![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
30 Cards in this Set
- Front
- Back
|
Discuss the paper on NAC by Cuzzocrea et al.
|
From the Brit J. Pharm, 2000, this italian study used a 2vo mong gerbil model to demonstrate that NAC 20mg/kg IP resulted in decreased CA1 death, dec nitrotyrosine, mda, and myeloperoxidase, and improvement in motor function.
|
|
|
Discuss the paper on NAC by Sekhon et al.
|
From Brain Res 2003. The authors, from the Medical Univeersity of South Carolina, used pre-treatment with NAC, 145mg/kg IP, to decrease stroke volume in a rat model of focal ischemia, in accordance with Krause’s Law. Neurological score was improved. Additionally, the authors demonstrated decreased production of TNF-α and iNOS.
|
|
|
Discuss the paper on thiol homeostasis by Shivakumar et al.
|
This 1995 Indian study, published in J Pharm Ther, can probably be considered a relatively seminal influence for this topic. Moderate and severe brain ischemia both resulted in loss of GSH, with associated increases in MDA and ROS and loss of enzyme function. However, moderate ischemia and resultant recovery was associated with rapid restoration of thiol homeostasis, whereas severely ischemic animals never regained thiol homeostasis and subsequently died. Maximal loss of GSH was observed in striatum and hippocampus. This suggests that GSH was there to be lost, and unless it is transported into neurons there must be endogenous neuronal glutathione reductase. Alternatively, one supposes that GR in associated glia may be responsible for maintaining CA1 thiol homeostasis. Either way, adminsitration of NAC may be helpful.
|
|
|
What is the importance of the recent paper by Franco et al?
|
This 2007 Brazilian paper published in Life Sciences, evaluated the effect of MTPT in various brain regions. Its primary interest to us is the demonstration of the presence of Glutathione reductase activity in hippocampus.
|
|
|
What is the actual technical term for glutathione?
|
Gamma-glutamylcysteinylglycine.
|
|
|
Draw glutathione.
|
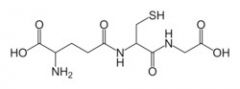
glutathione:
|
|
|
How does NAC work, in a nutshell?
|
It is converted to cysteine, and is thus a donator of sulfhydryl groups that can be incorporated (as cysteine) into glutathione. (Does this happen in hippocampus?)
|
|
|
What is (probably) the most critical enzyme in GSH synthesis?
|
Gamma-glutamylcysteine synthase. This enzyme is rate-limited by the availability of cysteine (a role for NAC) and is feedback-inhibited by the presence of GSH.
|
|
|
Summarize the first Chan-Hayashi paper on oxidative damage to ER.
|
Oxidative damage to the endoplasmic reticulum is implicated in ischemic neuronal cell death. Hayashi and Chan et al, JCBFM 2003. Chan et al induced global brain ischemia on wild-type and SOD1 transgenic rats and compared ER stress and neuronal damage. Phosphorylated forms of eIF2 alpha(P) and PERK, both of which play active roles in apoptosis, were increased in hippocampal CA1 neurons after ischemia but to a lesser degree in the transgenic animals. This finding, together with the finding that the transgenic animals showed decreased neuronal degeneration, indicates that oxidative ER damage is involved in ischemic neuronal cell death. binding with and oxidative ER protein modification. ER luminal were oxidatively modified and stagnated in the ER lumen, and GRP78 was detached from PERK by ischemia. All of these effects were attenuated by SOD1 overexpression. The authors propose that ROS attack and modify ER proteins and elicit ER stress response, which results in neuronal cell death.
|
|
|
Summarize the important literature on selenium in cerebral ischemia.
|
Selenium is an important antioxidant, and an essential cofactor for glutathione peroxidase. In 1997, Takasago et al demonstrated that the organoselenide ebselen reduced infarct volumes in focal ischemia. In 1998, the Ebselen Study group in Osaka showed that early tx with ebselen improved outcome at one month, but not three months. In 2001 a Scottish team demonstrated that ebselen reduced both gray and white matter damage and that this was probably through antioxidant action.
|
|
|
How might injury to the electron transport chain result in increased superoxide production?
|
Superoxide is a natural by-product of respiration, accounting for up to 1% of mitochondrial oxygen consumption. Interrupting electron flow by damaging one of the components of the ETS results in a “buildup” of e- proximal to the “occlusion” leading to increased acceptance of e- by oxygen and increased superoxide.
|
|
|
What are some of the methods Gary Fiskum proposes for reduction of oxidative stress in brain injury?
|
Mild uncoupling, pharmacologic inhibition of the mitochondrial permeability transition (MPT) by agents like 2-APB, and simply lowering the inspired fraction of oxygen.
|
|
|
How does Gary Fiskum think “mild uncoupling” works?
|
“When electron flow is only partially inhibited, the redox-mediated stimulation of ROS production can be counteracted by mild uncoupling agents. Mitochondrial ROS production is extremely sensitivie to inhibition by slight depolarization and oxidized shift in redox state at high membrane potential. Thus a drop of only a few mV reduces the rate of NADH-linked, substrate-dependent ROS formation by 50% with little effect on ATP production.” Fiskum et al, 2004.
|
|
|
What does Gary Fiskum think about the role of Bcl2 in mitochondrial oxidative stress?
|
Overexpression of Bcl-2 appears to increase mitochondrial hydrogen peroxide production. This suggests that Bcl-2 overexpression may exert a “preconditioning”-like effect, causing the increased expression of antioxidant enzymes.
|
|
|
Who described the “coil” method of focal brain hypothermia? Discuss the method.`
|
Clark and Colbourne, JCBFM, 2007. Used a simple 20Ga needle constructed from a hypodermic needle, implanted beneath the temporalis muscle and flushed with cold water, to induce focal unilateral brain hypothermia. No effect on core temp, HR or MABP. Can be used in conscious animals.
|
|
|
Can you cite the spanish paper in which the authors showed that the cumulative neuroprotective effect of multidrug therapy and hypothermia was greater than hypothermia alone? What were the drugs, and what was the model?
|
The paper was by Sanchez-Casado et al (2007). The model was global ischemia (10 min) and the drugs were magnesium and trilizad.
|
|
|
In a recent AEM paper, who investigated the difference between 33c and 35c hypothermia? What did they find? What was their model?
|
Logue and Callaway demonstrated that the benefit of induced hypothermia at 35C appears to be similar to the benefit of 33C. This was a global ischemia (asphyxial arrest) model.
|
|
|
Describe the method used by Colbourne et al for monitoring and inducing hypothermia.
|
Colbourne is pretty intense about hypothermia. He uses implanted abdominal and cerebral biotelemetry devices, hooked up to a system of UV lamps and water misters to control brain temperature within 0.5C. This system could cost as much as $100,000 and is probably beyond the resources of most labs (including ours, at the moment).
|
|
|
Describe the paper on hypothermia by Kollmar et al published in 2007.
|
Published in Stroke, this paper used MCAO occlusion in rats, and evaluated various outcomes, including TUNEL and neuroscore, at 24 hours and 5 days after varying degrees of hypothermia. The authors found that 34deg C was the optimal temperature for therapeutic hypothermia…in focal ischemia…in rats.
|
|
|
Summarize the findings of the Hypothermia after Cardiac Arrest Study Group.
|
This European paper, published in the NEJM in 2002, randomized patients to normal tx vs. hypothermia, 32-34C for 24h. Patients with hypothermia had decreased mortality, decreased neuro deficit, and no increase in side effects.
|
|
|
Describe the 2002 Australian study of hypothermia.
|
This small paper, published by Bernard et al in the NEJM, demonstrated that patients txd with hypothermia after out-of-hospital arrest were 5x more likely to have a good outcome, and with no increase in side effects.
|
|
|
Describe the Brongholi paper on glutathione levels during hypoxia.
|
Hippocampal slices exposed to OGD, followed by reperfusion, showed increased SOD activity and reduced GSH levels accompanied by reduced glutamate uptake, with decreased cell viability and hippocampal degeneration.The decrease of GSH could be attributed to conjugation of GSH to lipid-derived oxidation products, conversion to reversible or irreversible forms, increased efflux, or pertrubation in GSH synthesis, include a decrease in Na-dependent cysteine uptake. The decreased glutamate reuptake was not affected by administration of DTT (an exceptionally strong reducing agent).
|
|
|
What is a potential mechanism for the role of NAC in blunting excitotoxicity?
|
Zhang et al (for detail see below) demonstrated that NAC administration inhibits the assembly of a GluR6-PSD-95-MLK3 signaling module during cerebral ischemia in rat hippocampus. In this model, ischemic stress induces the formation of an mGluR6-PSD95-MLK3 complex, with disinhibiton and autophosphorylation of MLK3, and subsequent phophorylation and activation of JNK3, with pro-apoptotic transcriptional effects.
|
|
|
Briefly discuss the 2007 JCBFM paper on LPS-mediated ischemic preconditioning.
|
Rosenzweig et al show that LPS admin 72 hr prior to MCAO ischemia reduced infarct size and correlated with dec TNF signaling. Although LPS raised TNF levels and TNFR and other signaling components early, by the time of the injury the TNF signaling had been “down regulated.” This paper supports a role for extinsic apoptotic processes in focal ischemic stroke.
|
|
|
The refrig-a-RATor relies on a direct carotid cooling approach. Who wrote the theoretical paper that seems to validate the approach? Where was it published and when?
|
Wang and Zhu, at U of Md, in Eur J Appl Physiol, 2007.
|
|
|
Describe, in a nutshell, the theoretical model used by Wang and Zhu to investigate the carotid cooling approach.
|
The theoretical model involves mathematical representations of the neck (in xyz?) and the head in cylindrical coordinate systems. (Fig 1) The differential change in temperature along the carotid can then be modeled, roughly, as: deltaT/t = constant*(heat flow to tissue + heat flow to device)-heat convection due to blood flow. (Equation 1) And the differential change in temperature in the brain (head, actually) can be modeled, roughly, as: deltaT/t = constant*(heat flow to cold neck + head cond from tissue) + heat convection due to blood flow. (Equation (2)
|
|
|
What were Wang and Zhu’s findings vis-à-vis their theoretical carotid cooler?
|
Temperature falls along the length of the carotid artery in contact with the device, from 37 to 34.2 C if the device is at 5C on its surface (Figs 2 and 3).Temperatures in the brain tissue equilibrate (and uniformly, at that) at about 34.5 C, which is within the therapeutic range (Fig 4). The efficiency of the device in causing a temperature gradient along the artery diminishes sharply if the distance between the artery and the device is increased (Fig 5). What a shocker. Similarly, a shorter device results in less cooling (Fig 6). Another big surprise. The temperature decay along the artery is sensitive to the temperature of the cooling device, although perhaps not as much as one might think (Fig 7). Blood flow in vessels other than the carotid do not have a big impact on the efficiency of the device (Fig 8). Cooling should occur fairly quickly (Figs 10 and 11).
|
|
|
Why is Imoto’s study of peltier chips in neocortical seizures only nominally applicable to our RRR?
|
Had to use an external cooling system.
|
|
|
Discuss, briefly, the structure and function of HIF-1.
|
Hypoxia-inducible factors (HIFs) are transcription factors that respond to changes in available oxygen in the cellular environment, in specific, to decreases in oxygen, or hypoxia. The alpha subunit of HIF-1 is a target for prolyl hydroxylation by HIF prolyl-hydroxylase, which makes HIF-1 α a target for degradation by the E3 ubiquitin ligase complex, leading to quick degradation by the proteasome. This occurs only in normoxic conditions. In hypoxic conditions, HIF prolyl-hydroxylase is inhibited, since it utilizes oxygen as a cosubstrate. HIF-1, when stabilized by hypoxic conditions, upregulates several genes to promote survival in low-oxygen conditions. These include glycolysis enzymes, which allow ATP synthesis in an oxygen-independent manner, and vascular endothelial growth factor (VEGF), which promotes angiogenesis. HIF-1 acts by binding to HIF-responsive elements (HREs) in promoters that contain the sequence NCGTG.
|
|
|
Discuss the 2002 Danish paper on insulin + tPA in stroke.
|
This Danish paper evaluated the therapeutic effect of insulin alone or insulin combined with 30 min delayed thrombolytic therapy in rats embolized in the right hemisphere with a fibrin clot made from autologous blood. The authors concluded that insulin treatment aiming at blood glucose levels around 2-4 mmol l(-1) was detrimental to clinical outcome causing significantly increased mortality. However, this study suffers from several problems: First of all, the range of infarct volumes in this model was HUGE. For example, in controls the median infarct volume was 24%, but the RANGE was 4% to 51%. In the tPA group, the range was 1%-80%. Furthermore, of the 14/60 rats that died spontaneously, only 8 could be analyzed post-morten. Finally, we don’t know why those animals died—in spite of the fact that their infarcts weren’t all that different. The authors think it may have been hypoglycemia, but they have no data either way. In summary, this study suffers from technical problems not uncharacteristic of the embolic MCAO models.
|

