![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
38 Cards in this Set
- Front
- Back
|
Describe the morphology and the characteristic features of Rhodococcus species.
|
a. plemorphic (come in multiple shape): cocci to long rods.
b. G+, non-spore-forming bacilli c. may be weakly acid-fast due to myocolic acids in cell wall d. facultative anaerobes e. catalase positive f. multiple strains- vary in virulence (Rhodococcus equi = pathogenic) |
|

|
Left: log growth phase; note the rod shaped bacT (bigger and stains darker)
Right: stationary growth phase; note the cocci shaped bacT |
|
|
Where will you most commonly find Rhodococcus species?
|
a. ubiquitous in environment world wide.
b. survives in soil: enriched with organic matter (herbivore feces); neutral pH c. intestine in herbivores mostly, and other mammals, birds. |
|
|
How are Rhodococcus species transmitted?
|
a. primarily via ingestion and inhalation
b. via mucous membrane exposure also possible |
|
|
What kind of virulence factors does Rhodococcus equi produce?
|
a. capsule
b. lipoteichoic acid and peptidoglycan(located in G+ cell wall) activate macrophages --> release of proinflammatory cytokines--> inflammatory cascade c. virulence plasmid * pathogenicity island encoding 7 virulence-associated proteins(vap) * Vap A: expression increased at body temp; required for replication within macrophages |
|
|
What is the pathogenesis for Rhodococcus species?
|
Exposure to the bacT--> opsonized by complement components (C3b) --> phagocytosis via Mac-1 component receptor (CR3, CD11b/CD18) --> multiplies within macrophage (VapA)--> cell death, abscess, granulomatous inflammation
|
|
|
What are some of the clinical conditions associated with Rhodococcus species?
|
A. foal pneumonia (1-6mo of age)
a. tachypnea, dyspnea (most common) b. cough, mucoppurulent nasal discharge, fever c. chronic pyogranolomatous bronchopneumonia with suppurative lymphadenitis d. high mortality rate (affected by the virulence of the organism and ani's immune status) B. Abdominal disease a. up to 50% of foals with pneumonia b. may occur in older animals c. enterocolitis, typhilitis(cecitis), abscesses, peritonitis C. other sites in horses a. nonseptic polyarthritis (filled with neutrophils) b. septic arthritis, osteomyelitis c. metritis (inflammation of the uterus) rare D. swine a. cervical L.N. lesions-grandulomatous b. carcass condemnation E. other species a. pyogranulomatous lymphadenitis, abscesses(any site) pyogranulomatous pneumonia, hepatitis, osteomyelitis. |
|
|
Whats the zoonotic potential for Rhodococcus equi?
|
A. clinical conditions
a. immunocompetent: localized skin lesions, abscesses b. immunocompromised: pneumonia, lymphadenitis B. transmission a. people exposed to same environmental sources as horses direct transmission from horses. |
|
|
What lab diagnosis are used for R. equi?
|
A. culture trancheobronchial aspirate (Note: often + in nasal swab or feces of horses)
a. culture may take 24 hrs to grow b. catalase + c. can test isolates for virulence factors B. PCR (may not be any more sensitive than culture test) |
|
|
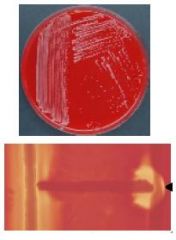
top: mucoid colonies on blood agar - may be pinkish-red after prolonged incubation.
bottom: CAMP -type rxn with S. arureus or Corynebacterium pseudotuberculosis. |
|
|
What are the primary self immunity agains R. equi?
|
cell mediated (Th1) followed by humoral (if the animal has anti-VapA antibodies, it is more protected)
|
|
|
What are the preventative measures against R. equi?
|
A. no vaccine available currently
B. management (hygiene and mare/foal density) C. Hyperimmune plasma (high risk foals) D. antibiotic prophylaxis (high risk foals; last resort) |
|
|
What are the treatments for R. equi?
|
A. erythromycin(may penetrate the bacT) plus rifampin (rapid developing resistance)
note: enterocolitis B. Azithromycin (entercocolitis) C. supportive care |
|
|
Describe the morphology and characteristic features of Corynebacterium.
|
a. pleomorphic, nonmotile, non-spore-forming bacilli
(coccoid, filamentous, club, rod forms; gull/chinese character) b. catalase + c. facultative intracellular d. more than 30 species e. species of major veterinary importance that have zoonotic potential: C. pseudotuberculosis and C. renale group |
|
|
Where will you most commonly find Corynebacterium pseudotuberculosis?
|
a. occurs in normal animals: skin and mucous membranes
b. survives well with organic matter, moisture, purulent material. c. susceptible to heat (60 C/ 140 F), disinfectants |
|
|
What are the mode of transmission for Corynebacterium pseudoturberculosis?
|
a. direct contact-skin wounds, contaminated instruments
b. arthropod vectors |
|
|
What are some of the clinical conditions associated with Corynebacterium pseudoturberculosis?
|
a. causes lymphadenitis of sheep and goats
b. ulcerative lymphangitis (inf. of lymph vessels) of horses, cattle( systemic dz rare) skin abrasion--> usually beings at fetlock area, may ascend --> swelling, abscesses along lymphatics --> rupture --> ulcerated areas. c. pectoral abscesses of horses bings with cutaneous babronemiasis (primarily in western US; seasonal peak in autumn) d. abscesses and mastitis of cattle |
|
|
What kinds of virulence factors does Corynebacterium pseudoturberculosis contain?
|
A. cell wall lipids: inhibit phagocytosis and lysis in phagosome; may contribute to host cell damage.
B. Lipoteichoic acid and peptidoglycan activate macrophages --> release of proinflammatory cytokines C. Phospholipase D (exotoxin) a. enhances survival in phagocytic cells and dissemination from site of entry. b. hydrolyzes ester bonds in sphingomyelin in cell membranes c. macrophage, neutrophil, endothelial cell dmg. d. inactivates complement e. dermal necrosis |
|
|
What is the pathogenesis for Corynebacterium pseudoturberculosis?
|
skin abrasion--> multiplication, pyogranulomatous inflammation--> abscess develops in layers, thick fibrous capsule--> dissemination via lymphatics (progressive debilitation possible)
|
|
|
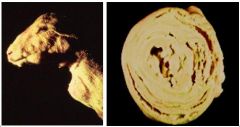
gross appearance for Corynebacterium pseudotuberculosis
note the onion ring arrangement on the right. |
|
|
What lab diagnosis are used for Corynebacterium pseudotuberculosis?
|
a. colony isolation and may take several days to grow
b. small white colonies may have mild beta hemolysis. |
|
|
What are the primary immunity against Corynebacterium pseudotuberculosis?
|
cell-mediated responses followed by humoral
|
|
|
What are the treatment option for Corynebacterium pseudotuberculosis?
|
a. poor antibiotic penetration
b. vaccination labeled for sheep c. prevention is important |
|
|
Where will you most commonly find Corynebacterium renale group?
|
they are normal flora of the lower UG tract of cattle.
|
|
|
What is the mode of transmission for Corynebacterium renale?
|
a. endogenous infection
b. direct contact c. contact with infected urine d. tissue damage increases likelihood of dz. |
|
|
What are some of the clinical conditions associated with Corynebacterium renale group?
|
Ruminants:
a. cyctitis and ascending pyelonephritis of cattle and other species b. problems most often in cows near parturition c. rarely in bulls or sheep d. may be fatal e. sporadic occurence Small ruminants: a. posthitis: necrotizing inflammation of prepuce b. ulcerative vulvitis also occurs |
|
|
What virulence factors does Corynebacterium renale group contain?
|
a. adhesin-fibrillar protein on cell surface(pili); may help resist phagocytosis
b. urease- hydrolyzes urea to ammonia which directly injures urothelium |
|
|
Whats the pathogenesis for Corynebacterium renale group?
|
endogenous or introduced bacT--> adhesin-mediated attachment to urothelium--> replication and urease production --> urothelium dmg, chronic inflammation --> cystitis, ureteritis, pyelonephritis.
|
|
|
What are the lab diagnosis for Corynebacterium renale group?
|
a.urine for suspected pyelonephritis
b. colonies may be off white or tan c. no hemolysis on blood agar |
|
|
what are the immunity, treatment, and prevention for Corynebacterium renale group?
|
a. protective immune response not defined
b. attempt systemic antibiotic treatment for pyelonephritis c. no vaccines |
|
|
What are the morphology and characteristics for Arcanobacterium pyogenes?
|
a. economically important pathogen/opportunist of ruminants and swine
b. G+, non-spore-forming, pleomorphic rod; may decolorize easily c. catalase +, facultative anaerobe d. susceptible to drying, heat (60 C), disinfectants |
|
|
Where will you mostly commonly find Arcanobacterium pyogenes?
|
a. normal flora on mucous membranes and skin of cattle, sheep, swine, and others.
b. most infections likely endogenous |
|
|
What is the mode of transmission for Arcanobacterium pyogenes?
|
a. usually opportunist; may be primary pathogen
b. spread by flies postulated for mastitis |
|
|
what virulence factors does arcanobacterium pyogenes contain?
|
A. extracellular matrix binding proteins: bind to collagen, fibronectin, promote adhesion
B. Neuraminidases: cleave sialic acid on host cells, exposes receptors for improved adhesion C pyolysin (PLO): binds to cholesterol in cell membranes --> forms pores --> cell damage, death (may also alter cytokine expression) D. proteases, DNAses: probably to relase nutrients (unknown significance) |
|
|
Whats the pathogenesis for Arcanobacterium pyogenes?
|
Tissue injury or other infection --> adheres, multiplies--> inflammatory response, tissue dmg --> lesions: abscesses, often with thick fibrous capsule; pyogranulomatous inflammation.
|
|
|
What are some of the clinical conditions associated with Arcanobacterium pyogenes?
|
A. cattle, other ruminants
a. mastitis, abortion, metritis, pyometra b. liver abscesses, endocarditis c. abscesses, pyogranulomatous inflammation at multiple other sites d. disseminated disease possible B. Swine a. abscesses at various sites c. other purulent processes C. Other species a. cause abscesses, other purulent processes in many species. |
|
|
Whats the diagnosis for Arcanobacterium pyogenes?
|
a. clinical signs, history
b. submit pieces of tissue for culture c. growth on blood agar may require up to 48 hrs. d. small, translucent hemolytic colonies. |
|
|
What are the immunity, treatment, and prevention for Arcanobacterium renale?
|
a. vaccines of questionable value
c. susceptible in vitro to many antibiotics; difficult to reach site of infection due to encapsulated abscesses. d. local treatment may help e. management important for prevention. |

