![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
54 Cards in this Set
- Front
- Back
|
|
|
|
How does fetal cartilage differ from mature articular cartilage?
|
Fetal cartilage is well vascularized by vessels running through cartilage canals
|
|
|
What does ossification of primary centers of ossification result in at birth?
|
diaphyses of long bones are all are bony
|
|
|
What does ossification of secondary centers of ossification result in at birth?
|
Epiphyses, apophyses, and cuboidal bones are partly cartilaginous
|
|
|
What process results in longitudinal bone growth?
|
Endochondral ossification
|
|
|
How are chondrocytes arranged for endochondral ossification?
|
longitudinal columns which are parallel to the long axis of the bone
|
|
|
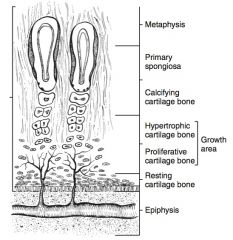
Zones of ossification:
|
From closest to the epiphysis to the diaphysis the zones are the zone of resting cartilage, the zone of proliferation, the pre-hypertrophic zone, the hypertrophic zone, and the zone of calcification
|
|
|
Describe zone of resting cartilage:
|
least metabolically active, and contains active chondrocytes
|
|
|
Describe zone of proliferation:
|
chondrocytes divide in a plane perpendicular to the long axis of the bone to increase bone length
|
|
|
Describe pre-hypertrophic zone:
|
chondrocytes become round and become encased in extracellular matrix
|
|
|
Describe hypertrophic zone:
|
chondrocytes stop dividing, increase in size and hypertrophy
|
|
|
Describe zone of calicification:
|
hypertrophied chondrocytes are replaced by mineralized bone and bone marrow
|
|
|
How does replacement of hypertrophied chondrocytes occur?
|
vascular invasion, resorption of cartilaginous maxtrix, recruitment of osteoblasts, osteoblasts deposit bone matrix
|
|
|
What influences the remodeling of cartilage to bone?
|
Biomechanical loading according to wolfe’s law
|
|
|
Wolfe’s law:
|
If loading on a particular bone increases, the bone will remodel itself over time to become stronger to resist that sort of loading, if the loading on a bone decreases, the bone will become weaker due to turnover
|
|
|
How does articular cartilage develop?
|
Thick cartilage mass at the articular side of the epiphysis acts as a type of growth plate with simultaneous growth, remodeling, and ossification take place that results in a thinner layer of articular cartilage
|
|
|
What does disturbance of endochondral ossification result in?
|
irregularities in thickness of epiphyseal cartilage, creating areas of weakness
|
|
|
What exacerbates weakened areas in epiphyseal cartilage?
|
Regression of or occlusion of cartilage vascular canals preventing nutritional supply to deeper layers of the retained cartilage that are too deep to receive nourishment from the synovial fluid
|
|
|
When do cartilage vascular canals regress?
|
By 7 months of age
|
|
|
What leads to the formation of fissues or cartilage flaps?
|
Biomechanical shearing forces on the weakened areas of the epiphyseal cartilage
|
|
|
What is a manifestation of compressive biomechanical forces on weakened areas of epiphyseal cartilage?
|
Infolding of cartilage to form subchondral bone cyst
|
|
|
Most common OC of the tarsocural joint:
|
DIRT (1st), distal lateral trochlear ridge (2nd), medial malleolus of tibia (3rd)
|
|
|
Most common OC of FP joint:
|
lateral trochlear ridge of the femur (1st) other: medial trochlea of femur, trochlear groove, distal end of patella
|
|
|
Most common OC of MFT joint:
|
subchondral cyst of medial femoral condyle
|
|
|
Most common OC in fetlock:
|
dorsal end of sagittal ridge of MC/MT3
|
|
|
How does cartilage repair differ from bone repair?
|
Bone can remodel throughout life but cartilage metabolism ceases early in juvenile period
|
|
|
What is the consequence of cessation of cartilage metabolism?
|
There is no capacity for substantial remodeling or repair and lesions that manifest late or are large are not repaired
|
|
|
What is osteochondrosis?
|
Disturbance of endochondral ossification linked with rapidly changing metabolisc status of articular cartilage in juveniles
|
|
|
What etiologic factors are associated with OC?
|
Biomechanical influences, exercise, failure of vascularization, nutritional imbalances, and genetics
|
|
|
What nutritional factors may contribute to OC?
|
Low copper levels (either low Cu intake or antagonism by Zn or cadmium), high P inducing a 2ndary hyperPTH, increased easily digestable CHO leading to increased insulin & IGF-1
|
|
|
What effect does insulin & IGF-1 have on endochondral ossification?
|
Mitogens for chondrocytes, stimulate chondrocyte survival & suppress apoptosis, decreases T3 & T4 which are involved in final chondrocyte differentiation and in metaphyseal blood vessel invasion of cartilage
|
|
|
How does growth rate related to OC?
|
Rapid growth rate correlated with increased OC but could be from high plane of nutrition or genetic influences
|
|
|
Radiographic characteristics of SCL:
|
radiolucent area with a thin well demarcated sclerotic rim
|
|
|
Where are SCL usually located?
|
SCB underlying articular cartilage in weight bearing area of joint or less commonly in metaphysis close to the growth plate
|
|
|
How are OC and SCL different?
|
OC lesions are usually at transition from weight bearing to not weight bearing articular surface and SCL are at weight bearing surfaces
|
|
|
What are the theories of SCL development?
|
Hydraulic, inflammatory
|
|
|
What is the hydraulic theory?
|
Primary cartilage damage followed by intrusion of synovial fluid, which put mechanical pressure on SCB during weight bearing and resulted in necrosis
|
|
|
What is the inflammatory theory?
|
Fibrous tissue & cystic fluid from SCL have increased proinflammatory mediators and cytokines such as PGE2, IL-1, IL-6
|
|
|
Most common location of SCL:
|
medial femoral condyle of femur (1st) phalanges (2nd)
|
|
|
What is the source of lameness with SCL?
|
Intracystic or intraosseous pressure
|
|
|
How often do SCL communicate with the joint?
|
Approximately 30%
|
|
|
What is tissue inside the SCL composed of?
|
Dense fibrous tissue, myxomatous tissue, with necrotic bone, calcified or mineralized areas, sometimes fibrocartilage
|
|
|
What is the lining of the SCL composed of?
|
Elongated fibroblasts parallel to collagen bundles, macrophages, PMN cells
|
|
|
SCL radiographic grades:
|
grade 1: lesion less than 10mm, dome shaped; grade 2a: lesion more than 10mm in depth with narrow cloaca; grade 2b: lesion more than 10mm in depth with wide cloaca; grade 3: condylar flattening or small defect in SCB; grade 4: lucency in condyle with no radiographic evidence cloaca
|
|
|
Non-surgical management of SCL:
|
rest, NSAIDs, vitamin supplementation, anabolic drugs
|
|
|
Surgical approaches to SCL:
|
arthroscopic, transosseous
|
|
|
Surgical treatments for SCL:
|
curettage & debridement, intralesional corticosteroid injection, grafting
|
|
|
How is surgical curettage & debridement performed?
|
Arthroscopic- remove overlying cartilage then curet; transosseous- drill into cyst first with 2.5mm pilot hole then 5.5 drill then curet
|
|
|
What is success of surgical curettage & debridement related to?
|
Better in younger horses (< 3 years) and better with less than 15mm of surface defect
|
|
|
What is success of intralesional corticosteroid injection related to?
|
Better for unilateral lesions than bilateral
|
|
|
What are the different grafting options?
|
Cancellous bone graft, mosaic arthroplasty, tricalcium phosphate granules (TPC), hydrogels +/- parathormone, autogenous fibrin plugs +/- allogenic chondrocytes or IGF-1, BMC + PrP +TCP
|
|
|
What are the best graft donor sites for the medial femoral condyle?
|
Trochlear groove and axial lateral trochlear ridge of the femur
|
|
|
What are the best graft donor sites for the lateral femoral condyle?
|
Trochlear groove, axial aspect of the medial femoral condyle
|
|
|
What has been used clinically as a donor site for MFC SCL mosaic arthroplasty?
|
Abaxial border of medial femoral trochlea of unaffected limb
|

