![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
115 Cards in this Set
- Front
- Back
|
2 energy sources for the Brain
|
Glucose and Ketone Bodies
(Ketone bodies made from Acetyl Coa in the liver when carbs are scarce so fatty acids are broken down) |
|
|
Pseudounipolar neurons are found as?
|
Sensory ganglia
|
|
|
Bipolar cells are found as?
|
Retina and olfactory epithelium
|
|
|
Which is the most common type of neuron in the CNS?
|
multiplar neuron
|
|
|
What is the septum pellucidum?
|
Thin membrane which separates the anterior horns of the left and right lateral ventricles.
Located midline and between the two cerebral hemispheres |
|
|
What is the interventricular foramina (of Monro)
|
channels that connect the paired lateral ventricles with the third ventricle at the midline of the brain
|
|
|
Where is CSF pressure the highest?
|
In the ventricles. Diminishes along the subarachnoid pathways.
|
|
|
CSF absorption occurs where?
|
Arachnoid villi. Penetrate the dura and protrude into superior sagittal sinus
|
|
|
Hypoventilation does what to do the body's C02 and pH?
Effect on intracranial pressure? |
Raises pC02 and decreases pH (more acidic). This vasodilates and increases intracranial pressure via increased cerebral bloodflow
|
|
|
Hyperventilation effect on body CO2, pH, intracranial pressure
|
reduces c02, increases pH. Vascular resistance increases and decreases CSF pressure.
-Option for management of acutely raised ICP |
|
|
What occurs when Intracranial Pressure raises to mean systemic pressure?
|
Causes widespread reduction in cerebral blood flow and perfusion. Global ischemia will lead to brain death.
|
|
|
What are some causes of increased ICP?
|
1) cerebral or extracerebral mass
2) Increase in venous pressure 3) obstruction to flow and absorption of CSF 4) Expansion of CSF volume (meningitis, subarachnoid hemorrhage) |
|
|
Clinical manifestations of ICP?
|
headache, N/V, drowsiness, ocular palsies, papilladema (optic disc swelling)
|
|
|
How often is CSF renewed?
|
~5 hours, 5x daily
|
|
|
Main sites of CSF formation
|
Choroid plexuses
|
|
|
Function of the blood brain barrier
|
Protect brain from substances
Biochemical barrier for selective transport Regulatory interface for metabolism |
|
|
Disorders which break down BBB
|
Stroke, seizures, infections, autoimmune disorders, multiple sclerosis, tumors
|
|
|
CSF composition
|
glucose 50-80 ng/dL
protein 40-45 mg/dL RBC’s *0 WBC’s *0-4 cells/µL opening pressure 12 – 20 mmH2O |
|
|
Vasodilation increases blood flow, how does this overall affect CNS BP?
|
Higher blood flow causes higher CNS BP, this increase intracranial pressure.
(Increased CO2 causes vasodilation, an effect of hypoventilation) |
|
|
Venous BP effects on CSF pressure?
|
increasing pressure produces immediate effect on ICP
|
|
|
3 ways to perform a spinal tap
|
Lumbar puncture
Cisternal puncture Ventricular tap |
|
|
Reasons to perform a spinal tap
|
-Diagnose infection
-Subarachnoid hemorrhage -CSF drainage and pressure reduction -Infusing medications |
|
|
Proper way to measure CSF pressure?
|
Patient lies in lateral decubitis position.
Draw line between iliac crests (insertion point) Penetrate through dura, arachnoid mater and draw from subarachnoid space *Epinephrine helps reduce bleeding |
|
|
Contraindications to a spinal tap
|
Raised intracranial pressure
Coagulopathy (low platelets, elevated prothrombin time) Area of infection overlying site |
|
|
Cerebral perfusion pressure. What happens when it is too low or too high?
|
Too low: brain tissue becomes ischemic
Too high: elevated ICP |
|
|
Noncommunicating (obstructive)hydrocephalus
|
Tumor/mass/abscess of infection which blocks flow of CSF
|
|
|
Blockage of arachnoid granulations is an example of what type of hydrocephalus?
|
Communicating hydrocephalus.
There is still communication of the ventricular tree. |
|
|
Hydrocephalus ex vacuo
|
Occurs due to reduction in brain atrophy (dementias, schizophrenia, post traumatic injuries).
It is not due to increased pressure, but a compensatory enlargement resulting from loss of parenchyma |
|
|
Clinical manifestations of abscess in the brain?
|
Fevers, headaches,
would not see a change in symptoms standing up or lying down |
|
|
Low pressure headaches which get better when standing up can be explained by what condition?
|
hydrocephalus (accumulation of CSF fluid)
|
|
|
Why is hydrocephalus a possible complication from meningitis?
|
Arachnoid granules become thickened. This is communicating hydrocephalus as there is no blockage of the ventricular system.
|
|
|
Patient has a small tumor in brain. Headaches which only present when sleeping lying down can be explained due to?
|
Hypoventilation which occurs naturally as we sleep.
Side note: Sleep apnea is a common cause of daily headaches |
|
|
Why do you not perform a spinal tap to relieve pressure on a person with cerebral edema?
|
The pressure will drop and the brain will push down on the foramen magnum.
(Should increase ventilator rate on patient to reduce blood flow to the brain. This decreases CO2 in blood) |
|
|
Cranial nerve lesions produce findings on which side of the body?
|
Ipsilateral (Same)
|
|
|
Tract which is a sensory pathway for pain and temperature?
Where does it decusate? |
Spinothalamic
Originates in the spinal cord. Decusates at the spinal level it enters and goes straight to the brain |
|
|
Tract which conveys vibration and proprioception? Decusates?
|
Dorsal column / medial lemniscus
(Decusates at the cervicomedullary junction - where cord becomes medulla) |
|
|
Tract that conveys motor impulses? Location of decusation?
|
Corticospinal (pyramidal tract)
Decusates at pyramids, where brainstem becomes cords |
|
|
Diplopia
|
Suspect CN 3,4,6
CN 2 is not part of brainstem and lesions to this causes loss in clarity/vision |
|
|
Droopy face. What CN affected? Brain location?
|
CN 7 - facial expression
In the Pons (CN 5,6,7,8 lies here) (CN 5 is possible but mainly is chewing muscles) |
|
|
Tongue weakness is a problem of what cranial nerve?
|
CN 12 - Hypoglossal
which emerges out of medulla |
|
|
Facial numbness is a problem of what CN?
|
CN 5 - in the pons
|
|
|
Alar plate becomes?
|
The dorsal horn or sensory cell columns in spinal cord development
|
|
|
Basal plate becomes?
|
Ventral horn or motor cell columns
(Sulcus limitans separates alar and basal) |
|
|
Define Dermatome
|
Region of skin innervated by axons of cells located in ONE dorsal root ganglion. Dermis associated with a developing somite.
|
|
|
Characteristics of a reflex
|
Prewired connection
Automatic, involuntary Predictable and uniform Can test a single cord segment or pair of cranial nerve |
|
|
Deep Tendon Reflexes (name some and their associated level)
|
Arm C5, 6 biceps
Forearm C5, 6 brachioradialis Elbow Extension C7 triceps Knee Jerk L4 quadriceps femoris Ankle Jerk S1 Gasrocnemius/ soleus |
|
|
What are muscle spindles?
|
Special sense organs innervated by Ia fibers, the largest and fastest axons
|
|
|
Synonyms for efferent limb (motor neuron)
|
Alpha motor neuron
motoneuron anterior horn cells ventral horn cell final common pathway lower motor neuron = LMN to muscle fiber |
|
|
What is a flexor reflex?
|
protective reflex, has an interneuron, occurs on ipsilateral side
|
|
|
Cross extensor reflex?
|
Ipsilateral withdrawal and contralateral extension
Involves commissural interneurons which cross midline. |
|
|
Preganglionic parasympathetic neurons in brain steam have axons traveling in CN's____ and preganglionic axons in ____spinal cord
|
CN 3,7,9,10
S2-S4 spinal cord |
|
|
SLUDD parasympathetic responses + 3 "decreases"
|
Salivation, lacrimation, urination, digestion and defecation
Decreased HR, diameter of airways and diameter of pupil |
|
|
Describe parasympathetic pathway for the cranium
|
1) cellbody located in brain stem (nucleus)
2) nucleus joins with axons entering/leaving that cranial nerve 3) synapse on postganglionic neuron such as otic, ciliary, submandibular, pterygopalantine |
|
|
CN involved in the baroreceptor reflex
|
CN 9
Medulla is the control center Parasympathetic can decrease/increase vagal activity Sympathetic can increase heart rate, cardiac filling, contractility and also constrict arterioles |
|
|
Thalamus function
|
Its function includes relaying sensation, spatial sense, and motor signals to the cerebral cortex, along with the regulation of consciousness, sleep, and alertness.
|
|
|
Hypothalamus function
|
autonomic and endocrine functions (hormones)
|
|
|
What is the corpus callosum?
|
Connects left and right hemispheres, facilitates interhemispheric communication. Largest white matter structure (containing 200-250 controlateral axon projections)
|
|
|
Lateral and medial geniculate
|
Structures of the thalamus
Lateral - Light (visual cortex) Medial - music (auditory cortex) |
|
|
What is the ventral posterior nucleus made up of? what part of brain? function?
|
VPL (body) +VPM (head)
Ventral posterolateral nucleus and ventral posteral medial Somatosensory (body and head) relay nucleus in the thalamus of brain |
|
|
What are upper motor neurons?
|
are cortical neurons that innervate lower motor neurons (either directly or via local interneurons). The axons of upper motor neurons are contained within the pyramidal system, which is composed of the corticospinal (pyramidal) and corticobulbar tracts.
|
|
|
What are lower motor neurons?
|
neurons that directly innervate skeletal muscle. The cell bodies of these neurons are located within the ventral horns of the spinal cord and within brainstem motor nuclei.
|
|
|
a lesion involving all of the corticospinal and corticobulbar fibers from the left cerebral cortex produces
|
1) Right hemiparesis (weakness of the right upper and lower limbs).
2) Weakness of the right face below the forehead. 3)Deviation of the tongue to the right upon protrusion (transient). |
|
|
Spinothalmic tract decusates where?
|
At the level it enters the spinal cord (pain/ temp)
|
|
|
Which lobe picks up sensory?
|
Parietal lobe
|
|
|
Lesion in the precentral region would cause what?
|
Affects motor since it is where the corticospinal tract originates
|
|
|
Which lobe controls motor function?
|
Parietal lobe (precentral region)
|
|
|
What circulation feeds the brainstem?
|
Posterior circulation (vertebral arteries (which merge to form the basilar artery at the pons))
|
|
|
CN 9 functions
|
somatic motor stylopharyngeus (elevate pharynx)
visceral motor parotid gland somatic sensory external ear special sensation taste to the tongue (posterior 1/3) visceral sensation baro- and chemoreceptor reflexes reflex gag (afferent limb only) |
|
|
What CN does sensation and taste to the posterior 1/3 of tongue?
|
CN 9
- Anterior 1/3: CN 7 is taste and CN 5 is touch |
|
|
What are features of a CN 9 neuropathy?
|
Hoase voice
Dysphagia (difficulty swallowing) Gag reflex absent (afferent limb) Abnormal taste |
|
|
Dysphagia
vs Dysphasia |
Difficulty swallowing (Brainstem problem)
- Dysphasia = abnormal language (cortex problem) |
|
|
Vagus nerve functions
|
somatic motor muscles of the larynx/pharynx
(speech and swallow) visceral motor thoracic and abdominal viscera somatic sensory external ear special sensation taste (posterior 1/3) visceral sensation pharynx, larynx, aortic arch/body thoracic and abdominal viscera special sensation tongue (posterior 1/3) |
|
|
What does a CN 10 neuropathy look like?
|
uvula deviated away from the lesion
hoarse voice (more so than CN 9) dysphagia tachycardia |
|
|
Describe the gag reflex
|
CN 9 is afferent limb
CN 10 is efferent limb Uvula deviates away from the cranial nerve lesion |
|
|
Person with a downsloping shoulder would be suspected of having?
|
CN 11 lesion (Weakness of trapezius muscle)
|
|
|
CN 11 innervates what muscles?
|
Trapezius and Sternocleidomastoid
|
|
|
CN 12 Hypoglossal innervates what muscles?
|
Intrinsic and Extrinsic muscles of tongue
|
|
|
What does hypoglossal neuropathy look like?
|
Dysarthria (motor speech problem -abnormal articulation)
Dysphagia tongue biting Tongue deviation "lick your wounds" |
|
|
Dysphagia
Dysphasia Dysarthria |
Difficulty swallowing
Abnormal language Abnormal Articulation (motor) |
|
|
What does a complete, right medullar lesion look like?
|
pain and temperature contra
vibration and proprio contra hemiparesis contra gag absent Tongue deviation Toward lesion voice hoarse swallowing dysphagia uvula deviation opposite les. |
|
|
Diplopia can be due to what involvement of structures?
|
CN III, IV, VI nuclei, nerves, NMJ’s or extraocular muscles
|
|
|
Difficulty swallowing (dysphagia) and hoarseness can be due to involvement of motor neurons whose cell bodies are located in a structure called the _______________ and whose axons contribute to cranial nerve(s) _______.
|
nucleus ambiguous
CN’s IX and X |
|
|
UMN and LMN
Describe: Tone, atrophy, fasciulations, reflex, Babinski sign, weakness |

|
|
|
How can a muscle atrophy if some sort of lesion is the problem?
|
Peripheral nerve lesion - connection to a muscle completely lost causing it to atrophy
|
|
|
What happens to a muscle in acute denervation?
|
Fasiculations occur, involuntary muscle twiches due to spontaneous discharge of an injured/severed axon - loss of resting tone and becomes hypotonic
|
|
|
Why is weakness seen with upper motor neuron lesions?
|
The signal from UMN to LMN is then interrupted and weakness will be seen. The LMN is still alive
|
|
|
A patient who complains of tremors or "Worms under their skin" would lead you to think what?
|
Lower motor neuron lesion
|
|
|
Difference in muscle loss with UMN and LMN
|
UMN- longer period of time till muscle GROUP loses tone
LMN- occurs acutely from denervation and is more focal |
|
|
A patient complains of jumpy legs or difficulty relaxing legs. What is the problem?
|
UMN lesion
|
|
|
Which is more severe: lesion in corona radiata, or in the internal capsule?
|
Corona radiata contains less fibers
|
|
|
What is a myotome?
|
THe muscles innervated by a single nerve root
Tears of roots give a pattern of weakness in a myotome |
|
|
Spasticity is seen in what type of lesion?
|
UMN lesion.
This leads to increased tone |
|
|
A CNS lesion does not always show UMN lesion findings. Why?
|
THe lesion must occur in the corticospinal tract in order to produce UMN findings
|
|
|
Legs which give out while standing is a common symptom of what lesion?
|
UMN
Also, patient's inability to relax legs or having shaky legs |
|
|
Motor strength grading is on what scale?
What grade describes ability to only move joint with gravity removed? |
5 scale
2/5 : can only move w/out gravity 3/5: Full ROM but against no resistance |
|
|
Describe the scores of reflex grading
|
4/4 sustained clonus
3/4 Spread to other segments 2/4 NORMAL 1/4 requires reinforcing maneuvers 0/4 absence with reinforcing maneuvers |
|
|
CT images are acquired in the ____plane and occasionally in ____plane
|
Axial plane
Sometimes in coronal |
|
|
Calcifications appear at what light intensity?
|
Bright
(grey and white matter appear grey) Nonhemorrhagic lesions are slightly dark |
|
|
What is the risk of using contrast medium in patients?
|
They are potentially nephrotoxic and of high concern is diabetics / renal failure
|
|
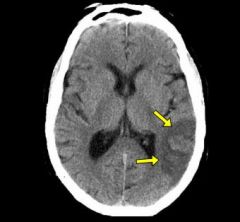
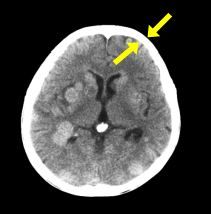
What type of scan is this? What is the arrow pointing to?
|
CT scan (all white calvarium)
Pointing to non hemorrhagic lesion |
|
|
In CT scans:
What appears bright? What appears slightly dark? |
Bright: calcifications, acute blood, contrast
SLightly dark: Most nonhemorrhagic lesions |
|
|
How does contrast help make diagnoses?
|
Contrast helps us visualize if blood is seeping into areas that usually don't have contrast-
Ex: variety of lesions, absces, subacute infarct, tumors Only regions that lack a BBB will normally show brightness |
|
|
MRI images are collected in what plane?
|
Cross-sectional
|
|
|
Advantages of MRI over CT
|
More cost -effective overall
Diagnostically answers questions better No ionizing radiation |
|
|
Disadvantages of MRI
|
SLower than CT (CT better for ER)
Must sedate younger children since scans are slow |
|
|
In T1 MRI: how does gray matter, csf, and white matter appear
|
Gray matter=gray
White matter= white CSF is dark |
|
|
In T2 MRI: what is appearance of gray matter, white matter, CSF
|
CSF is white**
Gray matter is relatively white White matter is relatively gray |
|
|
MRI FLAIR: how does gray, white matter appear? CSF?
|
CSF is black*
Gray matter is relatively white white matter is relatively gray |
|
|
What distinguishes CT from MRI?
|
An All white calvaria
|
|
|
What is the most sensitive MRI for nonhemorrhagic lesions?
(shows brightest) |
FLAIR
|
|
|
T2* GRE is most sensitive route for detecting what?
|
Hemorrhagic lesions
(Have black appearances) |
|
|
DWI and DTI are most sensitive routine sequences for what?
|
Acute infarctions
(areas of restriction diffusion of tissue water appear bright) |
|
|
Which neurotoxin affects presynaptic cholinergic transmission in the PNS
|
Botulism (most potent known toxin)
|
|
|
Which CN tests visual acuity AND visual fields
|
CN II
|
|
|
3 most common areas of aneurysms
|
Anterior communication artery (30%)
Middle Cerebral artery (20%) Posterior communicating (25%) |

