![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
30 Cards in this Set
- Front
- Back
|
Whats the basic morphology and characteristics for Erysipelas?
|
a. G+, non-spore-forming, facultative anaerobe
b. short rods, rounded ends (may grow as long, non branching filaments) c. catalase - d. nonmotile e. causes infections in swine, turkeys, humans |
|
|
What are the virulence factors for Erysipelas rhusiopathiae?
|
a. cell wall
b. capsule c. neuraminidase: 1) cleavage of sialic acid residueson endothelial cells --> thrombus formation; 2) thrombus may form diamond skin 3) virulent strains produce high amounts --> acute septicemic infections |
|
|
Whats the pathogenesis for Erysipelas
|
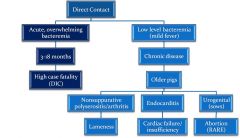
|
|
|
What are some of the clinical signs associated with Erysipelas rhusiopathiae?
|
A. Swine
a. acute erysipelas: activation of macrophages by cell wall peptidoglycan--> TNF -alpha --> DIC (can occur concurrently with "diamond skin" dz) b. "diamond skin" : almost pathognomic, can occur concurrently with acute phase, less severe form- infection may be limited to skin, deposition of Ag-Ab complexes in SQ vasculature --> thrombus B. Turkeys a. acute septicemia b. swollen snood (almost pathognomonic C. Sheep a. polyarthritis b. entry via umbilicus/wounds |
|
|
Whats the primary immune response for Erysipelas?
|
a. Humoral
|
|
|
Whats the prevention for Erysipelas?
|
A. vaccine
a. sows/gilts, pre- breeding b. boars (2x/yr) c. grower pigs B. age-segregation C. all-in; all-out |
|
|
What is the treatment for Erysipelas?
|
Penicilin may be used in both swine or turkeys.
|
|
|
Is Erysipelas zoonotic?
|
yes, people who are more susceptible to Erysipelas are:
a. veterinarians b. abattoir wrokers c. fish handlers Clinical signs: a. swelling at entry site b. sepsis, endocarditis &/or septic arthritis. |
|
|
What is the general morphology and characteristics for streptococcus?
|
a. G+ nonmotile cocci to ovoid
b. decolorize easily, especially older colonies (> 18 hrs; appear G-) c. single, pairs to long chains (divide in one plane) d. capsule in some species gives colonies a mucoid appearance. e. facultative anaerobes f. catalase negative |
|
|
Where will you most likely find streptococcus?
|
a. widely distributed
b. environmentally resistant c. colonize skin, GI tract, genital tract, upper respiratory tract d. |
|
|
What is the mode of transmission for Streptococcus?
|
a. direct contact
b. fomites c. ingestion d. inhalation |
|
|
How would you classify streptococcus?
|
A. hemolysis on blood agar
a. alpha - green discoloration (Hb --> met Hb) b. beta - clearing of agar around colony (erythrocytes lysed; most pathogens in the beta hemolytic group) c. Gamma - non-hemolytic (most nonpathogenic) B. Lancefield groups a. grouping based on Ab to surface carbohydrate Ag. b. categorized in series of letters |
|
|
What are some of the virulent factors found in Streptococcus?
|
A. adhesins
a. multiple surface proteins that bind extracellular matrix b. M prot 1) mediates attachment to CD46 2) binds to extracellular matrix prot; may coat surface of bacT with fibronectin (camouflage) 3) C4b binding-reducing phagocytosis 4) bind complement-control prot.- preventing opsonization 5) bind Fc portion of Ig's --> disrupt classical pathway B. Cell Wall C. Capsule -- hyaluronic acid 1) poorly antigenic; 2) does not bind complement well D. Toxins, enzymes 1) streptolysin S (SLS): b-hemolysis; flesh eating BacT. 2) streptokinase 3) streptococcus Dnases E. Leukocidal toxin ( S. equi) F. Acid production (S. muntans) tooth decay |
|
|
Streptococci pyogenes
|
a. Group A (GAS)- at least 80 types
b. human pharyngitis, scarlet fever, rheumatic fever, glomerulonephritis, toxic shock syndrome, "'flesh-eathing" BacT. c. rarely associated with bovine mastitis d. not considered part of normal flora of veterinary species (person--> person; pet --> person is rare) |
|
|
Streptococci pneumoniae
|
Does not have a Lancefield Classification
a. tend to occur in pairs, also revered to as "diplococcus" b. important human pathogen (human is a reservoir: anthroponosis) c. pneumonia in guinea pigs, horses, nonhuman primates d. menigitis e. aerosol, asymptomatic carriers f. uncommon cause of infections in other species |
|
|
Streptococci agalatiae
|
a. Group B - 5 types
b. contagious mastitis in dairy cattle c. obligate mammary pathogen; ID aided by CAMP test (hemolytic synergism: Staphylcoccal beta toxin and "CAMP factor" of S. agalactiae) d. sm. ruminants (mastitis); horses (genital tract infections); dogs (vaginal, skin infections); Cats (kidney, uterine infections); Humans (neonatal sepsis/meningitis) |
|
|
What type of Streptococcus are involved in bovine mastitis?
|
a. S. agalactiae
b. S. dysgalactiae ssp. dysgalactiae (alpha or gamma hemolysis) c. S. uberis (alpha/gamma hemolysis) d. others (e.g. S. pyogenes) |
|
|
Streptococcus dysgalactiae ssp. dysgalactiae
|
Group C
a. A/Y hemolytic b. bovine mastitis c. lamb polyarthritis (septic) |
|
|
Streptococcus dysgalactiae ssp. equisimilis
|
Group C
a. B hemolytic b. uncommon cause of abscesses, UTI in dogs c. Occasionally wound infections of horses |
|
|
Streptococcus equi ssp. equi
|
Group C
a. B hemolytic b. encapsulated c. Equine "strangles" 1) fever, purulent rhinitis/pharyngitis 2) upper airways, guttural pouches 3) abscessed L.N. typically mandibular and pharyngeal 4) may become systemic 5) chronic carrier state possible d. baterin available |
|
|
Streptococcus equi ssp. zooepidemicus
|
Group C
a. B hemolytic b. encapsulated c. many serotypes d. Horses: 1) asymptomatic carriage- oral cavity, pharynx, respiratory tract 2) opportunistic - resp and genital tracts 3) other infections (wounds, osteomyelitis, arthritis) e. occasional infections in other species: cervical lymphadenitis (guinea pigs) |
|
|
Streptococcus suis
|
Group S & R
a. alpha hemolytic b. Type 2 causes meningitis, srthritis, endocarditis, abortion in swine 1) contagious via tonsillar carriage 2) zoonotic: menigitis, otitis, septicemia --> can be fatal (handle/eat uncooked pork) c. Type 1 causes neonatal septicemia, polyarthritis of young pigs d. management very important for prevention (vaccine not routinely used) |
|
|
Streptococcus porcinus
|
Group E
a. B hemolytic b. L.N. abscesses in swine: 1) cervial lymphadenitis; 2) jowl, head, neck abscesses; 3) carcass condemnation |
|
|
Streptococcus canis
|
Group G
a. B-hemolytic b. commensal of skin, mucosa of dogs and cats c. neonatal infections d. some suppurative conditions e. Toxic shock syndrome, necrotizing fasciitis in dogs and cats |
|
|
Streptococcus bovis (or S. equinus)
|
Group D
a. occurs in alimentary tract (horse, ruminant) b. nonpathogenic c. rarely zoonotic |
|
|
What are the general morphology and characteristics for Enterococcus?
|
Group D Enterococci
a. G+ b. catalase negative c. cocci to ovoid shape in pairs, chains d. A/Y hemolysis c. facultative anaerobe e. commensals (GI) f. Multiple-antibiotic resistant 1) Vancomycin Resistant 2) "jumping genes" 3) vanA- cleaves vancomycin |
|
|
What are some of the clinical findings associated with Enterococcus?
|
a. associated with wounds or any compromised site in most species
b. Dogs and cats: 1) asymptomatic colonization 2) UTI (nosocomial and community- acquired) 3) otitis externa c. puppies, kittens, foals, calves, piglets, and infant rats 1) diarrhea-associated Enterococci (E. durans, E. hirae, E. villorum) |
|
|
What are the treatments for B-hemolytic Streps?
|
Sensitive: 1) Penicillins 2) Cephalosporins
Resistant: 1) aminoglycosides 2) Fluoroguinolones 3) Tetracycline |
|
|
What are the treatments for Enterococci?
|
important to perform culture sensitivity tests
Resistant to: 1)B-lactams 2) Aminoglycosides 3) Fluoroguinolones 4) potentiated sulfas b. vancomycin-R vet med isolates have been found |
|
|
useful summary for Staph, Strep, and Enterococcus.
|
a. most A and Y hemolytic species are found in normal flora w/exception of S. dysgalactiae, S. uberis, S. suis
b. B hemolytic species are usually pathogens but may be isolated in some cases from normal animals c. Group D enterococci are normal flora for most species and are opportunistic pathogens d. Enterococci inherently resistant to many antibiotics. |

