![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
92 Cards in this Set
- Front
- Back
|
Neuro exam assesses what 9 divisions of neuroaxis?
|
higher cortical functioning
cranial nerves cerebellum motor system sensory system deep tendon reflexes pathologic reflexes |
|
|
Broca's aphasia?
|
Left frontal lobe. Inferior Frontal gyrus
Maintain comprehension No fluency |
|
|
Gertsmann's syndrome?
|
Left parietal lobe lesion
Left/right indiscrimination finger agnosia acalculia agraphia without alexia anosognosia |
|
|
What cortical function is found in the right temporal region?
|
hearing sounds, rhythm, music
|
|
|
Wernicke's aphasia?
|
Left parietal temporal defect
Superior temporal lobe |
|
|
What are functions of the temporal lobes (Bilaterally) ?
|
learning and memory
olfaction: limbic auditory cortex: heschel's gyrus |
|
|
The perception of seeing objects bigger or smaller than they are is what?
|
Micropsia and macropsia
Right occipital lobe defect |
|
|
propasagnosia
visual hallucinations cortical blindness Anton's syndrome (lack of awareness of being blind) |
bilateral occipital lobe defect
|
|
|
What are the 5 muscles of CN III
Oculumotor |
m: levator palpebrae look for ptosis
m: superior rectus look up and out m: medial rectus adduction m: inferior rectus look down and out m: inferior oblique look up and in |
|
|
What is Adie's tonic pupil?
|
On exam, the eye is dilated and doesn’t constrict to light (we’re blocking the parasympathetic pathway from the Edinger-Westphal nucleus). The pupil will constrict with near vision- but very slowly. That’s why we call it a “tonic pupil,” it’s tonically slow.
|
|
|
What is Argyl Robertson's?
|
bilateral small pupils that constrict when the patient focuses on a near object (they “accommodate”), but do not constrict when exposed to bright light (they do not “react” to light).
|
|
|
The eyes are “down and out” with a droopy eyelid
|
CN III lesion
|
|
|
Patient tilts their head away from the lesion
|
CN 4 lesion
Think trauma or cogenital head-tilt decompensated with age |
|
|
The patient looks “cross-eyed.”
|
CN6
Consider intracranial pressure |
|
|
Pie in the sky
|
lesion in the temporal
(lower problem, has upper deficiency) |
|
|
Trochelar nerve: muscle and action?
|
Superior Oblique
Looks down and In |
|
|
Corneal reflex test
|
5 in
7 out |
|
|
Gag reflex test
|
CN9
CN10 |
|
|
An arm/leg that moves easier, or with less resistance, is the hypotonic limb
What problem in the brain is this? |
Ipsalateral Cereberallar Hemispheric Lesion (as opposed to vermis lesion)
|
|
|
"HANDS- tremor"
|
Nmemonic for cerebellar function examination
H: hypotonia A: ataxia or asynergy N: nystagmus D: dysmetria and dysdiadochokinesis S: stance or gait Tremor |
|
|
What is ataxia?
|
Inability to coordinate voluntary muscular activity
(Cerebellar problem) |
|
|
what are the types of nystagmus(s) seen in Cerebellar problems?
|
Optokinetic
gaze-evoked downbeat smooth pursuit |
|
|
Dysmetria
|
refers to the in ability to precisely coordinate the force and timing of muscular contraction when moving a limb. When the limb falls short of its target, it is called hypometria. When the limb extends beyond its target, it is called hypermetria.
|
|
|
Dysdiadochokinesis
|
refers to the impaired ability to rapidly perform alternating movements, such as rapid alternating hand movements.
|
|
|
What is excessive rebound (Stewart Holmes sign)?
|
inability of muscles to correct changes in resistance
Cerebellar function problem |
|
|
What kind of gait seen in a cerebellar lesion?
|
Wide based, unsteady , tendency to fall toward the unilateral hemispheric lesion (Same side)
"Ataxic" Heel to toe is also difficult* |
|
|
When is the pull test performed?
|
Parkinson's patients
|
|
|
A positional tremor is usually due to which disorder?
|
Metabolic disorders
(test with arms outstreched in the air) |
|
|
Pill rolling tremor is a defect in what structure(s)?
|
Basal ganglia
|
|
|
Romberg sign is a test for what?
|
Sensory system
(eyes closed) - relies on semicircular canals (eyes open) - eyes open and SC canals Checking for lesion in dorsal columns (proprioception) or a peripheral neuropathy |
|
|
A dermatome loss of sensation implicates what _____?
|
Radiculopathy - herniated intervertebral disk one which has become displaced from its normal position
|
|
|
Loss of sensation to the leg (But spares face and arms) implicates what type of lesion?
|
Vascular territory of the homunculus
Anterior cerebral artery (If it were complete side, we think subcortical where all the fibers coalesce |
|
|
Abnormal sensation only to the face indicates what?
|
Problem with the trigeminal nerve
|
|
|
A deep tendon reflex is a monosynaptic reflex that contains:
|
a. a sensory peripheral nerve that carries the impulse toward the spinal cord,
b. an afferent limb that allows the impulse to enter the spinal cord through the dorsal roots, c. an efferent limb that allows the impulse to exit the spinal cord through the ventral roots, d. and a peripheral nerve that carries the impulse to a muscle for contraction. |
|
|
What is a 4/4 reflex?
|
4/4: the reflex is elicited exceptionally easy, produces spread, and also produces clonus.
|
|
|
A lesion of the corticospinal tract shows what abnormal reflex?
|
Babinski Sign (primitive reflex that dissipates when brain myelinates)
|
|
|
What test do we perform to test for meningeal irritation?
|
Kernig sign
to evaluate patients with suspected meningeal irritation (i.e. meningitis). One places a patient supine on a bed, passively flexing the hip. The subsequent extension of a knee should normally not produce neck/back pain. If meningeal irritation is present, then passive extension of the knee produces the abnormal response of resistance of knee flexion. Click here to jump to the chapter on Kernig's sign. |
|
|
What is a 4/4 reflex?
|
4/4: the reflex is elicited exceptionally easy, produces spread, and also produces clonus.
|
|
|
A lesion of the corticospinal tract shows what abnormal reflex?
|
Babinski Sign (primitive reflex that dissipates when brain myelinates)
|
|
|
What test do we perform to test for meningeal irritation?
|
Kernig sign and Brudzinski sign
|
|
|
Fatiguable weakness implies a lesion at the _____
|
neuromuscular junction
|
|
|
Contrast muscular dystrophy versus infammatory myopathy
|
Dystrophy= defect in the internal structure
Typically Dystrophin gene Inflammatory = immune-mediate attack |
|
|
What are findings in duchenne muscular dystrophy?
|
Extremely high creatine kinase (up to 150,000)
Doughy gastrocnemius - pseudo hypertrophy Lordosis: weaknes of hip extensors Trendellenburg sign: pevlic girl weakness: pelvic girldle tilt each time a leg is raised to take a step Gower's sign: proxima lmuscle weakness. Rising from floor, goes to knees and elbows, extends knees and arms, "marches up himself" with hands and legs |
|
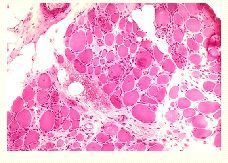
What is happening?
|
classic dystrophic changes with marked variation in fiber size and endomysial fibrosis. A few fibers are undergoing phagocytosis.
|
|
|
How does Becker differ from Duchenne?
|
Occurs later in life (Duchenne is by age 13), less severe
CK levels don't reach as high (10,000 range) **Look at histology to distinguish |
|
|
What two sign's are present in Duchenne and Becker's?
|
Gower's and Trendellenburg's sign
Indicate pelvic girdle weakness *Proximal weakness in both!! |
|
|
Which dystrophy produces a pattern of weaknes in face, scapulae, arm?
|
Fascioscapulohumeral Muscular Dystrophy
CK's can be normal, or elevate minimally up to 5x normal *Foot drop, pectoralis atrophy, scapular winging |
|
|
This dystrophy is caused by a genetic trinucleotide repeat.
hatchet like face, with baldness, cataracts, cardiac conduction defects and presence of myotonia |
Myotonic dystrophy
|
|
|
What are the 2 inflammatory myopathies? Presentation?
|
*Polymyositis
Associated w/interstitial lung disease Perform muscle biopsy *Dermatomyositis (involves rash preceding weakness) Associated with Ovarian Cancer Tx: Prednisone |
|
|
"Fatiguable weaknesses" - we suspect what disorder?
|
Neuromuscular junction disorder
Ptosis Dysconjugate gaze Dysphagia Dysphonia - inpairment in ability to produce voice sounds Proximal muscle arm and leg weakness |
|
|
what 3 diagnoses can be made when you localize a lesion to the neuromuscular junction?
|
Myasthenia Gravis
Lambert Eaton Myasthenic syndrome Botulism |
|
|
Main difference between Myasthenia Gravis and Lambert Eaton Myasthenic gravis
|
Myasthenia: Immune mediated Destruction of post-synaptic
associated with thymoma LEMS: immune-mediated destruction of pre-synaptic associated with small cell lung cancer |
|

What is this chart interpreting?
|
EMG test of muscles
Top is normal Middle is Myasthenia (repetitive simulation shows decrement) Bottom is LEMS (increment in the complex motor action potential) |
|
|
What is peripheral neuropathy?
|
refers to damage to the longest nerves that convey either sensation, strength, autonomic function, or any combination thereof
|
|
|
Sensory neuropathies usually start where and migrate to?
|
Start distally and progress proximally.
Can manifest numbness, tingling or dampened sensation |
|
|
Which symptoms tend to follow sensory symptoms?
|
Motor symptoms
i.e. weakness in great toe, inability to dorsiflex, producing footdrop...catching toes on uneven surfaces |
|
|
What other autonomic symptoms may occur alongside peripheral neuropathy?
|
dys-accommodation of the lens of the eyes
cardiac arrhythmias dys-hydrosis, anhydrosis, or hyper-hydrosis gastroparesis constipation erectile dysfunction, or loss of nocturnal penile tumescence edema or erythema of digits |
|
|
Most peripheral neuropathy are idiopathic...
The others can be explained by what problems? |
diabetes or impaired glucose tolerance
hypovitaminosis B12 vasculitis syphilis monoclonal gammopathy thyroid dysfunction |
|
|
When interrogating for possible causes of clinical neuropathy: what tests can you perform?
|
2-hour oral glucose tolerance test
vitamin B12 W-ESR RPR serum protein electrophoresis with immunofixation free T4 and TSH |
|
|
Most common dermatomes to know?
|
C5: shoulder
C6 thumb and index finger C7 middle finger C8 ring and pinkey finger T4 nipple line T10 umbilicus L2 inguinal canal |
|
|
What are the common myotomes to know (lower body)
|
L2- Leg adduction
L3- Hip flexion L4- Knee extension L5-Ankle dorsiflexion S1-Plantar flexion |
|
|
Testing deep tendon reflexes
Which 5? |
C5 biceps brachii
C5/6 brachioradialis C7 triceps L4 patellar S1 Achilles |
|
|
what types of lesions produce lower motor neuron findings? (4)
Presentations? (5) |
muscle, Neuromuscular junction,
Peripheral nerve, spinal nerve root/radical atrophy of muscle weakness of muscle fasiculations hypo or areflexia hypotonia |
|
|
Upper motor neuron lesion findings
|
Hypertonia
hyper-reflexia Clonus Babinski sign Spasticity (Rate dependent) *Clasped knife lesions in spinal cord, brainstem, subcortex, cortex can cause UMN if corticospinal tract is lesioned Findings are below the lesion |
|
|
Causes of Spinal Cord Lesion
5 acute ; 2 subacute ; 3 chronic |
Acute onset of signs and symptoms:
spinal cord infarct acutely herniated disc compression fracture producing impingement on the cord epidural abscess epidural hematoma Subacute onset of signs and symptoms multiple sclerosis plaques syrinx (expanding cyst) Chronic onset of signs and symptoms spinal cord tumor vitamin B12 deficiency (cobalamin) syphilis |
|
|
Which cranial nerves associated with parts of braintstem
|
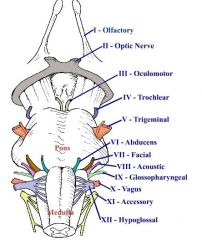
12, 11, 10, 9 exit from the medulla
8, 7, 6, 5 exit from the pons 4, 3 exit from the midbrain 2, 1 exit from this level |
|
|
Brainstem lesions lead to what findings? (Answers for each CN lesion)
|
1 decreased smell
2 decreased vision 3 double vision 4 double vision 5 decreased sensation 6 double vision 7 decreased strength of facial expression 8 deaf and dizziness 9 dysphagia and dysphonia 10 dysphagia and dysphonia 11 decreased head turning and shoulder shrug 12 dysarthria |
|
|
How do you determine if a patient with Bell's palsy has a central problem (i.e. stroke) or a peripheral CN 7 lesion?
|
Lower CN7 lesions also produce:
1. metal dysgeusia, as CN7 carries taste from the tongue (water tastes metallic) 2. ipsilateral hyperacusis, as CN7 innervates the stapedius, which normally dampens loud sounds 3. forehead weakness |
|
|
Lesions in the brainstem are usually caused by what?
|
Hemorrhagic or ischemic stroke
Also tumors MS is also possible (formation of plaques) |
|
|
What are signs and symptoms of spinal cord lesions?
|
bilateral lower extremity weakness
bilateral lower extremity sensory dysesthesias (possible upper extremity involvement if cervical spine involved), with a sensory level bowel and bladder retention or incontinence **See normal findings above the lesion **See UMN findings below the lesion |
|
|
Brainstem and cerebellum receive circulation from?
|
Vertebral Arteries and the basilar artery and its subsequent arteries
|
|
|
what are symptoms that would suspect posterior circulation defect?
|
loss of consciousness
syncope dizziness/vertigo dysphagia dysphonia dysarthria hemiparesis of face/arm/ leg equally invoved hemidysethesias of face/arm/leg equally involved |
|
|
Dysesthesia (Tingling) always implicates what type of lesion?
|
Subcortical lesion
|
|
|
Cortex signs and symptoms related to vascular causes:
What feeds arm/face and leg? |
Face and arm > leg = MCA (middle cerebral artery)
Leg > face and arm = ACA (anterior cerebral artery) |
|
|
What are 5 common causes of lesions showing cortical dysfunction?
4 common manifestations? |
subdural or epidural hematoma
subdural or epidural abscess meningioma subarachnoid hemorrhage seizures Manifestations: Apraxia, aphasia (Broca /wernicke), agnosia, neglect |
|
|
What is multiple sclerosis?
|
T-cell mediated disease that demyelinates only the CNS
**See plaques Upper motor neuron findings Spasticity Hyper-reflexia/clonus Babinski reflex Increased tone (hypertonia) |
|

What is seen here?
|
Multiple Sclerosis plaques
Present in 20's, 30's, 40's with waxing and waning motor symptoms **2 main eye findings: optic neuritis (may cause scotoma) and Internuclear Opthalmoplegia ( impairs adduction) Typically bilateral? |
|
|
What is optic neuritis?
What is affected? |
Inflammation of optic nerve. Typically product of immune-mediated demyelination.
Prevents nerve from entering the brain (Affects afferent pupillary reflex) |
|
|
What test do you perform when suspecting optic neuritis?
|
Swinging torch test
Should see constriction in both eyes if light shown in unaffected eye. In the affected eye, eyes would dilate. **Efferent pathway not effected in optic neuritis |
|
|
What causes Korsakoff's syndrome?
|
Lack of Vitamin B1, Thiamine
(Alcoholics) **Damage to medial thalamus anterograde amnesia retrograde amnesia, severe memory loss confabulation, that is, invented memories which are then taken as true due to gaps in memory sometimes associated with blackouts meager content in conversation lack of insight apathy - the patients lose interest in things quickly and generally appear indifferent to change. |
|
|
What two eye disorders do we associate with Multiple Sclerosis?
|
Optic Neuritis
and INO (MLF lesion) |
|
|
A right MLF lesion causes which inability?
|
Right eye is unable to look past midline (Adduct)
|
|
|
what are the 3 classifications of headaches?
|
Migraine - pulsatile and localize behind the eye. Commonly produce nausea and vomiting
Cluster - usually in men. Wake ppl up from sleep. Have histaminic symptoms: rhinorrhea, congestion, lacrima Tension - worsen at the end of the afternoon/evening, are described as nonpulsatile, and produce neck stiffness. They have no aura or lateralizing features, and do not typically produce nausea or emesis. |
|
|
what is decorticate posturing?
|
Implicates lesion above the red nucleus (midbrain) - removal of corticospinal pathways
produces flexed elbows with cluched fists in internal rotation, and leg extension with plantarflexion (tiptoe posturing). Think of it as the patient trying to touch the cortex of their brain. |
|
|
What is decerebrate posturing?
|
lesions below red nucleus but above vestibular nucleus
produces opisthotonos (head and trunk extended), teeth clenched, and an extended elbow with cluched fists in external rotation, and leg extension and internal rotation with plantarflexion |
|
|
What is seen in 3rd nerve lesion?
(3) |
An eye that deviates down and out
Ptosis Blown pupil |
|
|
What are third nerve lesion causes (2)which may spare pupils?
|
DIabetes
Myasthenia Gravis |
|
|
2 causes of third nerve lesions which also involve pupils
|
Aneurysm of posterior communicating artery
Tumor |
|
|
Symptoms of parkinson's disease
|
Bradykinesia (slowness of movement)
Postural instability Resting tremor Cogwheel rigidity |
|
|
Why can we not administer dopamine to parkinson patient's?
|
It can't cross the BBB!
So we give L-Dopa, a precursor of dopamine. |
|
|
what are dopamine agonist drugs for parkinson patient's?
|
Pramipexole (mirapex)
Ropinerole (Requip) |
|
|
What are the 3 categories (overall 6 kinds) of PNS autoimmune disorders?
|
PN:
Guillain Barre Syndrome (GBS) Chronic Inflammatory Demyelinating Polyradiculoneuropathy (CIDP) NMJ: Myasthenia Gravis (MG) Lambert Eaton Myasthenic Syndrome (LEMS) Muscle: Polymyositis Dermatomyositis |

