![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
97 Cards in this Set
- Front
- Back
|
What are intracellular uses of calcium ion? (4) |
- signal transduction - enzyme action - muscle contraction - exocytosis |
|
|
What are extracellular uses of calcium ion? (6) |
- nerve and muscle excitability - membrane permeability - blood coagulation - maintenance of tight junctions - synaptic transmission - functional integrity of bones and teeth |
|
|
What muscle condition can occur with hypocalcemia? |
tetany |
|
|
What percentage of calcium in the body is in bone and what percentage is in plasma/interstitial fluid? |
99% in bone 1% in plasma/interstitial fluid |
|
|
What happens to calcium binding as pH increases?
decreases? |
low pH = acidosis = more free calcium ion
high pH = alkalosis = less free calcium ion |
|
|
How is calcium absorbed from the lumen of the small intestines? |
diffusion and active transport
(only active transport is hormonally regulated) |
|
|
What fraction of ingested calcium is absorbed? |
1/3 |
|
|
What percentage of blood calcium ion is reabsorbed? |
99% |
|
|
What part of the nephron absorbs most of the blood calcium? |
proximal tubule (60%) |
|
|
What part of the nephron regulates rate of calcium reabsorption? |
distal tubule |
|
|
Describe the two calcium pools in bone |
Stable calcium pool-slow exchange rate due to remodeling
Labile calcium pool-rapid exchange from readily available pool |
|
|
What are the 4 phases of bone remodeling? |
1) Activation 2) Resorption 3) Reversal 4) Formation |
|
|
Describe the activation stage of bone remodeling. |
Osteoclast precursors are activated from hematopoietic stem cells in plasma and differentiate into osteoclasts in response to RANKL, cytokine, and M-CSF released from osteoblasts.
|
|
|
What 2 kinds of receptors do osteoclasts express for recruitment, differentiation, and activation? |
RANK and calcitonin receptors |
|
|
Describe the bone resorption phase of remodeling. |
Osteoclasts fuse and form a seal around bone. They then release H+ to dissolve calcium and phosphate ions and enzymes to degrade the remaining protein matrix. |
|
|
How long does bone resorption take? |
2-4 weeks |
|
|
Describe the reversal stage of bone remodeling. |
An unknown signal is given to go from bone resorption to bone formation. |
|
|
Describe the formation stage of bone remodeling. |
Osteoblasts first secrete osteoclast-activating cytokines and then osteoprotegrin (ODP)
Osteoblasts then synthesize alkaline phosphatases and osteoid matrix proteins
They then express PTH and D3 receptors |
|
|
What is osteoprotegrin? |
It is a decoy molecule that competes with RANKL and ultimately suppresses osteoclast formation and function |
|
|
How long does bone formation take? |
4-6 months |
|
|
Where is the labile calcium pool found? |
It is bone fluid that surrounds osteocytes in cannaliculi, sealed under osteoblasts, and under bone-lining cells. |
|
|
What effect do PTH and Vitamin D3 have on osteocytes? |
They stimulates osteocytes to take up calcium ion and transfer it to blood vessels of bone and surface osteoblasts. |
|
|
What causes bone fluid to flow? |
mechanical stress |
|
|
What does shear stress cause a release of? |
RANKL (to activate osteoclasts) |
|
|
What enzyme inhibits osteoblast function? |
sclerostin |
|
|
What is the major method of phosphate ion absorption? |
Ingestion |
|
|
What is the primary method to control phosphate levels? |
renal reabsorption |
|
|
What hormones regulate calcium homeostasis? (7) |
- Parathyroid hormone (PTH) - Vitamin D3 (aka Calcitriol) - Calcitonin - Sex steroids - Growth Hormone and IGF-1 - Glucocorticoids - Thyroid hormones |
|
|
What is PTH's function? |
to increase plasma calcium ion levels and reduce plasma phosphate ion levels |
|
|
What secondary messenger does PTH affect? |
cAMP |
|
|
When is PTH released? |
In response to small changes in plasma calcium concentrations |
|
|
What receptor do secretory cells of the parathyroid have to sense plasma calcium ion levels? |
CaSR - Calcium sensing receptor
(G-protein mechanism) |
|
|
What effect does PTH have on osteoblasts? |
Osteoblasts release cytokines to activate osteoclasts (requiring D3) |
|
|
What effect does PTH have on kidneys? |
It increases calcium resorption and decreases phosphate reabsorption |
|
|
Why is it important that both calcium and phosphate be reabsorbed in the kidneys? |
If the concentration of either ion gets too high, it may cause precipitation. |
|
|
What enzyme is activated in kidneys to produce the active form of vitamin D? |
1-hydroxylase |
|
|
What mediates calcium absorption in the gut? |
1, 25 (OH)-Vitamin D |
|
|
What are normal calcium levels in blood? |
9mg/dL +/- 0.5mg/dL |
|
|
What enzyme deactivates 1, 25-(OH) Vitamin D? |
24-hydroxylase |
|
|
What activates 24-hydroxylase? |
High levels of 1, 25-(OH) hydroxylase |
|
|
What transcription factor mediates expression of 1-hydroxylase? |
Vitamin D Receptor (VDR) |
|
|
What affect does 1, 25-(OH) vitamin D have on bone? |
Makes it more reactive to PTH |
|
|
What affect does 1, 25-(OH) vitamin D have on intestines? (2) |
- Increases calcium absorption - Causes synthesis of calcium binding proteins |
|
|
What affect does 1, 25-(OH) vitamin D have on kidneys? |
Has some minor increase in calcium reabsorption |
|
|
What affect does 1, 25-(OH) vitamin D have on lymphatics? |
decreases lymphocytes, lymphokines, and immunoglobulins |
|
|
What affect does 1, 25-(OH) vitamin D have on skin? |
Induces turnover of keratinocytes |
|
|
What cells of what organ secrete calcitonin? |
C-cells of the thyroid gland |
|
|
What effect does calcitonin have on blood? |
Decreases plasma calcium and phosphate ion levels |
|
|
How does calcitonin inhibit osteoclast activity? |
By increasing intracellular cAMP |
|
|
What hormones can stimulate calcitonin release? (2) |
gastrin and estrogen |
|
|
What unusual property does calcitonin have? |
analgesia |
|
|
What is the alternate expression of the calcitonin gene in nerve cells and what does it cause? |
CGRP - vasodilation |
|
|
At puberty, what hypothalamic hormone stimulates an increase in estrogen in girls and testosterone in boys? |
GnRH |
|
|
What hormones initiate long bone growth? (4) |
Estradiol (E2) or Testosterone (T), GH, and IGF-1 |
|
|
What do higher E2 receptors cause at the end of puberty? |
closure of growth plates |
|
|
What does hypogonadism cause during puberty? |
Late growth plate closure, so Pt is short during puberty and tall at the end with disproportionally long limbs |
|
|
What does precocious puberty cause during child development? |
Tall children that do not grow muchduring puberty; short limbs |
|
|
Why does the decrease of estrogen after menopause lead to bone loss? (3) |
Estrogen normally functions to stimulate osteoblast progenitors, increase osteoclast apoptosis, and inhibit cytokine production |
|
|
What hormone determines bone density in men? |
Testosterone |
|
|
What condition can occur with hyperthyroidism? |
Osteoporosis |
|
|
What do high plasma levels of glucocorticoids cause in relation to calcium? |
hypocalcemia |
|
|
How do glucocorticoids cause hypocalcemia? |
Inhibits both calcium reabsorption in kidneys and absorption in gut
Inhibits osteoblasts and vitamin D3 synthesis |
|
|
What causes hypoparathyroidism?
What affect does it have on Ca and PO4? |
- Loss of parathyroid gland function
- Lowered Ca and increased PO4 |
|
|
What causes pseudohypoparathyroidism?
What affect does it have on Ca and PO4? |
- Loss of PTH receptor function
- Lowered Ca and increased PO4 |
|
|
What are some causes of 1, 25-(OH) D3 deficiency? (4) |
- Insufficient sun, malnutrition, malabsorption of D3 - Inadequate enzymatic conversion as seen in liver or kidney disease - Anticonvulsant drugs - Receptor defect |
|
|
What happens to phosphate levels with decreased renal function?
What about 1-OHase activity? |
Increases blood phosphate concentration
Lowers 1-OHase activity |
|
|
What does lower 1-OHase activity lead to? |
Lower Vit D and thus lower blood Ca levels |
|
|
What are the symptoms of hypocalcemia? (4) |
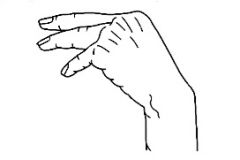
- Hyperactive reflexes, tingling (paresthesia), cramps, and Trousseau's sign - Seizures - decreased heart contractility - tetany (possibly asphyxiation from laryngospasm)
|
|
|
What are some causes of hypercalcemia? (3) |
- Hyperparathyroidism due to tumor of PT gland or ectopic tumor secreting PTH - Excessive ingestion of calcium or Vitamin D - tumors secreting bone-mobilizing substance, PTH-related peptide that cross-reacts with PTH receptors and activates them (called hypercalcemia of malignancy) |
|
|
What are Ca and PO4 levels in someone with hypercalcemia due to a tumor? |
Increased Calcium, Lowered Phosphate |
|
|
What are Ca and PO4 levels in someone with hypercalcemia due to excessive ingestion of calcium or Vitamin D? |
Increased calcium and increased phosphate |
|
|
What are some symptoms of hypercalcemia? (7) |
- Predisposition to kidney stones - Reduced neuromuscular excitability: weakness, fatigue, lethargy - Anorexia, constipation, nausea - Depression, EEG abnormalities, memory and personality changes - Bone weakness, pain, fractures - Peptic ulcers (b/c Ca induces gastrin release) - Calcification of soft tissue - Possible cardiac arrest |
|
|
What percentage of post-menopausal women are osteoporotic? |
20% |
|
|
What are the 3 bones that most commonly fractured due to osteoporosis? |
1) hip 2) vertebrae 3) distal radius |
|
|
What are the consequences of osteoporotic fractures? (4) |
- acute and chronic pain - limitation of physical activity - variable recovery - social isolation / depression |
|
|
What bone fracture has the highest rate of morbidity for the elderly? |
Hip bone |
|
|
Between spongy and compact bone, which one decreases in mass in osteoporotic patients? |
spongy (trabecular) bone mostly, some cortical bone if resorption exceeds formation |
|
|
What is the clinical definition of a patient who is diagnosed with osteoporosis? |
Her/his bone mineral density (BMD) falls 2.5 standard deviations below average |
|
|
What endocrine abnormalities lead to bone loss? (5) |
- Deficiency anywhere in the GH-IGF1 axis (growth hormone - insulin like growth factor 1) - Decreased vitamin D - Decrease in renal 1-hydroxylase activity - Hypercortisolism; hyperthyroidism - Type 1 diabetes |
|
|
When is peak bone mass attained? |
Soon after puberty |
|
|
What behaviors can cause bone loss? (5) |
- Drugs (like synthetic glucocorticoids) - Diet/anorexia, malabsorption diseases - Smoking - Alcohol - Lack of exercise |
|
|
What races are protected from osteoporosis? (2) |
- African-descended - Mexican-descended |
|
|
Why does bone mass decrease with age? |
Loss of sex steroid production with age (in both men and women) |
|
|
Why are there two phases of bone loss in women but only one in men? |
Women have their first significant loss during menopause before they begin to lose hormones due to aging. |
|
|
On what kind of receptor can testosterone act on for osteoblasts and osteoclasts? |
Androgen receptors |
|
|
Between testosterone and estradiol, which steroid has a greater effect on appositional growth? |
Testosterone |
|
|
What is appositional growth? |
Growth of bone from inside the diaphysis usually increasing in thickness |
|
|
Which receptor of estrogen mostly mediates the actions of estradiol? |
ER-alpha |
|
|
How does estradiol suppress bone turnover? (3) |
- Suppresses osteoblastic secretion of cytokines - Increases osteoblast lifespan - Decreases osteoclast lifespan |
|
|
What effect does decreased plasma estradiol levels have on Ca? |
Increases blood calcium |
|
|
Why does a decrease in estradiol levels lead to secondary hyperparathyroidism? |
The body tries to compensate for low calcium levels by increasing parathyroid function due to lack of calcium absorption via gut and increased excretion via kidneys. |
|
|
How long does the rapid phase of bone loss in post-menopausal women last? |
4 years |
|
|
What can prevent the rapid phase of bone loss in post-menopausal women? |
Estradiol supplementation
(but not calcium supplements nor exercise) |
|
|
What occurs in women 10-15 years after menopause? |
Increase in serum PTH in response to low free calcium in blood |
|
|
Does PTH increase in aged men as well? |
Yes |
|
|
What are some treatments for osteoporosis? (3) |
- Estrogen hormone replacement therapy (HRT) - Calcium & Vitamin D supplements - Bisphosphonates
(Prevention is exercising while young) |
|
|
What do bisphosphonates do? |
increase osteoclast apoptosis |

