![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
128 Cards in this Set
- Front
- Back
|
* The correct order of physical assessment is.. – A. Palpation, inspection, percussion, auscultation – B. inspection, palpation, percussion, auscultation – C. inspection, auscultation, percussion, palpation – D. Inspection, percussion, palpation, auscultation |
B. inspection, palpation, percussion, auscultation |
|
|
What parts of the hands are used in palpation? |
– Fingertips: finetactilediscrimination – Opposition of finger and thumb: position, shape and consistency of an organ or mass – Dorsa (back) of hand: temperature |
|
|
What is inspection? |
Inspection: critical observation of the patient in a systematic, deliberate manner. – Concentrated watching – General survey |
|
|
What is palpation? |
use of touch to determine: – size, texture, consistency , and location of body parts. Temperature, moisture, change in size, vibrations, pulsations, rigidity or spasticity, crepitation, presence of lumps or masses, and the presence of tenderness or pain. – Use different parts of the hands – Light v. deep palpation |
|
|
What kinds of palpation are there? |
Light: surface characteristics and areas of tenderness Deep: palpate an organ or mass Bimanual: envelop or capture certain body parts |
|
|
What is percussion? |
striking a part of the body with short, sharp taps of the finger. Location, size, position, and density of the underlying organs. Thorax and abdomen |
|
|
What kinds of percussion is there? |
– Direct Percussion • for Adult sinuses – Indirect Percussion • Strike interphalangeal joint (short fingernails are a must!!!) |
|
|
What are the characteristics of percussion notes? |
• Resonant • Hyperresonant • Tympany • Dull • Flat |
|
|
What is auscultation? |
Listening to sounds produced by the body |
|
|
How is auscultation performed? |
With an unassisted ear - speech, - percussion tones - difficult breathing - coughing - loud abdominal sounds With a stethoscope (or doppler) - heart - lungs - abdomen |
|
|
When you do a general survey of a person, what do you look for? |
• Physical Appearance – Age, gender, skin color, facial features • Body Structure – Stature, nutrition, symmetry, posture, body build • Mobility – Gait, range of motion • Behavior |
|
|
What is recommended for weight? |
– Recommended range for height – Add 10% for client with larger frame |
|
|
How do you take a height measurement? |
• Wall Mounted Device – Shoeless, standing straight and looking straight ahead. Feet, shoulders and buttocks should be in contact with the hard surface. |
|
|
How is BMI (Body mass index) calculated? |
• BMI: marker of optimal healthy weight for height – Healthy = level of 19 - 25.
|
|
|
What influences temperature? |
• Diurnal cycle • Menstrual cycle • Exercise • dehydration • faulty thermometer • environment • infections |
|
|
What are the routes of temperature measurement and what are the norms for those routes? |
• Oral (Normal 98.6) • Tympanic membrane thermometer (TMT) (99.5) |
|
|
What is axillary? |
Under the arm (arm pit) |
|
|
What is tympanic? |
Eardrum |
|
|
What is stroke volume? |
The amount of blood pumped into the aorta with each heart beat (typically around 70mL). |
|
|
How is the stroke volume palpated? |
In the wrist, arm, neck, leg or ankle as the pulse. |
|
|
What kind of pulse rhythms are there? |
- regular - irregular |
|
|
Describe the pulse rate. |
– Varies with age – Normal 50-90 beats per minute (bpm) • Bradycardia <50 • Tachycardia >90 |
|
|
In taking a pulse, what should be measured? |
- Rate - Rhythm - Force |
|
|
How is the pulse force recorded? |
– 4 point scale – 2+ ......Normal – 0 .......Absent |
|
|
How can pulse be described? |
- springy - straight - resilient |
|
|
What factors influence pulse rate and rhythm? |
- Drugs - pathology - exercise - age - gender - temperature - BP - serum electrolytes |
|
|
When measuring respiration, what is recorded? |
- rate - pattern - depth |
|
|
What is the normal respiration for a 1 year old? |
20 - 40 respirations/ min |
|
|
What is the normal respiration for an adult? |
10 - 20 respirations/ min |
|
|
What is the definition of blood pressure? |
Pressure of the blood against the wall of the blood vessels. |
|
|
What are the factors that influence blood pressure? |
- Disease - drugs - anxiety - Cardiac output - peripheral resistance - arterial elasticity - blood volume - blood viscosity - Age - weight - exercise |
|
|
What is the math problem that produces blood pressure? |
CO (cardiac output) X SVR (Systemic Vascular Resistance) = BP (blood pressure) |
|
|
How does cardiac output affect BP? |
Increased CO, increases BP |
|
|
How does vascular resistance affect BP? |
Increased VR (vasoconstriction), increased BP |
|
|
How does volume affect BP? |
Increased volume, increased BP |
|
|
How does viscosity affect BP? |
Increased viscosity, increased BP |
|
|
How does elasticity of the arterial walls affect BP? |
If the arterial walls are rigid, such as from arteriosclerosis, it increases BP |
|
|
How should the blood pressure cuff fit the patient and what are the results if it doesn't fit? |
It should cover 50% of the limb from the shoulder to the olecranon process. If it is too narrow, there will be an abnormally high reading and it's too wide, there will be an abnormally low reading. |
|
|
What are the blood pressure levels? |
Normal <120 <80 Prehypertension 120-139 80-89 Stage 1 hypertension 140-159 90-99 Stage 2 hypertension >or= 160 >or=100 Hypotension <95/60 |
|
|
What is normal Oxygen Saturation with the Pulse Oximeter? |
97% - 100% |
|
|
What affects oxygen saturation with the pulse oximeter? |
- Smoking makes it falesly high - false nails - nail polish - can use toes - can use earlobe - readings are altered in low perfusion states |
|
|
What is orthostatic hypertension? |
When the blood pressure drops when raising from a lying or sitting position. |
|
|
What patients would you worry about having orthostatic hypertension? |
- someone you would expect volume depletion - person known to have hypertension or is taking antihypertensive meds - a patient reporting fainting or syncope |
|
|
Why would you need to take a blood pressure on a thigh? |
- the arms aren't available - if the arm BP is excessively high |
|
|
How does the blood pressure differ in a thigh from an arm? |
Systolic BP may be 10-40mm Hg higher in the thigh as well as the diastolic BP |
|
|
What is a doppler and what does it do? |
- it enhances the pulse and BP when it can't be heard - it only gives a systolic reading - you hear a "whooshing" pulsatile beat |
|
|
What might be some characteristics observed in the elderly patient? |
- kyphosis (hunched over) - gait disturbances |
|
|
What might be some characteristics of the vital signs of the elderly patient? |
- normal temperature is often lower - pulse is typically 50-90bpm and slightly irregular - respiration is typically shallow and increased in rate - typically an increase in systolic pressure, therefore, there is a widened pulse pressure |
|
|
The force or strength of a pulse: A. is usually recorded on a 1-2 point scale B. Is a reflection of the heart's stroke volume C. Demonstrates elasticity of the vessel wall D. Reflects the blood volume in the arteries during diastole. |
B. Is a reflection of the heart's stroke volume. |
|
|
What is the pulse pressure? |
The difference between the systolic and diastolic pressures. |
|
|
What is mental status? |
Emotional and cognitive functioning. |
|
|
What is a mental disorder? |
- An organic disorder due to a brain disease of a known origin - A psychiatric mental illness with an organic etiology that has not been established |
|
|
Give an example of an organic disorder due to a brain disease of known origin. |
- Deliruim - Dementia - Alcohol and drug intoxication or withdrawal |
|
|
Give an example of a psychiatric mental illness. |
- Anxiety disorder - schizophrenia |
|
|
Mental Status is inferred through individual's behaviors. Which behaviors? |
- Consciousness - language - Mood and affect - Orientation - Attention - memory - abstract reasoning - thought process - thought content - perceptions (TOMCAT LAMP) |
|
|
What is consciousness? |
Being aware of one’s own existence. Most elementary of mental status functions. |
|
|
What is language? |
Using voice to communicate |
|
|
What is mood and affect? |
- Prolonged display of feelings |
|
|
What is orientation? |
The awareness of the objective world in relation to the self |
|
|
What is attention? |
The power of concentration. |
|
|
What is memory and what are the two kinds? |
The ability to lay down and store experiences and perceptions for later recall. - Recent memory is day to day events - Remote memory is years' worth of experiences |
|
|
What is abstract reasoning? |
Pondering a deeper meaning beyond the concrete and literal. |
|
|
What is the thought process? |
The logic train of thought. The way a person thinks. |
|
|
What is thought content? |
What the person thinks – specific ideas, beliefs, the use of words. |
|
|
What are perceptions? |
An awareness of objects through the 5 senses |
|
|
What can affect mental status? |
Age related changes in sensory perception, like vision or hearing loss, as well as loss of loved ones, loss of income or job status, physical changes related to aging (a weaker body) and a fear of the loss of life. |
|
|
When should a full mental status examination be performed? |
When there are - behavior changes - brain lesions (trauma, tumor, CVA, stroke) - aphasia secondary to brain damage - symptoms of psychiatric illness, especially with acute onset |
|
|
What kind of posture would be considered "normal"? |
Erect and relaxed. |
|
|
What kind of posture would be considered "abnormal"? |
- Curled in bed - tense muscles - frowning - restless pacing - slow walk - dragging feet. |
|
|
What kind of body movements would be considered normal? |
- voluntary - deliberate - coordinated, - smooth and even |
|
|
What kind of body movements would be considered abnormal? |
- Restless - fidgety - hyperkinetic - apathy and slowing - abnormal posturing |
|
|
What dress would be considered normal? |
- Appropriate for setting, season, age, gender - fits and put on appropriately |
|
|
What dress would be considered abnormal? |
Eccentric dress, bizarre makeup (manic syndrome) |
|
|
What kind of hygiene would be considered abnormal? |
- Disheveled appearance in a previously well-groomed person. - May reflect economic status or trend, not mental status. |
|
|
What does CVA stand for? |
Cerebrovascular accident |
|
|
What kind of behavior would be considered normal? |
- awake, alert - facial expression appropriate to the situation - speech is fluent, articulate, converses easily |
|
|
What is dysphonia? |
Any disturbance of normal vocal function. |
|
|
What is dysarthria? |
Any of certain disorders of articulation, as stammering or stuttering, caused by a nerve defect. |
|
|
In a mental status examination, what cognitive functions would be examined? |
- orientation - attention span - recent memory - remote memory - new learning - judgement |
|
|
In a mental status examination, how would you determine if the patient is oriented? |
If the patient knows: - the time: day of week, date, year, season - place: where they live, present location, type of building, name of city and state - person: own name, age, who the examiner is and type of worker |
|
|
In a mental status examination, how would you determine if the patient has an attention span? |
It would be noticed through normal conversation or could be given a series of directions. |
|
|
In a mental status examination, how would you determine if the patient has recent memory? |
They could be asked what they've eaten in the last 24 hours or asked when they arrived at the hospital, something that can be corroborated. |
|
|
In a mental status examination, how would you determine if the patient has remote memory? |
Could be asked about verifiable past events. |
|
|
In a mental status examination, how would you determine if the patient is capable of new learning? |
The 'four unrelated words test' could be performed. |
|
|
In a mental status examination, how would you determine if the patient is capable of proper judgement? |
- job plans - social or family obligations - plans for the future (Should be realistic) |
|
|
Name a supplemental mental status examination. |
The mini cog |
|
|
What is the mini cog? |
A supplemental mental status exam, a simple screening tool, that takes 3 to 5 minutes to administer. It detects cognitive impairment quickly. It is appropriate to use in all settings. |
|
|
What levels of consciousness would be considered abnormal? |
- alert - lethargic - obtunded (between lethargy and stupor - sleeps most of the time, difficult to rouse) - stupor or semi-coma - coma - acute confusional state (delirium) |
|
|
What is considered a 'stupor' or semi-coma? |
Spontaneously unconscious, responds only to persistent and vigorous shake or pain, has appropriate motor responses (withdraws hands to avoid pain) |
|
|
How does a coma present? |
Completely unconscious, no response to pain or to any external or internal stimuli (when suctioned does not try to push the catheter away) - light coma has some reflex activity but no purposeful movement - deep coma has no motor response |
|
|
How does acute confusional state, or delirium, present? |
Clouding of consciousness, impaired recent memory, agitated and having visual hallucinations. |
|
|
What would be considered abnormalities of mood and affect? |
- Flat affect (blunted affect) - Depression - Depersonalization (lack of ego boundaries) - Elation - Euphoria - Anxiety - Fear - Irritation |
|
|
What are the goals of a nursing pain assessment? |
Describe the patients pain experience in order to identify and implement appropriate pain management techniques Identify the patient’s goal for therapy and resources for self-management. |
|
|
What is the definition of pain? |
Whatever the patient says it is. Exists when he/she says it does. What the patient says is considered the most reliable indicator. It is an unpleasant sensory and emotional experience. |
|
|
What is the patient right when it comes to pain? |
Patients have the right to appropriate assessment and management of pain. |
|
|
How does pain in different patients differ? |
Different patients experience different levels of pain in response to comparable stimuli. Patients with chronic pain may be more sensitive to pain and other stimuli. |
|
|
What can unrelieved pain do? |
Unrelieved pain has adverse physical and psychologic consequences. Acute pain that is not adequately controlled can result in physiologic changes that increase the likelihood of developing persistent (chronic) pain. |
|
|
When the cause for pain is difficult to assess, what is important to remember? |
Pain can exist even when no physical cause can be found. Do not attribute pain that does not have an identifiable cause to psychologic causes. |
|
|
What is important for a nurse to remember regarding pain thresholds? |
A uniform pain threshold does not exist. It varies among everyone for many different reasons. Encourage patients to report pain, in particularly, ones that won't discuss it, or deny pain when it is likely present. |
|
|
What is important for a nurse to remember regarding pain in patients that cannot communicate? |
Special considerations are needed for obtaining pain assessment data for them. Include family members in the assessment process (in particularly mothers of young patients). |
|
|
What are the two types of pain? |
- nociceptive pain (Nerve fibers in periphery and CNS are functioning and intact) - can turn into neuropathic over time - neuropathic pain (atypical pain, includes missing limb pain and neuropathy) |
|
|
Regarding time, what types of pain are there? |
- acute (short term, self-limiting, predictable trajectory) - chronic (or persistent)(6 months or longer - malignant or nonmalignant) - breakthrough pain (pain starts before the next analgesic dose |
|
|
In pain assessment, what aspects are we assessing? |
- pattern - location - intensity - quality - associated symptoms - management strategies - impact on the patient's life
|
|
|
When assessing pain pattern, what do we ask? |
- when did it start (onset) - how long as the pain lasted (duration) - what may have caused it (OCD -onset, cause, duration) |
|
|
What is incident pain? |
Pain that increases due to an event such as a dressing change or a catheter insertion. |
|
|
When assessing pain location, what do we ask? |
– “Describe the site of the pain” – “Point to the painful area on the body” – “Mark painful area on the pain map” |
|
|
What can make locating pain be difficult? |
- Referred pain (a site different than the affected site) - Radiating pain (such as down an arm from MI) |
|
|
When assessing pain intensity, what does it mean and how do we go about it? |
It is a quantitative assessment of the severity of the pain and we use pain scales adjusted to age and cognitive function in an attempt to do that. |
|
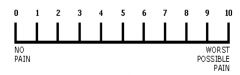
What is this called and who is it used for? |
A numeric pain scale used for adult patients who have full cognitive capabilities. |
|

What is this called and who is it used for? |
Wong-Baker FACES Pain Rating Scale used with children and adults with compromised cognitive capabilities. |
|
|
What is the FLACC pain scale? |
It is a chart with 5 categories to score a pain scale of 0 to 2 of patients who cannot communicate. It uses facial expressions and various activities to try and assess their level of pain. |
|
|
How do we assess quality of pain? |
- a description of the pain - neuropathic pain is usually described as burning, numbing, shooting, stabbing, or electric shock- like, or an itchy sensation - nociceptive pain may be described as sharp, aching, throbbing, dull and cramping. |
|
|
How do we assess associated symptoms of pain? |
Anxiety, fatigue, depression may exacerbate or be exacerbated by pain. We ask what activities increase or alleviate pain |
|
|
When assessing a patient's management strategies, what do we ask? |
“What strategies are you using now and what have you used in the past?” This refers to: - prescription and nonprescription medications - non-drug therapies such as hot and cold - complementary or alternative techniques such as acupuncture, herbal remedies and relaxation. |
|
|
When assessing the impact pain has had on a patient, what should be asked? |
What effect has the pain had on the patient’s ability to sleep, enjoy life, interact with others, perform work and household duties. |
|
|
When assessing a patient's pain, why do we take into account their beliefs, expectations and goals? |
Because some beliefs may hinder effective treatment (i.e. the belief that opioid use may result in addiction) or be wrong (i.e. 'I'm just getting old' or 'God's punishing me') |
|
|
When regarding pain, why is it critical to document when using a tool for pain assessment? |
To ensure effective communication among team members. Be sure they are all "on the same page". |
|
|
Why is reassessment of pain important? |
It is critical to reassess pain at appropriate intervals to be sure that the patient's pain is addressed. Reassessment of a postoperative patient is done within 30 minutes of an IV dose of an analgesic. It's important to know if it's working |
|
|
What is a good way to remember the areas of pain assessment? |
P - Provocative (or palliative) - what makes it better or worse Q - Quality or Quantity R - Region or radiation S - Severity Scale: 1 to 10 T - Timing or onset U - Understand the patient's perception of the pain or problem |
|
|
How does pain differ in the elderly? |
- pain is a common experience in the elderly but is NOT part of the aging process - it is wrong to assume that pain should be expected in the elderly and pain should always be addressed. |
|
|
How does pain differ in the genders? |
- men are more stoic - women are more prone to migraines, fibromyalgia, and are more sensitive to pain during the menstrual cycle |
|
|
• Pain signals are carried to the CNS by way of – A. Efferent sensory fibers – C. Abberrant sensory fibers |
B. Afferent sensory fibers |
|
|
• Neuropathic pain implies which of the following. A. An abnormal degree of pain interpretation B. An abnormal processing of the pain message C. An abnormal transmission of pain signals D. An abnormal modulation of pain signals. |
B. An abnormal processing of the pain message |
|
|
• Specialized nerve endings that are designed to detect painful sensations are: – A. Synapses - D. Nociregulators |
C. Nociceptors |
|
|
• Which of the following is the most reliable indicator for chronic pain? – A. MRI results – C. Tissue enzyme levels |
– B. Patient self-report |
|
|
• Deep somatic pain originates from sources in which of the following locations. – A. Skin and SQ tissues – C. Mediastinum |
– B. Bones and joints |
|
|
A person has just now exercised. What do you expect has happened to their vital signs? |
- higher temperature - higher BP (higher CO) - faster pulse (higher heart rate) |
|
|
A person is dehydrated. What do you expect has happened to their vital signs? |
- higher temperature - lower BP (lower CO) - faster pulse (higher heart rate) |

