![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
26 Cards in this Set
- Front
- Back
|
Is Chlamydia species specific?
|
Yes - they don't cross to infect other species.
And every niche from the lowest to the top has Chlamydia in it. |
|
|
What are the common traits of Chlamydiae (there are four)?
|
1. Obligate intracellular pathogen. Develops in a vacuole, called the inclusion.
2- alternating developmental forms- 1: Elementary body- (EB) infectious, not metabolically active, cannot replicate. 2: Reticulate body (RB)- cannot infect, is metabolically active and can replicate. 3- unusual cell wall- lacks peptidoglycan. EB cell wall consists of disulfide-linked proteins. In EB: very rigid shell. In RB: cell wall absent. 4- All infections begin in mucosal epithelia- most primary disease confined to mucosae. |
|
|
What are the EB's and RB's of Chlamydiae?
|
Reticulate body (RB)- cannot infect, is metabolically active and can replicate. The intracellular form.
Elementary bodies are very stable - physically resistant. They are infectious. Analogous to spores/ unusual cell wall- lacks peptidoglycan (unlike spores). EB cell wall periplasm consists of disulfide-linked proteins forming a very rigid shell. In RB: cell wall absent. |
|
|
How is LPS special in Chlamydia?
|
Genus common antigen. The LPS is conserved across all vertebrate animals.
|
|
|
What are the diseases caused by chlamydiae?
|
As a generalization, mucosal diseases.
Wide variety of veterinary conditions: Arthritis, (sheep, etc.) Abortion (sheep, goats, etc.) ocular disease (bighorn, swine, guinea pigs) Pneumonia (koala, birds) Hepatitis (crocodiles, frogs) STIʼs (koalas, cows, etc.) Gill diseases (fish) Chlamydia-like organisms in clams |
|
|
What is the relationship between chlamydia and sheep?
|
“_abortion storm_” Commonly in first pregnancy of previously unexposed females- ( suggests protection possible).
• Sheep, some goats and cows- can be enzootic in sheep- 1-5% abortions. • Can increase to 30% in previously unexposed herds • Disease is primarily _placentitis_- huge titers of chlamydia. Fetal infection secondary to systemic ewe infection. Enzootic Abortion of Ewes (EAE) Late term abortions, stillbirths, and weak lambs. Occurs worldwide (except Australia, NZ) Most important in intensively managed sheep. Abortions occur during the last 2-3 wk of gestation regardless of when infection occurs. Ewes seldom abort more than once, but they remain persistently infected (that's important): Can shed C. abortus from their reproductive tract for 2-3 days before and after ovulation. Rams can be infected- sexual transmission (less common). |
|
|
How would you control chlamydia abortus in sheep?
Is it zoonotic? |
Control: Isolating affected ewes and lambs and treating in-contact ewes with long-acting oxytetracycline or oral tetracycline.
C. abortus bacterins are available and are effective in reducing abortions. A modified live vaccine is also available for use. Challenging to clean up a flock once established. Vaccination, hygiene, use clean replacement animals. C. abortus is zoonotic but human cases are rare. All have involved pregnant women, who developed life-threatening illness. Only in a few cases in which the fetus was delivered by cesarean section did the infant survive. Pregnant women should not work with pregnant sheep, especially if abortions are occurring. |
|
|
Is chlamydia susceptible to antibiotics?
|
Yes, but you need to know where it is.
|
|
|
What is the antibiotic resistant chlamydia? Since no others are resistant (yet), how did they get it?
|
Chlamydia suis. Got it from eating fish waste products. Stole it from their chlamydia.
|
|
|
How does Chlamydia cause arthritis or serositis? What strain causes it? Is it a common presentation for chlamydia?
|
Sheep and calves- almost always C.
pecorum • Diarrhea, infection of intestinal mucosa • Dissemination- joint inflammation • Animals stiff, reluctant to move, can affect many animals in a herd • Young animals seem to be more susceptible • Can have chlamydia in the joints/synovial fluid rare for chlamydia to go systemic |
|
|
What does chlamydia felis caus?
|
• C. felis- infects all mucosal surfaces
• Most often severe conjunctivitis, also respiratory infection • The bacterium can persist for a long time on mucosae Chlamydia can cause conjunctivitis in many species (including humans). |
|
|
How does avian chlamydiosis present?
Is it zoonotic? |
C. psittaci - probably the worst of the zoonotic chlamydias - causes fatal pneumonia.
• _________ infection- rapid dissemination • Pericarditis, pneumonias, air sac lesions, rhinitix, conjunctivitis, etc…. • Several strains/species can be involved- clinical signs are strain-dependent. • Avian strains can cause serious human disease (primarily psittacine strains) • Psittacine birds, pigeons, turkeys- specific strains for each species. |
|
|
What are the 4 common chlamydial diseases in koala?
What are the symptoms and the chlamydial species of concern? |
4 common koala chlamydial diseases: conjunctivitis which can cause blindness pneumonia urinary tract infections
reproductive tract infections, which can cause female infertility. The symptoms of chlamydia manifest as sore eyes, chest infections, and "wet bottom" or "dirty tail". Species of concern: Chlamydia pecorum and Chlamydia pneumoniae. |
|
|
What bacteria might lead to the extinction of koala?
|
Chlamydia
• Fertility rate reduced to non-sustainable levels • Chlamydia becomes a major problem when animals are stressed. Species of concern: Chlamydia pecorum and Chlamydia pneumoniae. |
|
|
Which human chlamydia leads to arthritis? Which to artherosclerosis?
And then what's the 3rd zoonotic one? |
C. trachomatis! Trachoma!
PID, LGV, other STDʼs! Reiterʼs syndrome- arthritis! C. pneumoniae! • pneumonia! • atherosclerosis! C. psittaci, etc.! • psittacosis, other zoonoses! |
|
|
What is the basics of chlamydial pathogenesis?
|
• Attachment and entry
• Directed remodeling of the intracellular environment (Chlamydia secrete proteins into host cells upon contact) • Dissemination and Persistence (persistence is important) • Host response (the chlamydia secrete proteins that make the host cell a bacteria factory) |
|
|
Why do chlamydia live in vacuoles?
|
You can evade the CD8-T-cell function because they aren't really in the cytoplasm, so their antigens don't get presented in a way that the T-cells can recognize.
You do need to bring proteins in. |
|
|
What chlamydial protein is important in slowing antigen presentation?
|
CPAFcp
|
|
|
What is the pathogenesis of chlamydial disease?
What is the fundamental battle? |
Chronic chlamydial infection is a great example of host participation in disease.
Some diseases- primary infection is associated with symptoms of concern. Pneumonia, abortion. Other diseases- host/pathogen interactions lead to disease. The fundamental battle: Protective vs.pathogenetic immune responses |
|
|
Are there vaccines against Chlamydia? How effective are they?
What is the trade-off in vaccinating (as shown in the cat vaccination study)? |
_Bacterins_ are useful for some chlamydial diseases. Variable efficacy.
“This heavy consistency emulsion forms a respository of granuloma at the site of injection.” Ovine abortion: Vaccines effective in reducing abortion and, perhaps, pathogen spread. Note that _Disease_ is less serious in vaccinated groups, but _shedding_ is no lower and is extended. |
|
|
What happens to chlamydia when stressed?
What can this effect the host immune response to do? |
"Aberrent Development"
Never turn into EBs, stay big RBs. Will stay that way until the stress is removed. Ampicillin triggers this. Then things get better, they go back to being EB and they go infect another cell. highly associated with immune mediated disease. |
|
|
What is the effect of penicillin on chlamydia?
|
Makes them into aberrant forms by stressing them.
All beta-lactams do. |
|
|
What characteristic of chlamydia is critical to their disease process?
|
Persistent, silent infections can result from low grade productive infections (i.e. EB’s and RB’s) or via production of aberrant forms. Persistence is likely critical to chlamydial disease processes.
|
|
|
What does injection of killed EB (form of Chlamydia) lead to?
|
Deleterious immune responses:
Injection of killed EB leads to worse disease- Chlamydial antigens, in the absence of infectious chlamydiae, can cause symptoms in animals that had previously been infected. |
|
|
The "ugly" infections of chlamydiea lead to the "bad" - how?
|
The "ugly" ones infect the eyes and female genital tract in aggressive, purulent discharge, but these are easy to treat. But the repeated, persistent infections, the chronic infection, leads to the immune-mediated response (the bad).
|
|
|
How does chlamydia cause blindness?
|
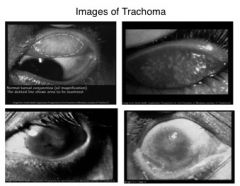
An example of the persistence of chlamydia causing worse disease. Mechanical damage caused by vascularization of the upper eyelid causes a persistent immune response and blindness.
|

