![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
98 Cards in this Set
- Front
- Back
|
What are the 2 major types of thrombi?
|
Red and White thrombi
|
|
|
HEMOSTASIS
↓ Initiation of coagulation ↓ Thrombin ↓ Fibrin ↓ Thrombus Stasis of clotting factors |
red thrombus
|
|
|
Where do red thrombi tend to occur?
|
Atria
Veins |
|
|
**Red Thrombi**
Fibrinolysis Immediate anticoagulation (IV) Long term anticoagulation (Oral) Very general tx of what? |
DVT
|
|
|
**Red Thrombi**
Immediate anticoagulation(IV) Long term anticoagulation (oral)*** Very general tx of what? |
Atrial Fibrillation
|
|
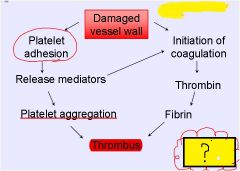
What's being formed here?
|
White Thrombus
|
|
|
Where do white thrombi tend to occur?
|
Arteries
|
|
|
A-Fib & DVT
White or Red Thrombus? |
Red Thrombus
|
|
|
STEMI, NSTEMI/Unstable angina/Percutaneous coronary intervention (PCI)
White or Red Thrombus? |
White Thrombus
|
|
|
What do you target to stop the effects of Red Thrombi?
|
Thrombin
Thrombus |
|
|
What do you target to stop the effects of White Thrombi?
|
Platelet Aggregation
Thrombus Thrombin |
|
|
What is the main difference between
the pharmacological treatment of STEMI and NSTEMI? |
Use of Thrombolytics for STEMI (total occlusion of vessel)
We don't want to use thrombolytics with NSTEMIs due to the threat of bleeding |
|
|
Heparin
Factor Xa inhibitors Direct thrombin inhibitors Warfarin These are classes of? |
Anticoagulants
|
|
|
What are the "-parins"?
Enoxaparin** Dalteparin Tinzaparin |
Low Molecular Weight Heparin
(LMWH) |
|
|
Name the two types of Heparin agents
|
Unfractionated Heparin
LMW Heparin |
|
|
MOA for Unfractionated Heparin?
|
Accelerates the reaction between:
-Antithrombin and thrombin -Antithrombin and Factor Xa** |
|
|
Unfractionated Heparin or LMWH?
-Subcutaneous (usually) or IV -Predictable anticoagulant effect -No monitoring of the aPTT -Can be used at home -Expensive |
LMWH
|
|
|
Unfractionated Heparin or LMWH?
-IV (usually) or subcutaneous -Unpredictable anticoagulant effect -Monitor the aPTT |
UFH
|
|
|
MOA LMW Heparin?
|
Accelerates the reaction between:
-Antithrombin and Factor Xa |
|
|
What accelerates the reaction between AT and factor IIa (thrombin) or factor Xa by at least 1000 fold?
|
Heparin
|
|
|
What forms a ternary complex?
|
UFH
note: need at leas 18 saccharide units |
|
|
What is the Anticoagulant of choice during pregnancy?
|
Subcutaneous unfractionated heparin
or LMWH |
|
|
This needs to be monitored via aPTT
|
UFH
|
|
|
What drug Prevents thrombosis
**Prophylaxis and treatment** |
Heparin
|
|
|
You suspect a patient is having Thromboembolism during pregnancy. What would you use to treat?
|
Heparin (safe for preggers)
|
|
|
What could you use for immediate anticoagulation during a STEMI?
|
Heparin
|
|
|
What would you use for these?
-Pulmonary embolism -Deep vein thrombosis -Thromboembolism during pregnancy*** -Postoperative venous thrombosis -Arterial embolism (eg. from atrial fibrillation) -ST-elevation myocardial infarction (STEMI) -Unstable angina (UA) and Non ST-elevation myocardial infarction (NSTEMI)*** -Percutaneous coronary interventions (PCI) |
Heparin
|
|
|
Type I – rapid, mild, transient
Type II – delayed, sustained, severe These describe? |
Heparin Induced Thrombocytopenia
(HIT) |
|
|
UFH and to a lesser extent, LMWH
binds to plasma proteins including platelet factor 4 (PF4) Where does PF4 come from? |
Platelets
|
|
|
Summary of Type II HIT
look this over.... |
-Platelet factor 4 is released from activated platelets and binds to heparin
-Antibodies are produced to the heparin-PF4 complex -These antibodies bind to the heparin-PF4 complex -This immune complex (heparin-PF4-IgG) binds to platelet Fc receptors resulting in platelet activation |
|
|
What will happen to the platelet count
with HIT type 2? |
platelets DECREASE
|
|
|
What is the predominant clinical
presentation with HIT type 2? |
Thrombosis
|
|
|
Treatment for HIT?
|
**Heparin must be stopped**
-Thrombosis can be treated with other agents-->Direct thrombin inhibitors |
|
|
-Platelet count can decrease by 50%
- Thromboembolic complications (limb loss 20-30%) These are complications of? |
HIT
|
|
|
What causes HIT more often? UHF or LMWH?
|
UHF--> 1-5%
LMWH --> ~1% |
|
|
Should you give enoxaparin (LMWH) to
a patient who has HIT? |
NO
Even though it doesn't cause HIT as often LMWH should be avoided! |
|
|
Osteoporosis can occur with patients taking heparin for _____ months
|
3-6
|
|
|
**Osteoporosis**
UHF causes _______ and decreased _______ |
bone reabsorption AND ↓ bone formation
|
|
|
**Osteoporosis**
LMWH only causes _____________ |
↓ bone formation
|
|
|
-Active Bleeding
-Thrombocytopenia -Coagulation disorders -Increased risk of hemorrhage -Avoid after surgery of brain, spinal cord, or eye***** Contraindications for? |
Heparin
|
|
|
A patient on Heparin is having life threatening bleeding? What is the Heparin antidote?
|
Protamine Sulfate
|
|
|
What are some precautions when using Protamine sulfate (Heparin antidote)?
|
Can have anticoagulant effects
**Anaphylactic reactions** - diabetics who take protamine containing insulin |
|
|
Synthetic pentasaccharide sequence of heparin that is a selective factor Xa
inhibitor |
Fondaparinux
|
|
|
Longer half life than LMWH
-17-21 hours -Does not require monitoring Clincal Use: Prophylaxis of DVT in patients undergoinghip fracture surgery, hip or knee replacement surgery or abdominal surgery who are at risk for thromboembolic complications Used for Acute DVT and Acute PE (Combined with Warfarin) |
Fondaparinux
|
|
|
Hirudin - anticoagulant
Where does this come from? |
Salivary glands of leeches
|
|
|
What are the 2 Thrombin Inhibitors (IV)?
|
Lepirudin
-Recombinant derivative of hirudin Bivalirudin -Bivalent analog of hirudin |
|
|
What is the ORAL Thrombin inhibitor that is an alternative to Warfarin?
|
Dabigatran
|
|
|
"-rudin"
|
Thrombin Inhibitors (IV)
|
|
|
What is Dabigatran? What drug is it an alternative to?
|
Oral Thrombin inhibitor
ALTERNATIVE TO WARFARIN |
|
|
-Directly bind to and inhibit thrombin
-Effects are independent of anti-thrombin -Inhibits soluble (i.e. free) and fibrin-bound (i.e. in a clot) thrombin This is the MOA of?? |
Thrombin Inhibitors
|
|
|
Clinical Use of Thrombin Inhibitors:
Heparin induced Thrombocytopenia |
Lepirudin
**Argatroban** |
|
|
Clinical Use of Thrombin Inhibitors:
Heparin-induced thrombocytopenia undergoing percutaneous coronary intervention (PCI) |
Bivalirudin
|
|
|
Which Thrombin Inhibitor can cause allergic rxns including anaphylaxis?
|
Lepirudin
|
|
|
Which Thrombin Inhibitor can cause Dyspepsia and gastritis?
|
Dabigatran (ORAL)
|
|
|
What is an oral anticoagulant?
|
Warfarin (Coumadin)
|
|
|
MOA of Warfarin (Coumadin)?
|
Vitamin K antagonist
Inhibits the synthesis of Vitamin K dependent clotting factors in the liver -Factors II, VII, IX and X -Inhibits the synthesis of protein C and protein S |
|
|
______ inhibits vitamin KO reductase,
thereby blocking the formation of vitamin vitamin KH2. **This prevents the carboxylation (and hence production) of vitamin K dependent coagulation factors** |
Warfarin
|
|
|
What happens if vitamin K
stays in the oxidized form? |
prevents the carboxylation (and hence production) of vitamin K dependent coagulation factors (X, IX, VII, II)
|
|
|
Why does it take so long to get a peak
anticoagulant effect of warfarin? A. Warfarin has a long half life B. Poor bioavailability of warfarin C. Long half life of preexisting clotting factors D. Rapid loss of protein C and protein S |
C. Long half life of preexisting clotting factors
|
|
|
The following describe the pharmokinetics of ______:
97% bound to plasma proteins -Mainly albumin Metabolized in liver Narrow therapeutic index Dosages vary greatly |
Warfarin
|
|
|
T/F
If you eat foods high in Vit. K the effectiveness of Warfarin decreases |
TRUE
|
|
|
Prevent thrombosis
-Takes 3-5 days to be effective -Start in conjunction with Heparin |
Warfarin
|
|
|
This drug is monitored with PT
|
Warfarin
Standardized PT time = International Normalized Ratio (INR) |
|
|
This drug can be used to prevent Thromboembolism in patients with:
-Chronic atrial fibrillation -***Prosthetic heart valve*** -People at risk following surgery, trauma or cancer |
Warfarin
|
|
|
How would you use heparin and
warfarin to anticoagulate a person who develops a DVT? |
Start both warfarin and heparin at the SAME time
warfarin= DELAYED heparin= IMMEDIATE **Stop Heparin once INR is in normal range** |
|
|
A patient is scheduled for an
angioplasty. What anticoagulant may be administered just prior to the procedure? |
UFH
Enoxaprin Bivalirudin |
|
|
**Skin necrosis--from widespread
thrombosis** -Occurs early in therapy (within the first 10 days) -**Possibly due to reduced activity of Protein C** This is an adverse effect of? |
Warfarin
|
|
|
What is Protein C?
|
Endogenous anticoagulant
With a half life of only 8 hours (Less than most of the other vitamin K dependent clotting factors) |
|
|
**Purple toe syndrome**
-Usually occurs within 3-10 weeks -Release of **cholesterol microemboli** from atheromatous plaques Adverse effect of? |
Warfarin
|
|
|
A syndrome characterized by nasal
hypoplasia and stippled epiphyseal calcifications that resemble chondrodysplasia punctata. (Bone Problems) Assosciated with? |
1st Trimester Use of Warfarin
|
|
|
Is warfarin teratogenic?
|
YES
**Especially in 1st Trimester** (not as common in 2nd and 3rd trimesters) |
|
|
When would you consider using warfarin in a pregnant patient?
|
When she has a mechanical heart valve
|
|
|
This drug:
-When used alone, it can cause venous limb gangrene or multicentric skin necrosis -The rapid loss of the endogenous anticoagulant, protein C, can cause a **hypercoagulated state** |
Warfarin
**Heparin Induced Thrombocytopenia** |
|
|
A 47-year-old male with a history of atrial fibrillation that is being treated with metoprolol and warfarin presents to the emergency department with a nose bleed. His INR is measured at 9.3 (target 2.0-3.0). How can youstop the bleeding (i.e. stop/counteract the effects of warfarin)?
|
GIVE VITAMIN K
Then, clotting factors, frozen plasma, prothromin concentrate |
|
|
A 67-year-old female with hypertension, heart failure, and chronic kidney disease (CKD stage 3) was admitted with chest pain and shortness of breath. Her ECG was normal, however, there is suspicion of a UTI. She was started on unfractionated heparin (UFH) infusion for suspicion of a pulmonary embolism. She also was noted to have exacerbation of her heart failure (ejection fraction 25%). She began treatment for the UTI with ceftriaxone. On hospital day 7, her platelet count declined from 289 x 109/L on admission to 75 x 109/L. The aPTT prior to starting heparin was 28 seconds (normal 20-35 sec) and is now 57 sec (therapeutic range 48-71 sec). What drug change would you most likely make?
|
PATIENT HAS HIT
Stop UFH, Start Lepirudin |
|
|
Know this...
|
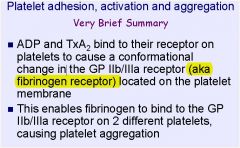
It's for anti-platelet stuff
|
|
|
Name a Cyclooxygenase Inhibitor
|
Aspirin
|
|
|
MOA of Cyclooxygenase Inhibitors (Aspirin)?
|
Irreversibly inhibits cyclooxygenase
-Greater inhibition of COX-1 than COX-2 Blocks the production of TxA2 -Platelets |
|
|
Do you want to inhibit the production of
PGI2 or TxA2 when using Aspirin? |
TxA2 !!!
Inhibiting PGI2 would cause Vasocontriction and platelet aggregation |
|
|
PGI2
-Platelet Aggregation and causes Vasoconstiction or -Inhibits platelet aggregation and causes Vasodilation |
-Inhibits platelet aggregation and causes Vasodilation
|
|
|
Why is cyclooxygenase inhibited for
only a short time in endothelial cells and forever in the platelet? |
Platelets lack nuclei and can't make more proteins...
Endothelial cells HAVE NUCLEI... |
|
|
Other than Aspirin, What is the MOA of other NSAIDs, like ibuprofen?
|
Reversibly Inhibit COX-1 and COX-2
|
|
|
Can we use COX-2 inhibitors for anti-platelet therapy?
|
NO
Potentially Cardiotoxic Apsirin negates any GI benefit from using a COX-2 (COX-2's are easier on the stomach) |
|
|
Adverse Effect:
**GI irritation and Bleeding** |
Aspirin
-Inhibits the synthesis of prostaglandins that promote secretion of bicarbonate and mucous |
|
|
Name the ADP Receptor Antagonists (2)
|
Clopidogrel
Prasugrel |
|
|
"-grel"
|
Clopidogrel
Prasugrel **ADP Receptor Antagonists** |
|
|
GP IIb/IIIa Receptor Antagonist?
|
Abciximab
|
|
|
It's 2 AM... here... have fun
|

|
|
|
Which of the following agents may be used for the secondary prevention of an acute MI? (select all that apply)
A. Abciximab B. Aspirin C. Clopidogrel D. Dalteparin |
Clopedigrel
|
|
|
Which of the following agents may be used to prevent thrombosis during PCI? (select all that apply)
A. Abciximab B. Aspirin C. Clopidogrel D. Dalteparin E. Warfarin |
A. Abciximab
B. Aspirin C. Clopidogrel D. Dalteparin |
|
|
Which Thrombolytic is isolated from Streptococci?
|
Streptokinase
|
|
|
What is t-PA?
|
Tissue Type Plasminogen Activator
breaks up clots... |
|
|
What are the recombinant t-PA thrombolytics?
|
Alteplase
Reteplase Tenecteplase |
|
|
"-plase"
|
Recombinant t-PA Thrombolytics
|
|
|
MOA of thrombolytics?
|
Catalyze the formation of plasmin fromplasminogen
- Plasmin degrades fibrin -Helps promote dissolution of a clot |
|
|
These agents are Not for unstable angina or NSTEMI
**Increased risk of death, MI and bleeding** |
Thrombolytics
|
|
|
If a patient has an extensive, proximal DVT
or Pulmonary Embolism (hemodynamically unstable) What would you use? |
Thrombolytic
these break up clots |
|
|
This thrombolytic can cause and allergic anaphylaxis and hypotension
|
Streptokinase
|

