![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
37 Cards in this Set
- Front
- Back
|
What are the three components of the cardiovascular system?
|
heart, blood vessels and blood
|
|
|
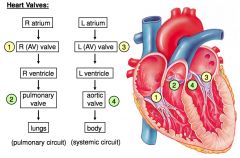
What are the two circuits of the cardiovascular system?
|
pulmonary circuit and systemic circuit
|
|
|
What is the pulmonary circuit?
|
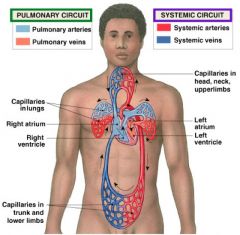
carries blood to/from gas exchange surfaces of lungs
|
|
|
What is the systemic circuit?
|
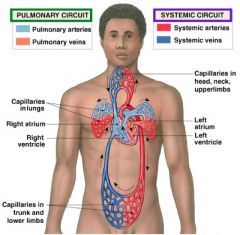
carries blood to/from the body
|
|
|
Blood alternates between _____ and _____
|
pulmonary circuit; systemic circuit
|
|
|
arteries
|
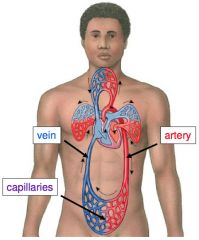
carry blood away from heart
|
|
|
veins
|
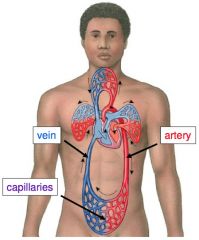
carry blood to heart
|
|
|
capillaries
|
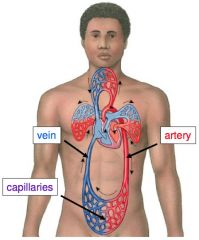
networks between arteries and veins
"exchange vessels" exchange materials (e.g. dissolved gases, nutrients, wastes) between blood and tissues |
|
|
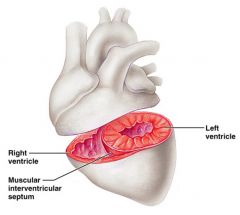
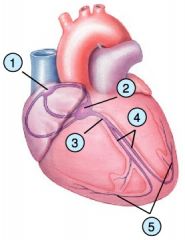
What are the four chambers of the heart?
|
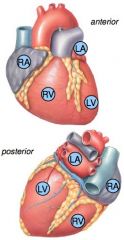
left and right atrium, left and right ventricle
|
|
Blood travels from:
|
1. superior vena cava
2. inferior vena cava 3. coronary sinus to the right atrium |
|
Blood travels from the right atrium to the right ventricle:
|
1. pulmonary trunk
2. left pulmonary arteries 3. right pulmonary arteries |
|
Blood travels from the right and left pulmonary veins to:
|
the left atrium
|
|
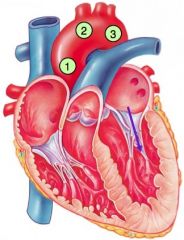
Blood travels from the left atrium to the left ventricle:
|
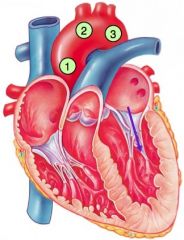
1. ascending aorta
2. aortic arch 3. descending aorta |
|
|
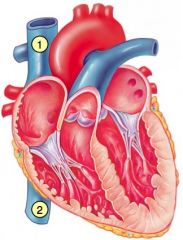
heart valves
|
ensure unidirectional blood flow through the heart
|
|
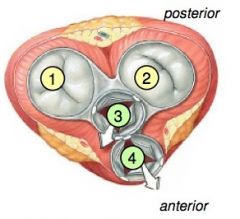
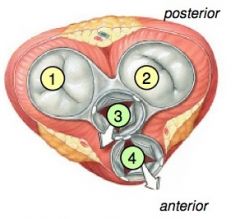
AV (atrioventricular valves)
|
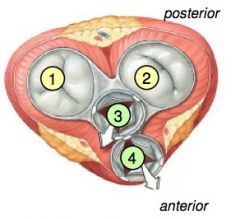
-prevent backflow into atria when ventricles contract
-chordae tendineae anchor AV valves to papillary muscles (prevent prolapse) 1. R AV valve (tricuspid valve) 2. L AV valve (bicuspid valve, mitral valve) |
|
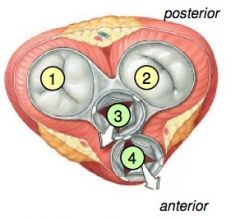
Semilunar valves
|
-prevent backflow of blood into the ventricle
3. Aortic valve - lies between L ventricle & the aorta 4. Pulmonary valve - lies between R ventricle & pulmonary trunk |
|
|
aortic valve
|
lies between L ventricle & the aorta
|
|
|
pulmonary valve
|
lies between R ventricle & pulmonary trunk
|
|
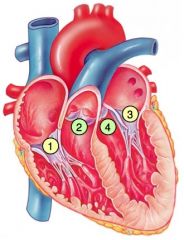
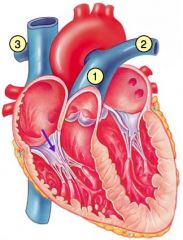
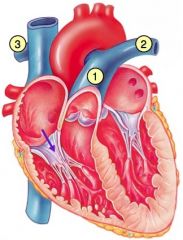
Heart valves
|
|
|
|
cordae tendineae
|
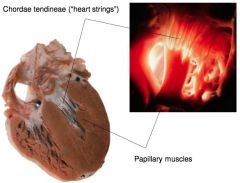
"heart strings"
|
|
|
Atrioventricular Valve Function
|
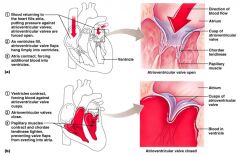
1) Blood returning to the heart fills atria, putting pressure against atrioventricular valves; atrioventricular valves are forced open
2) As ventricles fill, atrioventricular valve flaps hang limply into ventricles 3) Atria contract, forcing additional blood into ventricles 1) Ventricles contract, forcing blood against atrioventricular valve cusps. 2) Atrioventricular valves close. 3) Papillary muscles contract and chordae tendineae tighten, preventing valve flaps from everting into atria |
|
|
Semilunar Valve Function
|
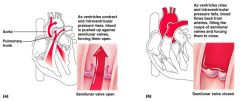
a) as ventricles contract and intraventricular pressure rises, blood is pushed up against semilunar valves, forcing them open.
b) As ventricles relax and intraventricular pressure falls, blood flows back from arteries, filing the cusps of semilunar valves and forcing them to close. |
|
|
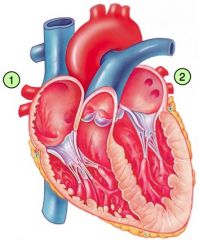
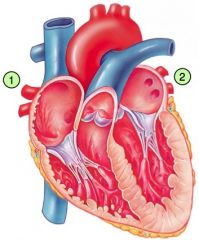
Why is the left ventricle larger than the right ventricle?
|
|
|
|
The bulk of the myocardium consists of cardiac muscle cells. What are two types?
|
contractile cells and autorhythmic cells
|
|
|
cardiac contractile cells
|
provide the pressure that pumps blood through the body
|
|
|
desmosomes
|
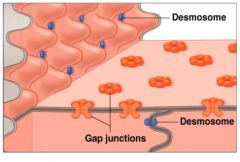
mechanical connection allows forceful contractions
|
|
|
gap junctions
|
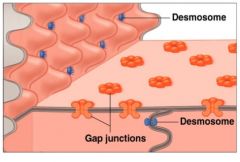
electrical connection allows heart to act as one unit
|
|
|
Two types of autorhythmic cells
|
intrinsic and extrinsic
|
|
|
intrinsic
|
control heart rate
|
|
|
extrinsic
|
effects on heart rate are through nerves & hormones
|
|
|
What are the five main types of autorhythmic cells?
|
1. sinoatrial node
2. atrioventricular node 3. atrioventricular bundle 4. R/L bundle branches 5. Purkinje fibers |
|
|
Authrhythmic cells: intrinsic conduction system
|
1) Initiate and 2) Distribute electrical impulses that stimulate contraction
|
|
|
automaticity
|
autorhythmic cells contracts automatically
|
|
|
pacemaker potential
|
("drift") unstable resting membrane potential authrhymic cells automatically and gradually depolarize toward threshold
|
|
|
SA node depolarizes first, establishing heart rate
|
-SA node generates 80-100 action potentials per minute (intrinsic rate)
Parasympathetic stimulation slows heart rate -AV node generates 40-60 action potentials per minute (intrinsic rate) |
|
|
Sequence of Excitation/Depolarization (1 of 2)
|
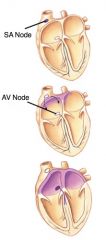
Pacemaker cells of SA node depolarize
↓ Electrical activity travels rapidly to AV node via internodal pathways ↓ Depolarization spreads across atria AV node delays impulse ~ 0.1 second **allows atria to contract before ventricles do |
|
|
Sequence of Excitation/Depolarization (2 of 2)
|
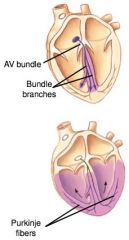
Depolarization wave travels down AV bundle and L/R bundle branches
↓ Depolarization wave travels thru ventricles via Purkinje fibers Ventricular contractile cells depolarize & contract |

