![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
63 Cards in this Set
- Front
- Back
|
address possible sensations during pregnancy |
heartburn, backache, leg cramps, various fears and |
|
|
Preconception care |
- geenral health - screening - genetic counselling |
|
|
General Helath advice |
optimal nutrition and |
|
|
Foods to avoid |
Listeria infection is a |
|
|
Folic acid |
Folic acid (0.5 mg tablets) is now generally |
|
|
Examination |
blood pressure, cardiac status, urinalysis |
|
|
Rubella serology |
Rubella serology should be estimated and, if required, |
|
|
VAricella |
Ask about a history of varicella and, if necessary, |
|
|
Vaccinationd to consider |
• Boostrix (diphtheria, tetanus, pertussis) |
|
|
summary: advice to patients |
• Stop smoking. |
|
|
The inital visit |
book them into an antenaal outpatient department - must make a estimated due date US helps |
|
|
History |
• Confi rm the pregnancy by the menstrual history and |
|
|
vaginal bleeding |
if Rh negative, send blood |
|
|
if maternal age >37 years |
consider fi rst trimester |
|
|
Examination |
• general fi tness, colour (?anaemia)
Speculum examination: perform a Pap smear and |
|
|
Antenatal screening |
Debate continues |
|
|
1st trimester combined screening test |
• Serology tests (9–13 weeks, 10 is ideal): |
|
|
Estimating due date |
from the first day of the last menstrual period subtract 3 from the month and add 7 to the days |
|
|
Visits during pregnancy |
average number is 12, being reviewed to 6 A common routine schedule
A systematic review of seven RCTs found no |
|
|
Things to record for each visit |
• weight gain |
|
|
Record day of fi rst fetal movements (i.e. ‘quickening’) |
• primigravida: 17–20 weeks (primigravida first birth-multi is 2nd or more) |
|
|
Fundal Height |
The uterus is a pelvic organ until the |
|
|
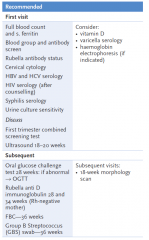
Routine Ix |
|
|
|
Causes of proteinuria in pregnancy |
Urinary tract infection |
|
|
Nutrition Advice |
1 Eat most: • lean meat, poultry or fish—1 or 2 serves (at least 2 serves of red meat per week) |
|
|
Weight gain in prgnancy |
12kg |
|
|
Drugs in pregnancy |
avoid all even ideally caffeine avoid passive smoking smoking cessation programs are effective in imporveing irth outcomes
but can have 1 cup of coffee or 2 teas |
|
|
Breastfeeding |
encourgared |
|
|
Activities durign pregnangcy |
Mothers should be reassured that pregnancy is a |
|
|
Sex in pregnancy |
Coitus should be encouraged during pregnancy but
Positions: posterior entry and the female in superior positions are suitable |
|
|
Travel |
avoid standing in trains avoid air travel after 28 weeks and its not permitted after 36 weeks |
|
|
Fetal movement chart |
If daily fetal movements exceed 10 and the regular |
|
|
Possible exposure to rubella |
When contact with a possible case of rubella occurs |
|
|
Vaginal bleeding in early pregnancy |
common 10% of all pregnancies BUT 15% do miscarry - gotta make sure its not an ectopic and or a threatened misccarriage |
|
|
Vaginal bleeding < 6 weeks |
• <6 weeks: Do serial quantitative HCG levels, which should double every 2 days (ultrasound usually unhelpful). If rise is too slow it means a non-viable pregnancy (?in tube or uterus). If HCG >1500 IU/L transvaginal ultrasound is used to show gestational sac. |
|
|
Vaginal bleeding 6-8 weeks |
Ultrasound will defi ne an intra-uterine |
|
|
Vaginal bleeding >8 weeks |
Normal ultrasound reassuring since miscarriage rate is only 3%. |
|
|
Vaginal bleeding 18-24 weeks |
A small bleed between 18–24 weeks indicates |
|
|
Morning sickness |
occurs in >50% almost always disappears by end of 1st trimester mild cases reassure and avoid drugs
|
|
|
Morning sickness NON-PHARM |
— small, frequent meals |
|
|
Medication for morning sickness |
— pyridoxine 50–100 mg bd |
|
|
Hyperemesis gravidarum |
This is severe vomiting in pregnancy, which may result |
|
|
Mx of Hyperemesis |
• Test urine—MCU (micro-culture of urine); ketones: if |
|
|
Heartburn |
Non-pharmacological treatment such as frequent small meals, avoidance of bending over and elevation of the head of the bed are the mainstays of treatment. |
|
|
Cramps |
Pregnant women are more prone to cramp. If it develops |
|
|
Varicose veins |
These can be troublesome as well as embarrassing. Wearing special supportive pantyhose (not elastic bandages) is the most comfortable and practical way to cope, in addition to adequate rest |
|
|
Haemorrhoids |
Haemorrhoids in the later stages of pregnancy can |
|
|
Dental Hygiene |
Dental problems can worsen during pregnancy so |
|
|
Back Pain |
Advice about lifting, sitting and resting • First trimester: use normal physical therapy and advise exercises • Second trimester: use supine side lying rotation and sitting techniques only; advise exercises. |
|
|
Guidelines to back pain Tx in pregnancy |
Guidelines for treatment |
|
|
Exercise guidlines in pregnancy |
Advise the patient that walking is an excellent exercise. |
|
|
Carpal tunnel syndrome |
Splinting of the hand and forearm at night might be |
|
|
Hypotension |
This is due to increased peripheral circulation and |
|
|
Pruritus |
Generalised itching (pruritus gravidarum) is usually |
|
|
Obesity |
Obesity is associated with increased obstetric morbidity, |
|
|
Breathlessness of pregnancy |
physiological breathlessness of pregnancy |
|
|
Supplements in pregnancy |
iron, folic acid, B12, iodine, vit D |
|
|
Iron |
Iron is not routinely recommended for pregnant women |
|
|
Folic acid |
Folic acid is advised for all women contemplating |
|
|
Vitamin B12 |
Vitamin B12 is essential for the developing fetus and if |
|
|
Iodine |
It is recommended, for pregnant and lactating women |
|
|
Vitamin D |
There may be a case for routine testing but it is advisable |
|
|
Advice on when to seek medical help |
• If contractions, unusual pain or bleeding occur before term |

