![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
68 Cards in this Set
- Front
- Back
|
What groups are considered to be microbic?
|
1. Bacteria
2. Protozoa 3. Fungi |
|
|
What microbe has the following properties?
1. Spend their lives in a fluid extracellular environment, although some spend their time inside host cells. 2. Humoral response is usually adequate to clear these microbes 3. These microbes that are intracellular usually invade phagocytes, where humoral response have know access to them. May be cleared by either CD4 or CD8 cellular responses |
Bacteria
|
|
|
What microbe has the following properties?
1. Can be either extracellular or intracellular 2. Extracellular can be susceptible to the actions of antibodies although, unlike bacteria, their antibody-mediated destruction appears to be predominantly based on opsonization and phagocytosis with a lesser role for complement-mediated lysis. 3. These intracellular microbes are cleared by the same methods that are effective for intracellular bacteria |
Protozoa
|
|
|
What microbe has the following properties?
1. Not very virulent 2. Can trigger a variety of immune responses including the production of high levels of specific antifungal antibodies. However, antibodies appear to be ineffective in clearing fungal infections although they can become the basis for hypersensitivity responses triggered by fungal infection. Instead, inflammatory cell-mediated DTH responses are the primary means of clearing these infections |
Fungi
|
|
|
What is the ribosomal structure for prokaryotes?
|
70S (50S + 30S)
|
|
|
What is the purpose of a positive stain?
|
Direct bonding of the stain to the tissue under study. Most stains are positive.
|
|
|
What is the purpose of a negative stain?
|
1. Contrasts a thin specimen with an optically opaque stain
2. Allows the specimen to appear very light against a black surface 3. Has a mild preparation method and should not be used with infectious agents as the operator can potentially be infected |
|
|
What is the correlation among infectious disease, virulence, dosage, portal of entry and resistance of host?
|

Here it is
|
|
|
What are some characteristics determining virulence?
|
1. Protection against non-specific destruction in the body.
2. Invasiveness and tissue destruction |
|
|
What is the pathogenic effect type specific polysaccharide from the capsule, which is found on S. pneumonia, Klebsiella pneumonia, bacillus anthracis, yersinia pestic?
|
NON-RECOGNITION: Inhibits phagocytic adherence and capture
|
|
|
What is the pathogenic effect M-Protein and Waxes/Mycoic acids (acid fast cell wall) from the cell wall of Streptococcus, Mycobacterium Tuberculosis?
|
NON-DESTRUCTION: Inhibits phagocytic digestion
|
|
|
What is leucocidin?
|
Leucocidin is a protein that kills WBCs providing intracellular resistance to destruction
|
|
|
How do bacteria invade and destroy tissue?
|
1. Have enzymes that damage human cells
2. Have enzymes that degrade intracellular materials or inactivate local response factors 3. Trigger immunopathologic damage to tissue |
|
|
What are viruses virulence based on?
|
Viruses depend on the host for replication, so some of its virulence is based on the properties of the host.
|
|
|
How do viruses invade and inflict tissue destruction?
|
1. Cytolysis
2. Render infected cells dysfunctional 3. Unchecked and rapid replication 4. Immunopathologic tissue destruction |
|
|
How do fungi invade and inflict tissue destruction?
|
1. Direct extension of growth
2. Immunopathologic tissue destruction |
|
|
What microbes are generally not very virulent, but decrease host resistance?
|
Fungi
Most are not capable of living or growing in the host, unless the host is compromised. The inflammation associated with fungi is due to your body attempting to fight it off. |
|
|
What is toxigenicity based upon?
|
Bacterial cells producing exotoxins and endotoxins.
|
|
|
What contributes to toxigenicity by:
1. Elaborating toxic proteins from living cells or when cell undergoes autolysis 2. All are proteins 3. Often not encoded on bacterial genome but rather on PLASMID DNA or presence of bacterial virus DNA 4. Protein _____toxins can be used to form ANTITOXINS |
Exotoxins
|
|
|
What are antibodies that detoxify toxins?
|
Antitoxins
|
|
|
What is the term for something that is immunogenic but non-toxic and is created in a lab based on the original exotoxin?
|
Toxoid
|
|
|
What are detoxifying or neutralizing immunoglobulins created by the host in response to the toxoid?
|
Antitoxins
|
|
|
How are antitoxins made?
|
Toxin (convert to) Toxoid (inject into host) Antitoxins
|
|
|
What is this contributor to toxicity?
1. LPS of the bacterial cell wall. Especially common in gram negative cells 2. Constituent part of the bacterial cell wall 3. Produce effects when large numbers of bacterial cells grow in the body, especially when they gain access to blood stream (gram negative sepsis) 4. Physiologic effects includingfever, low blood cell count, inflammation, Hypotensive shock, coagulation, septic shock? |
Endotoxins from bacterial cells
|
|
|
What are the physiological effects produced by endotoxins?
|
1. Fever
2. Low blood cell count 3. Inflammation 4. Hypotensive Shock 5. Coagulation 6. SEPTIC SHOCK |
|
|
What is the lipid portion of the cell wall that is toxic called?
|
Lipid A
|
|
|
How are fevers activated?
|
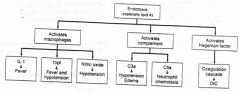
Lipid A endotoxin activates macrophages which trigger IL-1 to induce fever
|
|
|
How is fever and hypotension activated?
|
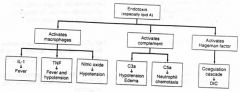
Lipid A activates macrophages which trigger TNF resulting in fever and hypotension.
|
|
|
How is hypotension activated?
|
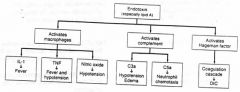
Lipid A endotoxin activates macrophages, triggering Nitric Oxide leading to hypotension.
|
|
|
How is hypotension edema activated?
|
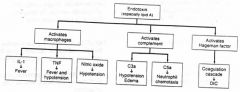
Lipid A endotoxin activates complement triggering C3a leading to hypotension edema.
|
|
|
How is neutrophil chemotaxis activated?
|
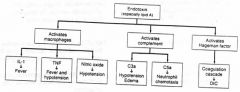
Lipid A endotoxin activates complement leading to C5a causing Neutrophil Chemotaxis.
|
|
|
What type of toxins are POLYPEPTIDES with molecular weights between 10000 and 90000 Daltons?
|
Exotoxins
|
|
|
What type of toxin is EXCRETED by living cells?
|
Exotoxins
|
|
|
What type of toxin is RELATIVELY UNSTABLE to temperatures above 60 degrees C?
|
Exotoxins
|
|
|
What type of toxin is ANTIGENIC (stimulates the formation of antibodies)?
|
Exotoxins
|
|
|
What type of toxin can be converted to a toxoid?
|
Exotoxins
|
|
|
What type of toxin DOES NOT PRODUCE FEVER in the host (except TSS)?
|
Exotoxin
|
|
|
What type of toxin is VERY TOXIC in microgram quantities to laboratory animals?
|
Exotoxin
|
|
|
What type of toxin is a low molecular weight component of LPS; LIPID A is the toxic component
|
Endotoxin
|
|
|
What is the gold standard for what is causing fever?
|
Isolating the organism
|
|
|
What type of toxin comes from PART OF THE CELL WALL of gram-negative bacteria that can be released when the cell lyses or during vegetative growth?
|
Endotoxin
|
|
|
What type of toxin is relatively STABLE to temperatures above 60 deg C for several hours with no loss of activity?
|
Endotoxins
|
|
|
What type of toxins are NOT ANTIGENIC (lipid A) meaning that cannot form antibodies against them
|
Endotoxins
|
|
|
What is the best indicator of an inflammatory response occuring within the body?
|
C reactive protein
|
|
|
What type of toxin CANNOT be converted to a toxoid?
|
Endotoxins
|
|
|
What type of toxin PRODUCES FEVER in the host?
|
Endotoxin
|
|
|
What type of toxin is WEAKLY toxic; hundreds of microgram quantities required to be lethal for animals?
|
Endotoxins
|
|
|
What is the value for shock?
|
LOW BLOOD PRESSURE
|
|
|
What Activates DIC?
|
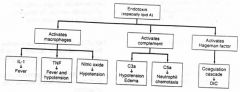
Lipid A endotoxin activates Hageman factor triggering the coagulation cascade to release DIC
|
|
|
What is immunogenic but non-toxic and is created in a lab and based on the original exotoxin?
|
Toxoid
|
|
|
What are detoxifying or neutralizing immunoglobilins. They are created by the host in response to the toxoid?
|
Antitoxins
|
|
|
What is the pathogenic effect of the extracellular enzyme Collagenase from C. perfringens?
|
Connective tissue invasion
|
|
|
What is the pathogenic effect of the extracellular enzyme Lecithinase from Clostridial sp.?
|
Cell membrane destruction
|
|
|
What is the pathogenic effect of the extracellular enzyme Protease from Clostridial sp.?
|
Protein break down
|
|
|
What is the pathogenic effect of the extracellular enzyme Lipase from Clostridial sp. and S. aureas?
|
Lipid breakdown
|
|
|
What is the pathogenic effect of the extracellular enzyme Elastase from Ps. aeruginosa?
|
Destruction of elastin tissues
|
|
|
What is the pathogenic effect of the extracellular enzyme Coagulase from S. aureas?
|
Inhibits phagocytosis
|
|
|
What is the pathogenic effect of the extracellular enzyme DNAase from S. areas?
|
DNA breakdown
|
|
|
What is the pathogenic effect of the extracellular enzyme Hemolysins from S. pyogenes and Clostridial sp.?
|
RBC lysis
|
|
|
What is the pathogenic effect of the extracellular enzyme Hyaluronidase from S. aureas and S. pyogenes?
|
Hyaluronic acid; epithelial tissue spread
|
|
|
What is the pathogenic effect of the extracellular enzyme Streptokinase from S. pyogenes?
|
Clot dissolution
|
|
|
What is the virulence of Encapsulated S. Pneumoniae?
|
Virulent Strain. The encapsulated form is found in virtually all organisms causing pneumonia.
|
|
|
What is the virulence of NON-encapsulated S. pneumoniae?
|
Avirulent Strain. Does not typically cause disease.
|
|
|
What is leucocidin?
|
Leucocidin is a protein that kills WBCs. So, it has Non-destruction/resistance to killing.
|
|
|
How do Clostridial enzymes damage human cells?
|
1. Only grows in necrotized tissue (anearobic bacteria)
2. Causes Necrosis of tissues 3. Produces exoenzymes that are highly necrotizing 4. As the tissue is dying, the organism will create a wave front through which the tissue is spreading 5. This is why we amputate gangrene -- necrotizing front will just keep moving if we don't |
|
|
What bacteriae cause Toxic Shock Syndrome?
|
S. Aureas or S. Pyrogens
|
|
|
How does Toxic Shock Syndrome occur?
|
Exotoxin antigens bind to receptors on surface of lymphocytes, which cause release of IL-1, TNF and cytokines which can cause TSS
|
|
|
What is attacked on T-cells when HIV patients are infected?
|
CD4 receptors are attacked
|

