![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
82 Cards in this Set
- Front
- Back

|
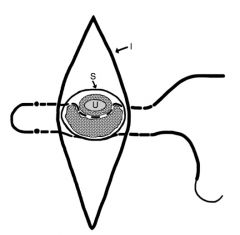
bladder eversion
|
|

|
|
|

|
bladder eversion
|
|
|
suture during penectomy to secure penile stump to skin and crush CCP
|
|

|
|
|

|
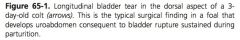
Ruptured bladder
|
|
|
Relation of bladder to peritoneum:
|
apex of bladder is covered with peritoneum but the remainder is retroperitoneal
|
|
|
Muscle layers of the bladder:
|
outer longitudinal and oblique layer, inner transverse and circular layer which becomes external to the outer layer dorsally
|
|
|
Innervation of the bladder:
|
sympathetic, parasympathetic, cholinergic, somatic
|
|
|
Sympathetic innervation of the bladder:
|
hypogastric nerve with preganglionic fibers from spinal segments L1 to L4 in the caudal mesenteric ganglion and post-ganglionic beta 2 receptors (bladder) or alpha 1 and 2 (urethra)
|
|
|
Parasympathetic innervation of the bladder:
|
sacral spinal segments forming pelvic nerve
|
|
|
Somatic innervation of the bladder:
|
pudendal nerve branch innervation of the urethralis muscle sphincter
|
|
|
Innervation of the detrusor muscle:
|
parasympathetic pelvic nerve and beta 2 sympathetic post-ganglionic fibers
|
|
|
Dominant nerve activity during filling or storage of the bladder:
|
sympathetic (stimulation of beta 2 sympathetic receptors, inhibition of parasympathetic pelvic nerve)
|
|
|
Most common signalment for uroperitoneum in the foal:
|
colt shortly after birth
|
|
|
Most common size and location of bladder tears:
|
2-5 cm in length on dorsal surface
|
|
|
Clinical pathology association with uroperitoneum:
|
hyponatremia, hypochloremia, hyperkalemia, azotemia
|
|
|
Diagnosis of uroperitoneum:
|
serum to peritoneal fluid creatine ratio greater than 2, free fluid in abdomen on ultrasound
|
|
|
Stabilization prior to surgery for uroperitoneum:
|
address hyperkalemia to prevent cardiac arrhythmias, decrease abdominal distension by draining urine
|
|
|
How is hyperkalemia addressed with uroperitoneum?
|
Administration of Ca gluconate followed by non-K containing fluid (0.9% saline) with dextrose
|
|
|
Effects of Ca and dextrose treatment on uroperitoneum:
|
Ca antagonized K, dextrose causes release of insulin which increase Na/K ATPase pump to move K intracellular
|
|
|
Cardiac affects of hyperkalemia:
|
ventricular fibrillation, cardiac arrest, 3rd degree AV block, premature ventricular beat
|
|
|
Risk of rapid drainage of urine form abdomen:
|
hemodynamic collapse
|
|
|
How is hemodynamic collapse prevented when draining uroabdomen?
|
Concurrent administration of non-K containing IVF
|
|
|
Medical management of uroperitoneum:
|
indwelling bladder catheter, correction of lyte abnormalities
|
|
|
Indications for medical management of uroperitoneum:
|
foals with small tears, adults in which distinct tear can not be identified
|
|
|
Medical management of patent urachus:
|
dip navel with chlorhexadine solution 2-4 times a day, broad spectrum antibiotics
|
|
|
Why is iodine not indicated for management of patent urachus?
|
Has been associated with rapid dissication and irritation of tissues and development of acquired patent urachus
|
|
|
When is surgical management of patent urachus indicated?
|
No response to medical management in 5-7 days, ultrasound reveals multiple abnormalities of the umbilicus
|
|
|
Composition of uroliths:
|
predominately calcium carbonate, type 2 contain phosphate as well
|
|
|
Types of uroliths:
|
1: yellow-green speculated easily fragmented 2: gray-white smooth resistant to fragmentation
|
|
|
What is struvite?
|
MgNH3PO4
|
|
|
Surgical approach to urolithiasis:
|
cystotomy through ventral midline, parainguinal, laparoscopic, pararectal, perineal urethrostomy approaches or lithotripsy
|
|
|
Medical management of urolithiasis:
|
dietary changes (avoid legumes, avoid Ca containing feeds or supplements)
|
|
|
What is sabulous urolithiasis?
|
Accumulation of large amount of urine sediment secondary to bladder paralysis
|
|
|
How do clinical signs of sabulous urolithiasis differ from urolithiasis?
|
In sabulous urolithiasis the bladder is usually distended and the sabulous mass can be indented on rectal palpation after the bladder is drained
|
|
|
Types of bladder displacement:
|
extrusion (eventration) through a tear in the vagina or eversion (prolapse)
|
|
|
Cause of bladder extrusion:
|
perineal lacerations
|
|
|
Cause of bladder eversion:
|
excessive straining
|
|
|
Treatment of bladder displacement:
|
surgical resection of affected portion of bladder
|
|
|
Most common bladder neoplasia:
|
squamous cell carcinoma
|
|
|
Indications for cystorrhaphy:
|
bladder disruption (tear, rupture)
|
|
|
Approach to cystorrhaphy in foal:
|
oversew umbilicus, fusiform incision around umbilicus
|
|
|
Approach to cystorrhaphy in adult:
|
mare: caudal midline incision from 2-3 cm cranial to umbilicus for 15-18 cm, prolapse bladder through vaginal incision, urethrotomy or spincterotomy; male: starts 2-3 cm cranial to umbilicus then directed 2-4 cm paramedian at the prepuce
|
|
|
Describe cystorrhaphy:
|
bladder exposed by maintaining traction on urachus, inspect urachus for tears, identify bladder tear, excise wound margins, close tear in 2 layers (either continuous oversewn with inverting or double inverting) with absorbable suture that does not penetrate the mucosa, resect urachus
|
|
|
When is cystoplasty indicated?
|
Patent or persistent urachus or option in foal with bladder or urachal tear
|
|
|
Describe cystoplasty:
|
oversew umbilicus, elliptical incision around umbilicus, umbilicus and urachus dissected free of body wall, umbilical vein double ligated and resected as far cranially as needed to removal all diseased vein, bladder exposed with traction on urachus, stay sutues placed in ventrolateral bladder, umbilical arteries double ligated and resected at the level of the urachal resection, clamp placed across urachus, transverse incision made across apex of bladder, traction applied to stay sutures, bladder closed in 2 layers with absorbable suture without penetration of bladder mucosa
|
|
|
Indications for cystotomy:
|
urolithiasis
|
|
|
What should be avoided with ventral approach to bladder in adult males?
|
Transection of superficial caudal epigastric and external pudendal during approach
|
|
|
Describe cystotomy:
|
bladder exteriorized through incision, isolated from abdomen with gauze packing, incision made in ventral bladder over urolith, cystotomy closed in 2 layers
|
|
|
Which layer of the abdominal closure is more critical in males?
|
External rectus
|
|
|
Benefits of parainguinal approach to cystotomy:
|
eliminates reflection of prepuce and penis, eliminates encountering large vessels during ventral/ parapreputial approach
|
|
|
Indications for laparoscopic approach to bladder:
|
cystorrhexis, persistent urachus, umbilical infection, urolithiasis
|
|
|
Complications of laparoscopic approach to bladder:
|
hemorrhage, obstructed visualization by falciform fat, need to be proficient with intra/ extracorporeal suturing or laparoscopic suturing devices
|
|
|
What is lithotripsy?
|
Fragmentation of urinary calculus with pulse dye laser (504nm) or Ho:YAG laser (2100nm)
|
|
|
How does the pulse dye laser cause fragmentation?
|
Generation of acoustic wave that is greater than the tensile strength of the urolith
|
|
|
How does the Ho:YAG laser cause fragmentation?
|
Photothermal and photoacoustic waves
|
|
|
Disadvantages of lithotripsy:
|
availability of laser, long surgery times, may not fragment urolith
|
|
|
Complications of bladder surgery:
|
ventricular arrhythmia with hyperkalemia in uroperitoneum, chemical peritonitis, adhesion formation in foals, incisional infection
|
|
|
Location of urolith obstruction in steers and bulls:
|
usually distal sigmoid flexure
|
|
|
Location of urolith obstruction in swine:
|
usually sigmoid flexure or distal penile urethra
|
|
|
Location of urolith obstruction in small ruminants:
|
urethral process and distal sigmoid flexure
|
|
|
What is performed prior surgical intervention for urolithiasis in ruminants?
|
Cystocentesis or percutaneous placement of foley catheter in bladder to empty bladder
|
|
|
Advantages of ruminant cystocentesis:
|
improved patient comfort, reduced risk of rupture
|
|
|
Disadvantages of ruminant cystocentesis:
|
uroperitoneum from leakage from cytocentesis site
|
|
|
Disadvantages of percutaneous placement of foley catheter in bladder?
|
Peritonitis, adhesion formation
|
|
|
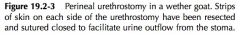
Surgical treatment options for ruminant urolithiasis:
|
urethral process amputation, urohydropulson, penectomy, PU, ischial urethrostomy, ischial urethrotomy, cystotomy, tube cystotomy, bladder marsupialization
|
|
|
Complications of urohydropulsion:
|
difficulty in catheter passage, traumatic urethritis, urethral rupture
|
|
|
Describe penectomy:
|
distal perineal incision made, penis dissected free, amputated after vessel ligature, CCP closured with a horizontal mattress suture that fixes the penile stump to the skin, urethra incised longitudinally and sutured to adjacent skin, tubing introduced into urethra and left in place 3-5 days to compress CSP
|
|
|
Disadvantage of PU:
|
stricture of stoma
|
|
|
Indication for ischial urethrotomy:
|
removal of calculi then reapposition of urethral mucosa to maintain breeding function
|
|
|
Treatment of uretheral uroliths:
|
PU, urethral hydropulsion
|
|
|
How is urethrorrhexis diagnosed?
|
Retrograde infusion of sterile saline to identify communication or urethra with wound, endoscopic examination, ultrasound +/- saline infusion, retrograde contrast radiography
|
|
|
Treatment of urethrorrhexis:
|
prevention of further tissue damage by diverting urine flow through a catheter
|
|
|
Most common location of urethral rents:
|
proximal at level of ischial arch
|
|
|
Treatment of urethral rent:
|
subischial PU without penetration of urethral mucosa, just through tunica albuginea of CSP
|
|
|
Describe temporary PU:
|
6-8 cm incision on midline 4-6 cm ventral to anus just distal to ischial arch, SQ tissues divided, retractor penis muscles divided, bulbospongiousus muscles divides, urethra exposed, longitudinal incision made in caudal urethra
|
|
|
Describe permanent PU:
|
perform as for temporary PU, suture penile muscles on cut edge in continuous pattern with absorbable suture, apposed urethral mucosa to skin with interrupted sutures without excessive tension on urethra
|
|
|
When is a distal urethrotomy performed?
|
Remove distal obstructions in approach similar to PU
|
|
|
Closure of distal urethrotomy:
|
accurate reconstruction of CSP and bulbospongiosus to present urine leakage, apposition of retractor penis muscle for security
|
|
|
How is urethral stricture minimized after urethra surgery?
|
Minimize duration of catheterization, accurate tissue repair, effective hemostasis, adequate drainage of perineal tissues
|
|
|
Complications of urethral surgery:
|
partial dehiscence of urethrostomy, stricture
|

