![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
57 Cards in this Set
- Front
- Back
|
Imaging Modalities
|
•Magnetic Resonance Imaging (MRI)
MR Venography and Angiography, Diffusion and Perfusion MRI, MR Spectroscopy and Functional MR. •Computed Tomography (CT) CT perfusion and CT Angiography •Cerebral Angiography •Nuclear Medicine PET/CT & SPECT |
|
|
How MR works?
|
•MR Radio frequencies are used to excite tissue in the presence of a strong magnetic field. The resulting resonance frequencies are then collected and digitally processed.
|
|
|
Contrast In Meuroimaging
|
•Iodinated contrast in CT
•Gadolinium in MRI •Used to demonstrate breakdown in the blood brain barrier •Demonstrate tumours, infection and vascular lesions |
|
|
CT advantages
|
•Easily available
•Rapid imaging •Better at detecting blood •Evaluates fine bone detail and calcium better than MRI |
|
|
MRI advantages
|
•No radiation
•Good spatial resolution •Multiplanar •Multiple sequences allow varying image contrasts to be achieved •Anatomic and Physiological imaging |
|
|
Dangers of MRI
|
can;t raise the temp on any one area by more than 1 degree (only danger in MRI) or metal in them we dont know of
|
|
|
MRI SEQUENCES
|
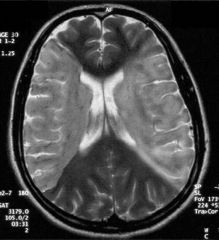
•There are > 200 sequences
•T1 : fat is bright, CSF black. •T2 : CSF bright •Flair: CSF black, however bound water is bright (depresses the CSF so that pathology is bright) •Diffusion: infarcted tissue bright |
|
|
Neuroangiography
|
Visualize lesions in vessels including atherosclerotic plaques, stenosis, aneurysms, and arteriovenous malformations. Invasive procedure requiring insertion of a catheter through the femoral artery up to the carotid
- digitally subtract away the bone - morbidity (stroke) 1 in 1000 - mortality 1 in 100, 000 |
|
|
CATHETER ANGIOGRAPHY Pros and Cons
|
Advantages
•High spatial resolution •Prelude to intervention Disadvantages •Invasive with significant morbidity and mortality |
|
|
MR Angiography & Venography
|
DISADVANTAGE: u see all the vessels at one go
|
|
|
Physiological Imaging of Brain Lesions
|
Diffusion weighted Imaging (DWI): cellularity
Perfusion weighted Imaging (pMRI); Haemodynamics MR spectroscopy (MRS) & PET: Metabolism |
|
|
MR spectroscopy indication
|
- ID a mass in the brain, need to biopsy
- undertake a MR spec scan to ID the most metabolically active area (worst area) for the location of biopsy sample - if the area is not metabolically active at all then it could simply be an area of necorsis (eg. radiation) |
|
|
Stroke Epi
|
•Cerebral Infarctions 3rd most common cause of death.
•75% occur in the territory of the MCA •50,000 Australians per year affected •75% survive but 50% require long term care RULE OF 1/3 |
|
|
Role of Imaging in stroke
|
•Confirm Diagnosis
•Triage for therapy Exclude haemorrhage Assess damage, location, pattern and extent Salvageable Brain ? CT perfusion or MR perfusion •Follow outcome |
|
|
Acute Stroke
|
within 3hrs to rule out haemorrage and qualify for thrombolysis and EXCULDING MIMICS
•85% Ischaemic & 15% Haemorrhagic •However 40% of CT scans are normal in the first 6hrs and over 60% of scans may be normal in the first 3hrs •Mimics include :- Migraine, Seizures, infection, demyelination and mass lesions (DDx) |
|
|
Goals of Stroke Imaging 4P’s
|
•Evaluation of Parenchyma
–Non contrast CT or MR •Evaluation of Pipes –CT or MR angiography •Evaluation of Perfusion –CT perfusion or MR perfusion •Evaluation of Penumbra –CT perfusion |
|
|
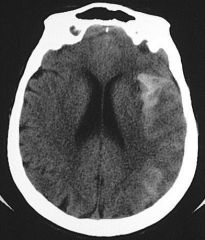
1. Evaluation of Parenchyma
EARLY CHANGES |
Earliest changes seen on CT Reflect changes in the water content of the brain due to evolving cytotoxic oedema
- loss of gray white junction, loss of definition of Basal ganglia, insular ribbion, internal capsule - hyperdense MCA sign |
|
|
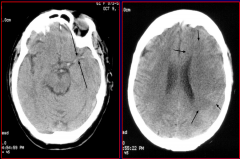
EARLY CT CHANGES
- cerebral oedema - mass effect |
Sulcal effacement
Ventricular distortion |
|
|
Earliest changes seen on MRI
|
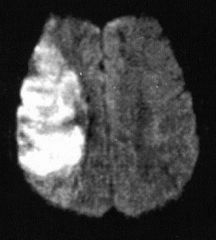
•Diffusion restriction within 30 mins of event, maybe earlier.
•Cytotoxic oedema swelling of gray matter increased signal intensity on T2 & FLAIR •Loss of intravascular flow voids |
|
|
Stroke (subacute changes)
|
•Increased mass effect first 3 days. CT shows wedge shaped infarct involving both grey and white matter.
•Haemorrhagic transformation may occur 1 to 14 days following infarction. •Other types of haemorrhagic infarction include laminar necrosis and venous infarction. |
|
|
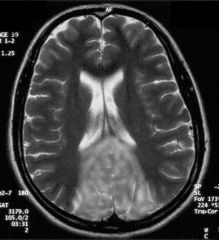
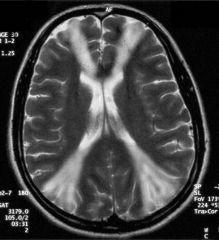
MCA Territory
|
|
|
|
ACA Territory
|
|
|
|
PCA Territory
|
|
|
|
Watershed Infarction
|
low BP and diseased aa. and then suddenly drop BP by tiny amounts (in old diseased people first- in young people need a massive drop in BP)
So those areas furtherest away affected first - this image between the MCA & ACA territories |
|
|
CT scan in the posterior fossa
|
- poor due to the thickness of the petrous temporal bone thus use an MRI for anything there esp if a suspected brainstem infaract
|
|
|
3. Evaluation of Perfusion
|
•Brain is continuously perfused by 15 -20% of Cardiac output ~ 800mls/min.
•Cerebral blood volume CBV in mls/100g of tissue •Cerebral blood flow CBF in mls/100g/min •Mean Transit time MTT :- time between arterial flow and venous return. •CBF = CBV/MTT |
|
|
2. evaluation of pipes:
Neuroangiography at different time phases |
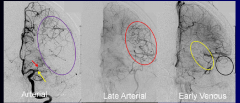
1. arterial
2. late arterial 3. early venous |
|
|
CT Perfusion
|
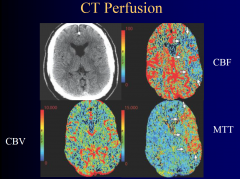
|
|
|
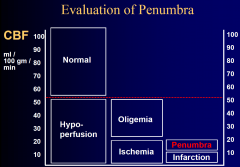
4. Evaluation of Penumbra
|
|
|
|
Penumbra
|
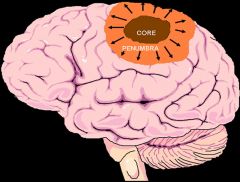
In pathology and anatomy the penumbra is the area surrounding an ischemic event such as an ischemic, thrombotic or embolic stroke.
|
|
|
Venous Haemorrage
|
spill over into tissues
- the haemorrage isnt in a known arterial location think venous |
|
|
Extradural Haematoma
|
•“D” shaped or convex shape
•Often associated with a skull fracture •Usually due to arterial bleeding - medical emergency - large aa. torn and blood fills quickly with no time to compensate. ticking time bomb, and once the brainstem enters the foreamen magnum its gameover |
|
|
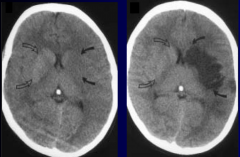
Subdural Haematoma
|
•“C” or crescent shaped
•Commonly due to tearing of venous structures •Occurs more slowly and is more common in cerebral atrophy massive but not as big emergeny (its happened over days, some blood is bright (acute) the other is hypodense (same as the CSF or brain) thus weeks old blood) |
|
|
Subarachnoid Haemorrhage
|
•Haemorrhage into the subarachnoid space which may be due to
•Aneurysm rupture •Trauma POORLY defined |
|
|
Nontraumatic Intracerebral Haemorrhage
|
•Aneurysm or vascular malformation rupture
•Hypertension •Venous thrombosis •Amyloidosis •Neoplasia •Anticoagulation therapies |
|
|
Infection/Inflammation
|
- temporal lobes
- bilateral think herpes - abcess can cause a necrotic core (DDx necrotic tumour) - multiple lesions in the lungs or brain think miliary TB |
|
|
Low Grade Tumours
|
- margins defined
- contrast enhancement |
|
|
High Grade Tumours
|
poorly defined
- cross midline (with corpus collsum) - oedema |
|
|
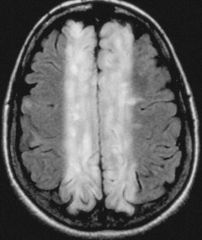
White matter lesions
|
- MS
- lesions perpendicular to the lateral ventricles - lots of demylinating plaques |
|
|
Usefulness of CT
|
- poor resolution in brain imaging
- useful for quick ID of bleeds |
|
|
MR vs CT
|
- more detail
- functional imaging possible - expensive - slow image acquisition |
|
|
T1 & T2
|
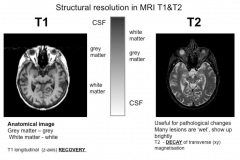
|
|
|
the stronger the magnet....
|
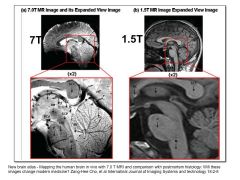
|
|
|
DTI
|
- diffusion of protons depends on freddom of movement in tissue
- membranes restrict movement - location and direction of fibre tracts can be determined in vivo by DTI, allowing tract tracing in live humans FRACTIONAL ANISOTROPY: FA 0- water moves freely (eg CSF) FA 1- highly restricted water movement |
|
|
DTI image
|
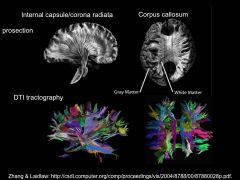
|
|
|
PET
|
detects gamma ray emitted from injected radionucleotide tracer
- FDG most commonly used in neuroimaging - taken up like normal G but not metabolised |
|
|
PET test design
|
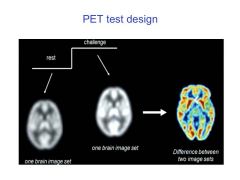
|
|
|
PET pros and Cons
|
Pros:
- non-invasive - specific functional signficance - multiple isotopes Cons: - no temporal resolution - low spatial resolution - radioactive |
|
|
Functional MRI
- BOLD |
- differences in blood flow (due to differing behaviours of oxygenated & deoxygenated blood in a big magnet
|
|
|
BOLD MOA
|
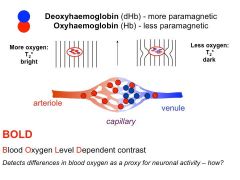
- dHb deflect magnetic fields
- BOLD functional MR only detects blood flow through small vessels |
|
|
Local Blood Oxygenation and Neuronal Activity
|
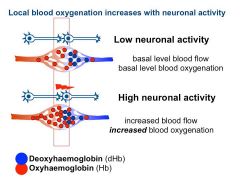
|
|
|
BOLD overview
|
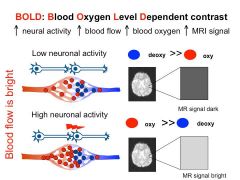
|
|
|
BOLD Signal intensity curve
|
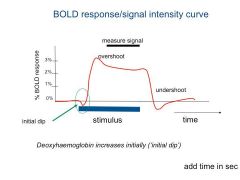
|
|
|
How to make use of fMRI
|
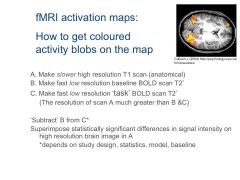
|
|
|
Time resolution tradeoff
|
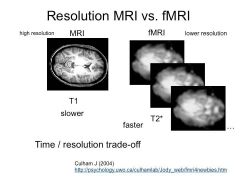
|
|
|
fMRI Pros and cons
|
Pros:
- good spatial resolution - good temporal resolution - non-invasive & no radioactive compunds - repeat scanning possible Cons: - noisy - motion artifact - bone and airspace artifacts - metal objects |
|
|
Diffuse Optical tomography (DOT) or InfraRed Optical imaging (IROI)
|
Essentially BOLD imaging, infrared light passed into brain, optical absorption of haemoglobin
Not yet in common clinical use for brain, verification and standardisation in progress Potential advantages Good for children – quiet, mobile Allows active behaviour during scan Can be worn continuously Potential for intraoperative imaging Very fast – time resolution high Spatial resolution still low but improving |

