![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
31 Cards in this Set
- Front
- Back
|
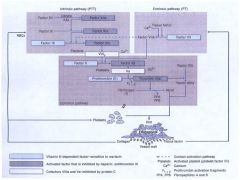
Draw the Coagulation Cascade
|
|
|
|
Name the Antithrombotic Agents
( Anticoagulants) |
Heparin
Low-molecular weight heparins -Enoxaparin -Dalteparin -Tinzaparin Fondaparinux Warfarin (Coumadin) Direct thrombin inhibitors -Bivalirdin -Lepirudin -Argatroban |
|
|
Name the Antithrombotic Agents
(Antiplatelets) |
Aspirin
Dipyridamole Thienopyridines -Ticlopidine -Clopidogrel -Prasugrel Glycoprotein IIb/IIIa Inhibitors -Abciximab -Eptifibatide -Tirofiban |
|
|
Thrombolytic Agents
|
Streptokinase
Urokinase Alteplase (tPA) Reteplase Tenecteplase |
|
|
Drugs to Treat Bleeding
|
Aminocaproic Acid
Protemine Sulfate Vitamin K |
|
|
MOA of Heparin
|
Binds to antithrombin III and catalyzes the inactivation of factors IIa, Xa, IXa, and XIIa.
Factors IIa and Xa most sensitive. *Ternary complex to inhibit factor IIa (requires 18 saccarides)* |
|
|
Monitor Heparin with:
|
APTT
Therapeutic range or 1.5-2.0 x control. |
|
|
MOA of LWMH
|
Just like heparin, but smaller so less Anti-IIa activity compared to Anti-Xa (2:1 to 4:1)
|
|
|
Advantages of LWMH over Heparin
|
-Predictable dose-response anticoagulation
-Increased bioavailability -Longer duration of action -Dose-independent clearance -Decreased incidence of thrombocytopenia -No laboratory monitoring required |
|
|
Fondaparinux
|
A synthetic pentasaccharide with specific anti-Xa activity (via ATIII)
|
|
|
Warfarin
|
Inhibits vitamin K epoxide reductase which results in the loss of carboxylation of factors II, VII, IX, and X so they can't bind Ca++ (only 10-40% as effective)
*Slow onset (5 x 36 hours) |
|
|
How to monitor Warfarin therapy:
|
PT
INR (Normal: .8-1.0, Therapeutic 2.0-3.5) - If INR >9.0 give vitamin K 2.5-5mg PO (INR should decreas in 6-8 hours, 24-48 hours for full effect). |
|
|
Argatroban
|
Small molecule that directly inhibits trombin
*monitor with aPTT and adjust for liver function *Used in patients with HIT. |
|
|
Lepirudin and Bivalirudin
|
Directly inhibit all actions of thrombin by binding in 1:1 molar ratio.
*No antidotes *Monitor with aPTT adjust for kidney disease. |
|
|
Asprin
|
Irreversibly binds to and inactivates COX-1, which prevents production of TXA2
*No effect on activated platelets. |
|
|
Dypyridamole
|
Inhibits phosphodiesterase in platelets
*potentiates de-aggregating effects of prostacyclin. *Little effect by itself, adjunct to warfarin or aspirin. |
|
|
MOA of Thienopyridines
|
Irreversible inhibition of ADP induced platelet activations.
*All must be activated by CYP450 |
|
|
Abciximab
|
Murine monoclonal antibody that inhibits glycoprotein IIb/IIIa
*May cause allergic reactions *Half life is that of platelets. |
|
|
Tirofiban
|
A non-peptide glycoprotein IIb/IIIa inhibitor.
*Half-life of 90-180 mins |
|
|
Eptifibatide
|
Synthetic cyclic heptapeptide glycoprotein IIb/IIIa inhibitor.
*Half life of 1-2.5 hours. |
|
|
MOA of Glycoprotein IIb/IIIa Inhibitors
|
Block glycoprotein IIb/IIIa from binding fibrinogen.
*Platelet function significantly decreased at 50% blockade *Still 80% blockade has minimal effect of bleeding time *>90% blockade gives extremely prolonged bleeding time. |
|
|
Streptokinase
|
Indirect plasminogen activator, converts plasminogen to plasmin.
Low affinity for fibrin (systemic lytic state) *Can cause allergic reaction* |
|
|
Urokinase
|
Naturally occuring plasminogen activator (Produced by the kidneys)
Directly activates plasminogen. Less antigenic than streptokinase Lacks fibrin specificity (Systemic lytic state) |
|
|
Alteplase
|
Tissue-type plasminogen activator
High affinity for fibrin (limits systemic lytic state) |
|
|
Reteplase
|
A deletion mutant variant of tPA that still directly converts plasminogen.
|
|
|
Tenecteplase
|
Multiple point mutations of alteplase
*increased resistance to PAIs and longer half life (18-20 mins) **More fibrin specific that alteplase** Used for acute myocardial infarction. |
|
|
Aminocaporic Acid
|
Competitive inhibitor of plasminogen activators.
|
|
|
Protamine Sulfate
|
Positive charged protein from fish sperm that binds to and inactivated Heparin.
|
|
|
Vitamin K
|
Has something to do with Warfarin : )
|
|
|
Absolute Contraindication to Thrombolytic Use
|
Any prior intracranial hemorrhage
Known structural cerebral vascular lesion (e.g. arteriovenous malformation) Known malignant intracranial neoplasm (primary or metastatic) Ischemic stroke within 3 mo except acute ischemic stroke within 3 hr Suspected aortic dissection Active bleeding or bleeding diathesis (excluding menses) Significant closed-head or facial trauma within 3 mo. |
|
|
Is the intrinsic or extrinsic pathway more important for in vivo coagulation?
|
Extrinsic
*initiated by tissue factor or thromboplastin. |

