![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
53 Cards in this Set
- Front
- Back
|
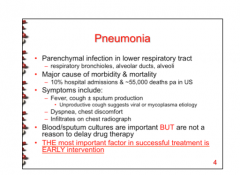
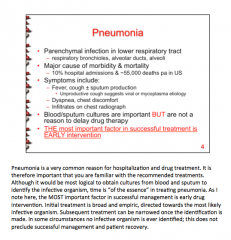
What is pneumonia? Symptoms? The most important factor in successful treatment? |
|
|
|
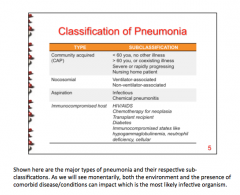
Wat are the four major types of pneumonia? When would you most likely see each? |
|
|
|
Define pneumonia. What are some common symptoms? Are drug/sputum cultures important? What is THE MOST important factor in successful treatment?
|
|
|
|
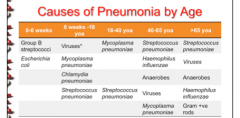
Most common causes of pneumonia by age: 0-6 weeks 6 weeks - 18 years old 18years old - 40 years old 40-65 years old >65 years old |
|
|
|
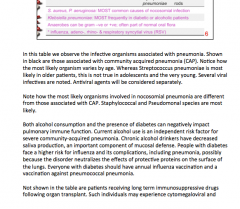
Most frequent cause of each: Nosocomial infection Diabetics or alcoholics
Can anaerobes be gram + or gram -? Part of normal what? What are the viruses in ages 6 wks-18 years? |
|
|
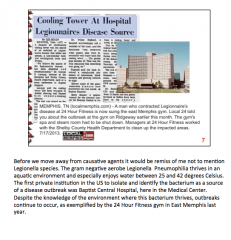
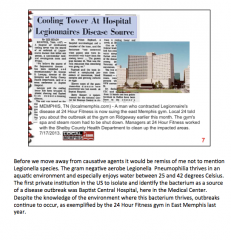
Look over Legionaire's disease. |
|
|
|
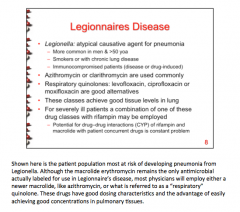
Does legionella cause pneumonia? In what sex and ages is it more common? Is smoking a risk factor? What about immunocompromised patients? What two ABs used most commonly? Good alternatives? What about for severely ill patients? Drug interactions?
|
|
|
Look over |
Look over |
|
|
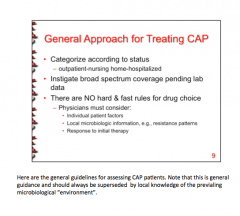
What is the first generation macrolide? What are the 2nd generation macrolides? 3rd generation? Draw the decision treat for treating CAP. |

|
|
|
Most common used drugs: Macrolides
Mechanism? |
Erythromycin (1st gen) Azithromycin (3rd gen)
50s ribosomal inhibitor blocking translocation |
|
|
Most commonly used drugs: Tetracyclines
Mechanism? |
Doxycycline
30s ribosomal inhibitor blocking protein synthesis |
|
|
Most commonly used drugs: Floxacins
Mechanism? |
Levofloxacin
DNA gyrase inhibitor preventing DNA replication |
|
|
Most commonly used drugs: Penicillins
Mechanism? |
Amoxicillin + Clavulonic acid Piperacillin + Tazobactam
Block cell wall cross-linking |
|
|
Most commonly used drugs: Carbonpenem
Mechanism? |
Meropenem
Blocks cell wall cross-linking |
|
|
Most commonly used drugs: Cephalosporins (CEFs or CEPHs)
Mechanism? |
Cefazolin (1st gen) Cefurozime (2nd gen) Ceftriaxone (3rd gen) Ceftazidime or Cefepime (both 3rd gen with antipseudomonal activity)
Inhibition of cell wall cross-linking |
|
|
Most commonly used drugs: Aminoglycosides
Mechanism? |
Gentamicin
30s ribosomal inhibitor |
|
|
MOR: Macrolides |
Ribosomal methylation & mutation of 23S rRNA active efflux |
|
|
MOR: Cyclines |
Decreased entry into and increased efflux from target insensitivity |
|
|
MOR: Fluoroquinolones Floxacins |
Mutation of DNA gyrase Active efflux |
|
|
MOR: Penicillins Cillins |
Drug inactivation (B-lactamase) Altered PBPs (target insensitivity) |
|
|
MOR: Cephalosporins CEFs or CEPHs |
Decreased permeability of gram -ve outer membrane (altered porins) Active efflux |
|
|
MOR: Aminoglycosides
|
Drug inactivation (amino glycoside modifying enzyme) Decreased permeability of gram -ve outer membrane Active efflux Ribosomal methylation |
|

Look over |

Look over |
|
|
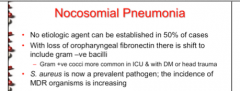
Nosocomial pneumonia: Is an etiologic agent sometimes established? With loss of oropharyngeal fibronectin there is a shift to include ______________________. When is gram + more common? What is the prevalent pathogen? |
|
|
|
What are the indicated drugs for nosocomial pneumonia? Alternative? What do all except vancomycin have activity against? What is vancomycin reserved for? |
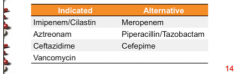
Gram negative Treatment of MRSA (IV) |
|
|
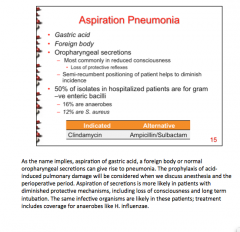
What two things causes aspiration pneumonia? When does it occur? What helps to diminish incidence? What are half of all hospitalized patients (bacteria)? Medication indicated and alternative? |
|
|
|
Mechanism of action and resistance: Clindamycin |
MOA = 50s ribosomal inhibitor blocking translocation Resistance = Methylation of binding site, enzymatic inactivation |
|
|
Mechanism of action and resistance: Vancomycin |
MOA = Binds D-alanyl-D-alanine terminus of the peptide precursor units, inhibiting peptidoglycan polymerase and transpeptidation reactions
Resistance = replacement of D-ala by D- lactate |
|
|
Oral dosing is simplest and most acceptable route of drug delivery for less severe infections. What is it reserved for? When could absorption be compromised? Look over slide. |

|
|
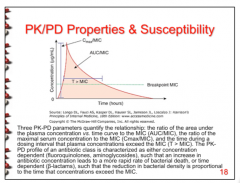
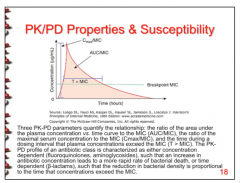
What three PK-PD parameters quantify the relationship? What is it characterized as? |
|
|
|
What does concentration dependent mean? What does time dependent mean?
What are pharmacologic sanctuaries? |
Concentration dependent = increase in AB concentration leads to a more rapid rate of bacterial death. (AUC/MIC, Cmax/MIC)
Time dependent = reduction of bacterial density is proportional to the time that concentrations exceed the MIC. (T > MIC)
Microbes in some tissues benefit. Poor penetration, prevailing pH, or local factors leading to increased drug inactivation protect these areas. |
|
|
Which drug classes have time above MIC as the predictive parameter? |
Penicillins, Cephalosporins, Carbapenems
(Time dependent = dosed more frequently and usually to keep MIC 30-50% of dose interval, sometimes prolonged or constant infusion). |
|
|
Which drug classes have 24 hour AUC/MIC as the predictive parameter? |
Aminoglycosides, Fluoroquinolones, Tetracyclines, Vancomycine, Macrolides, Clindamycin
(Concentration dep = once daily dosing = given at large concentrations over long intervals) |
|
|
Which drugs have Peak/MIC as the predictive parameter? |
Aminoglycosides, Fluoroquinolones |
|
|
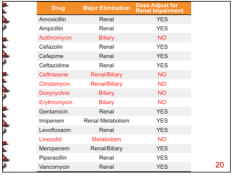
Which drugs eliminated by the kidney only? Should you reduce the dose in the case of impair renal function? |
|
|
|
For which drugs do you not have to worry about dose adjustment for renal impairment? How are they metabolized? |
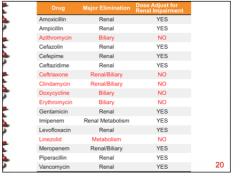
|
|
|
Major toxicity: Gentamicin |
Nephrotoxicity Ototoxicity Neuromuscular paralysis |
|
|
Major toxicity: Vancomycin |
Nephrotoxicity Ototoxicity Red Man's syndrome |
|
|
Major toxicity: Erythromycin |
CYP3A4/Pgp inhibitor Cholestatic jaundice QT prolongation |
|
|
Major toxicity: Imipenem |
Partial cross-reacivity with pen/ceph hypersensitivity Seizures |
|
|
Major toxicity: Meropenem |
Partial cross-reactivity with pen/ceph hypersensitivity Decreased coagulation |
|
|
Major toxicity: Levofloxacin |
Tendon rupture in adults Cartilage damage in young children |
|
|
Major toxicity: Doxycycline |
GI distress Teeth discolored Photosensitivity Decreased bone growth |
|
|
Major toxicity: Linezolid |
Bone marrow suppression Non-specific MAO inhibitor |
|
|
What will predispose a patient to a similar allergy with cephalosporin or a carbapenem? |
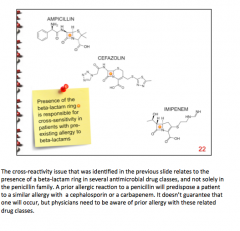
|
|
|
Which drugs are known teratogens? Which should you caution w/ breast feeding? Amoxicillin, Ampicillin, Azithromycin, Cefazolin, Cefepime, Ceftazidime, Ceftriaxone, Ciprofloxacin, Clindamycin, Imipenem, Meropenem, Vancomycin, Clarithromycin, Doxycycline, Erythromycin, Gentamicin, Levofloxacin, Linezolid, Metronidazole, Piperacillin, Trimethoprim |
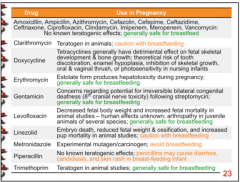
|
|
|
What do you combine with each? Why? Amoxicillin, Piperacillin, Ampicillin |
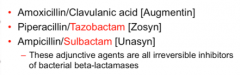
|
|
|
What do you combine with Imipenem? Why? |
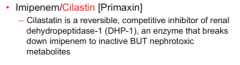
|
|
|
Why is daptomycin not used for pulmonary infections? |
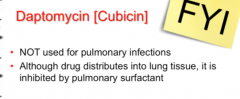
|
|
|
Bronchitis: Type of episodes in younger patients? Older? Which bacteria are responsible? In smokers? |
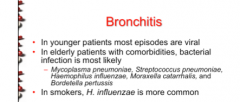
|
|
|
Indicated drugs for bronchitis? With resistance? |
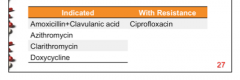
|
|
|
How do lung abcesses respond to medical management? When do they resolve? What are the anaerobes responsible? |
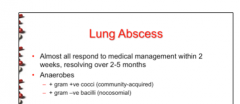
|
|
|
What drugs are appropriate? Why should metronidazole not be used alone? |
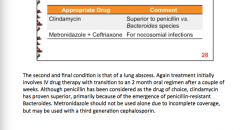
|

