; corticosteroids; poodle bone marrow dyscrasia
|
|
|
Which leukocytes can contain intracytoplasmic organisms?
|
Monocytes and neutrophils
|
|
|
What are some examples of intracytoplasmic organisms that can be found within leukocytes?
|
Erlichia; Hepatozoon; Bacteria; viral inclusions; Histoplasma; Leishmania
|
|
|
what two things does erythropoietin stimulate? |
hemoglobin synthesis erythroid cell maturation |
|
|
a defect in a glycolytic enzyme leads to... |
hemolytic anemia |
|
|
with intravascular hemolysis, hemoglobin become_____ and binds to _______. if the _______ capacity is exceeded then they're filtered out through the glomerulus |
dimers haptoglobin haptoglobin |
|
|
if the binding capacity of haptoglobin is exceeded, unbound hemoglobin can be either ______ or when uptake capacity is exceeded, ______ |
resorbed excreted as free hemoglobin |
|
|
in what species is rouleaux formation normal? in what is it abnormal and what does it indicate? |
normal= horses and cats dogs= inflammatory disease |
|
|
names three species that have poikolocytes in a healthy animal |
calves pigs goats |
|
|
what is basophilic stippling? name two scenarios in which it is scene? |
RNA clumps seen with a WRIGHT'S stain
seen with: 1. lead poisoning 2. regenerative anemia of sheep, cats, and cattle |
|
|
anemia due to hemorrhage or hemolysis will be either _____cytic and _____chromic or ____cytic and ______chromic |
macrocytic and hypochromic normocytic and normochromic |
|
|
anemia due to blood loss and accelerated RBC destruction tend to be ________ anemias |
regenerative |
|
|
reduced or defective erythropoiseis tend to be _______ anemia |
non regenerative |
|
|
name some clinical signs/lab findings that would help you distinguish intravascular hemolysis from extravascular |
both have icterus and bilirubinuria intravscular will also have hemoglobinemia and hemoglobinria |
|
|
what are the hallmarks of immune mediated hemolytic anemia? |
marked regenerative anemia
sometimes you see auto-agglutination in the sample tube (small speckle/clumps of blood) |
|
|
what does insulin and hemolytic anemia have to do with each other? |
insulin drives phosphorus into the cells, causes hypophosphatemia, and causes hemolysis |
|
|
the cytokine ______ is responsible for the liver's production of ______ during anemia of chronic disease |
IL-6 Hepcidin |
|
|
name two causes for relative polychthemia |
dehydration splenic contraction |
|
|
how do activated platelets stick to the vessel wall? |
von willebrand's factor |
|
|
what is the end result of secondary hemostasis? |
fibrin |
|
|
true or false: secondary hemostasis and fibronlysis are triggered at the same time |
true |
|
|
what is the precursor to fibrin? |
fibrinogen |
|
|
who breaks down fibrin? |
plasmin |
|
|
what are the degradation of fibrin? |
D dimers |
|
|
what test assesses intrinsic coagulation pathway? extrinsic? |
intrinsic-PTT extrinsic- PTT |
|
|
true or false: vessels normally produce activators of blood coagulation |
false, normally produce inhibitors |
|
|
what is thrombopoesis? |
platelet formation |
|
|
what's the name for a "platelet" in a bird and reptile? |
thrombocytes |
|
|
what is the most common reason for non-regenerative anemia? |
anemia of chronic disease |
|
|
what type of tube do you put a bone marrow sample into? |
EDTA |
|
|
what are two things that you can glance for to see that you've actually gotten a bone marrow sample? |
megakaryocytes fat |
|
|
what cells are seen with acute leukemia? chronic leukemia? |
acute--very immature blast cells chronic--mature cells, small, look actually pretty normal |
|
|
define myelodisplastic syndrome |
cells made in bone marrow that are not maturing normally (ineffective hematopoesis) |
|
|
where does lymphoma start? |
in solid tissues CAN go to bone marrow but doesn't start in bone marrow |
|
|
what are some things you can do to further diagnose cells in acute lymphocytic leukemia? |
immunophenotyping PCR |
|
|
chronic lymphocytic leukemia can often be confused with..? |
reactive lymphocytosis |
|
|
to diagnose multiple myeloma, you need two of four diagnostic features. name the four |
monoclonal gammopathy bence-jones proteinuria radiographic evidence of osteolysis plasma cells in the bone marrow |

