![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
26 Cards in this Set
- Front
- Back
|
Staphylococcus - gram +/-?
What is streptococcus? |
Both are Gram +
|
|
|
Where are staph infections normally?
Are they obligate parasites? What environments are they resistant to? |
Staphylococci are normal flora of many dermal surfaces
Hairy skin Teat Mucosal surfaces Facultative opportunistic pathogens Environmentally resistant- survives drying, heating, pH fluctuations, high salt (potato salad, food poisoning) |
|
|
What are the predominant animal species that most staph species infect?
|
Nearly 50 species associated with animals-
primarily birds and mammals. |
|
|
How is facultative different from opportunistic when defining pathogens?
|
Facultative pathogens are commensals in one spot and cause disease in another spot in an immunocompetent individual, whereas opportunistic pathogens can only attack when the host is immunocompromised.
|
|
|
Is staph catalase +/-?
What are the most severe acute pathogen of staph? |
All staphylococci are _catalase_ positive, Except two odd ones.
Coagulase positive staphylococci are the most severe _acute pathogens_, but wound infections/catheter-associated infections by Coag. Negative Staph are common. |
|
|
Do Staph build biofilms?
|
hell yes, big biofilmers
|
|
|
Staphylococcus has lots of virulence factors, there are two big surface ones - what are they?
|
Note: most aspects of staphylococcal disease in animals mirror
conditions in humans Possible exception: mastitis. Virulence factors largely the same too. Protein A: Staph. aureus cell surface protein binds _IgG at the Fc End___. Capsular polysaccharide: at least 11 capsular _serotypes__. Peptidoglycan and techoic acids may participate in adhesion and serious systemic disease. |
|
|
What are two important things about protein A?
|
This is a surface virulent factor of Staph.
1 - it is completely coated by it 2 - it binds with IgG so that IgG can't get it. It also bind von Willebrand's factor and helps form biofilms That seems like more than two. |
|
|
Why are capsular polysaccharides important to staph?
|
This is a surface virulent factor of Staph.
He's not really sure why it's so important, but it has at least 11 capsular serotypes - probably help it evade the immune system or phagocytosis. |
|
|
What is staph's interaction with neutrophils?
|
They have a unique interaction in which they can be taken in by one and then grow there.
|
|
|
What are the 4 exoenzymes of staph?
|
The important secretory enzymes:
Coagulase: Binds to __prothrombin_ to form a complex- “Staphylothrombin”- activates clotting cascade Function- masking of bacteria within clot hides organisms from host defense Lipases: may have activity against host cell membranes FAME- fatty acid metabolizing enzyme: may effect immune function Hyaluronidase: depolymerizes extracellular matrix- provides access to cell surfaces. Proteinases: possible activity against immune molecules. |
|
|
What are the hemolysins?
Which are important diagnostically? |
Roles in pathogenesis not altogether clear.
Alpha, beta, gamma, delta hemolysins. Alpha is most active- pore forming cytolysin. May be involved in sepsis, mastitis. Beta- sphingomyelinase, activity toward RBC (thus,_beta hemolysis_) Gamma- leukocidin : most strains from severe dermatitis are gamma hemolysin positive. Delta may be proinflammatory. Different hemolytic profiles are important in diagnostics- Keep track of: Alpha hemolysin is a pore forming cytotoxin, beta hemolysin is a sphingomyelinase reshemolysis. |
|
|
What is Enterotoxin/Toxic shock syndrome toxin (TSST)/canine type C
enterotoxin? |
What causes food poisoning from staph.
Superantigen activity Many variants, specificity for different host species. Lead to diarrhea/vomiting in several species- via activation of T cells in the ___lamina propria___ . Canine pyoderma- enterotoxin positive S.a. Toxin produced mucosally or systemically, works either on nervous system (enterotoxins) or on MHC/TCR interaction. Encoded on __pathogenicity islands__. |
|
|
What are the epidermolytic toxins and exfoliative toxins of staph?
|
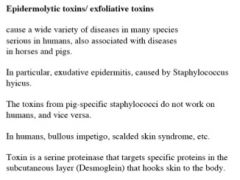
The "in particular" one is most important.
|
|
|
What are the three staphylococci that are most important in veterinary
disease? Which are coagulase positive? |
S. aureus: many species of animal
S. intermedius: dogs, ducks, pigeons, mink, horses S. hyicus: pigs, secondary infections in others. All are coagulase-positive. (S. hyicus has variability in Coag production). Several coagulase negative species are found in other species. |
|
|
Is staphylococcal mastitis contagious?
How severe are these infections? What role do superantigens play with these strains? |
Staphylococal mastitis: cows, goat, ewes
Contagious mastitis 25-30% of these infections are Staph- most common cause in many regions. Primary problem is $$ loss from _milk production_ A range of severity from subclinical to chronic Acute cases- high cell counts in milk. Milk clots, edema can also form May need to cull animals that have persistent infections. Antibiotics can be used. Many strains are Toxic Shock Toxin positive. TSST = staphylococcal superantigen. Role of TSST in veterinary disease not clear. |
|
|
How can we prevent staphylococcal mastitis?
|
dip teats in iodine/glycerol solutions. Dry after dipping
ointments maynot work against mastitis. wear gloves to reduce cross contamination of animals. work with clean animals before working with possibly affected animals |
|
|
Mastitis is an infection within the teat, what is a staph infection on the dermal surface that animals have in common with humans??
|
Impetigo, pustular dermatitis Many species affected, pustules on hairless areas of the body. Treat by cleaning, systemic antibiotics.
|
|
|
What does staphylococcus hyicus cause?
|
Exudative _epidermitis_: Greasy pig disease
Staphylococcus hyicus Extensive nonpruritic exudate Found in very young pigs Can range from 10-90% mortality, sudden onset. Acute disease: Suckling pigs. Chronic disease: Weaner pigs. Pathogen can be isolated from the_genital tract__ of healthy sows |
|
|
How does exudative epidermitis present?
Can you use antibiotics? |
Exudative epidermitis- Staphylococcus hyicus
Strains produce exfoliative toxin Piglets will be anorexic, depressed, febrile. Antibiotics are useful, hygiene important. Isolate symptomatic animals. |
|
|
Is there a homolog to greasy pig syndrome in human medicine?
|
Staphylococcal Scalded Skin
Syndrome Homologous etiology with Greasy Pig Disease. (exudative epidermitis caused by s. hyicus). S. hyicus (pig pathogen) produces toxins similar to S. aureus Human) exfoliative toxins- sloughing of skin. Similar toxins from different pathogens have different target specificities. |
|
|
What are the staph infections in poultry?
|
Chondronecrosis- femoral head necrosis
Systemic infection- commonly S. aureus- deposits in and around the growth plates of bones. Can interrupt blood supply to infected sites- microabscesses Etiology: secondary infection following trauma or holding in poor environments. “bumblefoot”: lesions in foot resulting from presence of a foreign body. May be caused by other bacteria too. “battery blister”: abrasive condition in muscles covering the sternum, pelvic region, or wing tips. Localized skin problems too. Many of the external or secondary infections by Staph. species can be addressed through changes in environmental conditions or animal handling practices. For poultry- problems common with poor quality cage wire, poor litter quality, generally dirty environments. |
|
|
What are staph infections in rabbits like?
|
Low virulence and high virulence strains.
Low- limited numbers of rabbits. High- epidemics in a rabbitry, can lead to chronic problems. Many clinical conditions: SubQ abscesses, rhinitis, exudative dermatitis, many other infections. he deemphasized this slide |
|
|
Do horses get staph infections?
|
Yes, similar spectrum as in other animals, many derm conditions. Saddle boils, equine acne.
S. aureus, s. hyicus are among many bacteria that can cause these. surface antisepsis, washing. |
|
|
What are staph infections in dogs like?
Many strains are blank positive - what is the blank? |
Superficial pyoderma, caused by Staphylococcus intermedius. Similar to S. intermedius is the predominant coag. positive staph on canine skin. Many strains are __enterotoxin__ positive.
|
|
|
Is staph becoming resistant? Can you equip animals with any immunity?
|
Note: no __long lasting immunity___ from any staphylococcal infections
Note Human Diseases- food poisoning (enterotoxin mediated) and Toxic Shock Syndrome (TSST mediated). Antibiotic resistance is a huge and growing problem. In human clinical settings: 95% of S. aureus infections are resistant to penicillin. 50% of S. aureus isolates are resistant to multiple antibiotics. 30% are resistant to methicillin A big deal: MRSA- Methicillin Resistant S. aureus. Certainly a problem in the veterinary clinic as well. |

