![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
192 Cards in this Set
- Front
- Back

|
Elastrator
|
|

|
|
|

|
|
|
|
inguinal hernia
|
|

|
inguinal rupture
|
|
|
|
|
|
ruptured inguinal hernia
|
|

|
|
|
|
|
|
|
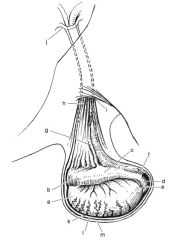
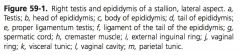
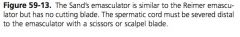
Components of the male reproductive anatomy:
|
scrotum, testis, epididymis, inguinal canal, tunics, gubernaculum, and spermatic cord
|
|
|
What is the tunica dartos?
|
muscle that relaxes with heat and contracts with cold to held regulate testicular temperature and change the size of the scrotum, in the median plane of the tunica dartos divides the scrotum into left and right halves
|
|
|
Scrotal arterial supply:
|
external pudendal artery
|
|
|
Nervous supply to scrotum:
|
genitofemoral nerve
|
|
|
How do the left and right testes differ?
|
left is usually larger and more caudal than the right
|
|
|
What is the tunica albuginea?
|
inelastic capsule over the testis, which forms septa of connective tissue to divide the testis into lobules
|
|
|
What is contained in each testicular lobule?
|
seminiferous tubules, sertoli cells, and interstitial cells
|
|
|
What lines seminiferous tubules?
|
spermatogonia attached to a basement membrane. As the spermatogonia mature they are pushed toward the lumen to emerge as spermatozoa
|
|
|
What stimulate emergence of spermatozoa from the seminiferous tubule?
|
FSH
|
|
|
Function of sertoli cells:
|
provide mechanical and nutrition support to the developing spermatozoa
|
|
|
Function of interstitial cells:
|
produce androgens and estrogens
|
|
|
Alterntive name for interstitial cells:
|
leydig cells
|
|
|
Regions of the epididymis:
|
head, body and tail
|
|
|
Where is the head of the epididymis?
|
cranial pole of the testis
|
|
|
What is the head of the epididymis composed of?
|
efferent ductules of the testis unite to form a single coiled tube, which are the body and tail of the epididymis
|
|
|
Where is the body of the epididymis?
|
dorsolateral surface of the testis
|
|
|
Where is the tail of the epididymis?
|
projects beyond the caudal border of the testis, wraps medially
|
|
|
What is the continuation of the epididymis?
|
ductus deferens
|
|
|
Function of the epididymis:
|
receives immature sperm and with ejaculation, peristaltic motion force sperm from the epididymis to the ductus deferens
|
|
|
What is in the inguinal canal?
|
spermatic cord, genitofemoral nerve, external pudendal vasculature, and efferent lymphatics pass through the canal
|
|
|
What are the borders of deep inguinal ring?
|
caudal edge of the IAO is the cranial border, the rectus abdominus and prepubic tendon (prepubic tendon is the tendon of insertion of the rectus abdominus) are the ventral and medial border and the inguinal ligament is the caudal border
|
|
|
What is the external opening of inguinal canal?
|
superficial inguinal ring is slit in the external abdominal oblique muscle
|
|
|
How are the deep and superficial inguinal rings aligned?
|
medial are aligned but the lateral borders are divergent making the medial aspect of the canal shorter than the lateral aspect
|
|
|
What is the tunica vaginalis?
|
extension of the peritoneum, and has a visceral and parietal surface
|
|
|
What is the vaginal process?
|
Sac formed of the visceral surface adhered to the tunica albuginea and the parietal surface is continuous with the parietal periton
|
|
|
What is the vaginal ring?
|
ring that forms as the peritoneum invaginates into the canal through the deep inguinal ring
|
|
|
What is the gubernaculum?
|
fetal cord that extends from the fetal testis to the scrotum and guides decent into the scrotum
|
|
|
When do the fetal gonads arise during gestation?
|
Day 40
|
|
|
What and when does the vaginal process form during gestation?
|
gubernaculum extends from the caudal pole of the testis and ends in an expansion between the internal and external abdominal oblique muscles, with peritoneal lining penetrating this area around day 45 of gestation
|
|
|
What begins at 5 months of gestation?
|
testicle hypertrophies under the influence of the leydig cells, the cephalic (suspensory) ligament atrophies, and the epididymis begins decent into the vaginal process
|
|
|
What occrurs at 8.5 months of gestation?
|
gubernaculum begins to shorten and the testicle shrinks in size due to loss of leydig cells. The epididymis and subperitoneal gubernaculum dilate the vaginal ring and inguinal canal
|
|
|
When does the testicle passes into the inguinal canal?
|
around 270-300 days of gestation
|
|
|
When does the testicle descend into the scrotum?
|
Within a few days of birth
|
|
|
When does the vaginal ring contract?
|
within a few weeks of life
|
|
|
What are the parts of fetal gubernaculum?
|
Cranial, middle, caudal
|
|
|
Where is the cranial portion of the gubernaculum?
|
between the testis and the epididymis
|
|
|
What does the cranial portion of the gubernaculum become?
|
proper ligament of the testis.
|
|
|
Where is the middle portion of the gubernaculum?
|
between the epididymis and the point of entry of the gubernaculum at the inguinal ring
|
|
|
What does the middle portion of the gubernaculum become?
|
ligament of the tail of the epididymis
|
|
|
Function of the ligament of the tail of the epididymis?
|
connects the tail of the epididymis to the parietal tunic
|
|
|
Where is the caudal portion of the gubernaculum?
|
extends from the abdominal wall to the scrotum
|
|
|
What does the caudal portion of the gubernaculum become?
|
scrotal ligament,
|
|
|
Function of the scrotal ligament?
|
connecting the parietal tunic to the scrotum
|
|
|
What is the scrotal ligament called in a cryptorchid?
|
inguinal extension of the gubernaculum testis
|
|
|
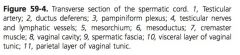
Components of the spermatic cord:
|
tunica vaginalis, vessels, nerves, and lymphatics, and the ductus deferens
|
|
|
Function of the cremaster?
|
contracts to retract the testicle
|
|
|
Arterial supply to the cremaster?
|
cremasteric artery
|
|
|
What is the mesorchium?
|
fold of the parietal tunic enclosing the neurovascular portions of the cord
|
|
|
What is the mesoductus ?
|
fold of the parietal tunic enclosing the ductus deferens
|
|
|
What is the mesofuniculum?
|
thin portion of the mesorchium between the mesoductus and the parital tunic
|
|
|
Arterial supply to the ductus deferens:
|
deferential branch of the umbilical artery
|
|
|
What are the branches of ehe testicular artery?
|
epididymal artery
|
|
|
Arterial supply to the testicle?
|
Testicular artery, epidydmal artery cremasteric artery, deferential artery
|
|
|
What is the panpiniform plexus?
|
Tortuous portions of the testicular artery and vein in the cord
|
|
|
Where does the testicular artery empty?
|
right testicular vein drains to the caudal vena cava and the left testicular vein drains to the left renal vein
|
|
|
Monorchidism:
|
complete absence of 1 testicle as a result of testicular degeneration
|
|
|
When can testicular degeneration occur to produce monarchism?
|
prior to birth or in an abdominally retained testis after birth from a vascular insult, such as spermatic cord torsion
|
|
|
How is monorchidism confirmed?
|
with hCG stimulation test after the contralateral testicle has been removed
|
|
|
Complete abdominal cryptorchid:
|
both the testis and epididymis retained in the abdomen
|
|
|
Partial abdominal cryptorchid:
|
retained abdominal testicle but the epididymis is within the inguinal canal
|
|
|
Inguinal cryptorchid:
|
both the testicle and epididymis within the inguinal canal
|
|
|
Why is the retained testicle infertile?
|
cannot produce sperm because of rudimentary development of the seminiferous tubules due to high temperature exposure but the leydig cells are capable of producing hormones
|
|
|
Mechanisms of cryptorchidism:
|
failure of the subperitoneal portion of the gubernaculum to enlarge the vaginal ring, failure of the subperitoneal portion to regress after enlargement of the vaginal ring, or failure of the testicle to regress to a size that can traverse the vaginal ring prior to ring constriction after birth
|
|
|
What is the side predilection for cryptorchism?
|
More left cryptorchids are abdominally retained than right, which may reflect natural testicular size. The smaller right testicle may be capable of traversing the vaginal ring and become retained in the inguinal canal while the larger left testicle fails to traverse the vaginal ring and becomes retained abdominally
|
|
|
How are retained testicles diagnosed?
|
testosterone concentration, hCG stimulation and testosterone concentration, and conjugated estrogen concentration
|
|
|
How does testosterone distinguish cryptorchis?
|
Intact stallions and cryptorchids have significantly higher concentrations of testosterone than geldings. Geldings tend to have testosterone values less than 40 pg/mL
|
|
|
When is Testosterone concentration less accurate?
|
horses less than 3 years old and in the winter
|
|
|
How does Concentration of testosterone after hCG distinguish cryptorchids?
|
should rise within 30 to 120 minutes (or longer) after administration IV of 6-12,000 units of hCG to horses with testicular tissues. Geldings had less than 40 pg/mL testosterone before and after stimulation while cryptorchid horses had values greater than 100pg/dL before and after stimulation
|
|
|
When is hCG stimulation less accurate?
|
horses less than 18 months and in the winter
|
|
|
What is the most accurate at distinguishing geldings from cryptorchids?
|
Conjugated estrogen
|
|
|
When is conjugated estrogen less accurate?
|
horses less than 3 years, donkeys
|
|
|
How does estrogen concentration distinguish cryptorchids?
|
less than 50pg/mL were classified as geldings and concentrations greater than 400pg/mL were cryptorchid
|
|
|
When does Inguinal herniation occur?
|
portion of the intestine travels through the vaginal ring and into the vaginal canal
|
|
|
What is a scrotal hernia?
|
intestine travels through the canal and into the scrotum
|
|
|
What is a ruptured inguinal hernia?
|
parietal tunic is ruptured
|
|
|
What is an inguinal rupture?
|
rent occurs in the peritoneum, allowing intestine to pass outside of the tunic into the scrotum
|
|
|
What is a direct hernia?
|
Intestine is outside of the vaginal tunic
|
|
|
What is a indirect hernia?
|
Intestine stays confined within the vaginal cavity
|
|
|
How are Congenital hernias treated?
|
Unless there is an inguinal rupture or a ruptured hernia, hernia should be reduced manually or a truss can be applied and worn for a week at a time
|
|
|
How is a inguinal hernia truss constructed?
|
rolled cotton packed into the superficial inguinal ring and held in place with elastic gauze, secured with a tape wrap in a figure 8 pattern over the hind quarters
|
|
|
Approaches to surgical congenital hernia repair:
|
open approach or laparoscopic
|
|
|
Describe open approach for congenital hernia repair:
|
incision is made over the superficial inguinal ring, vaginal sac isolated, and the scrotal ligament is transected. The intestine is reduced back to the abdomen, which can be facilitated by twisting the spermatic cord. After reduction, the spermatic cord is ligated and transected proximal to the superficial ring. For added security, the superficial inguinal ring can be sutured closed
|
|
|
When is laparoscopy chosen for congenital inguinal hernias?
|
non-strangulating hernias
|
|
|
Describe laparoscopic congenital hernia repair:
|
dorsal recumbency, intestine is guided back into the abdominal cavity as is the testicle. The testicle is ligated and transected intra-abdominally. The deep inguinal ring and vaginal ring are closed with laparoscopic staples or suturing
|
|
|
Advantages of Laparoscopy for congenital hernia repair?
|
quicker, has less post-operative swelling, and the foal has a shorter convalescence time
|
|
|
Predilictions for Acquired inguinal hernias?
|
more likely after exercise or breeding and there are breed predilications in standardbreds, drafts, and andalusians
|
|
|
Complications of acquired inguinal hernias?
|
Strangulation of the intestine by the vaginal ring can cause ischemic injury to the bowel, strangulation or obstruction of the spermatic vasculature causes ischemic injury to the testicle
|
|
|
Treatment options for acquired inguinal hernias:
|
If detected early, an attempt can be made to manually reduce the hernia with either external manipulation or manipulation per rectum. If there is question of strangulation or the hernia cannot be reduced manually, correction is approached in dorsal recumbency with either a single incision over the inguinal ring or a combined approach with an incision over the inguinal ring and a ventral celiotomy incision (midline, paramedian, parainguinal)
|
|
|
How is reherniation prevented with acquired inguinal hernias?
|
If the testicle is removed, reherniation is prevented by ligation of the spermatic cord as proximal as possible, closure of the superficial inguinal ring, or gauze packing of the inguinal canal for 24-48 hours. If the testicle is not removed, reherniation is prevented by suturing the superficial inguinal ring around the spermatic cord, or in a second procedure to laparoscopically cover the deep inguinal ring or vaginal ring
|
|
|
What are the laparoscopic options for reventing reherniation in a stallion without the testicle removed?
|
placement of a mesh beneath the peritoneum and over the deep inguinal ring, creation of a peritoneal flap which is sutured or stapled over the ring, or placing a coil within the inguinal canal.
|
|
|
What is Torsion of the spermatic cord?
|
cord rotates on its vertical axis, usually within the vaginal process
|
|
|
Predisposition for torsion of the spermatic cord?
|
abnormally long ligament of the tail of the epididymis or proper ligament of the testis
|
|
|
What is Rotation the spermatic cord of 180 degrees associated with?
|
may be an incidental finding and cause no clinical signs of pain, but may be associated with subpar testicular function
|
|
|
What is rotation of the spermatic cord of 360 degrees or greater associated with?
|
pain and enlargement of the testicle and cord
|
|
|
How is clinical torsion of the spermatic cord treated?
|
removal of the affected testicle
|
|
|
What can be done to prevent torsion of the spermatic cord?
|
In cases in which the rotation was thought to have occurred because of abnormally long testicular ligaments, the contralateral testicle can be fixed in position (orchidopexy or orchiopexy) by placing non-absorbable suture through the tunica albuginea and tunica dartos at the cranial and caudal pole of the testis
|
|
|
What is a hydrocele (vaginocele)?
|
abnormal collection of normal fluid in the vaginal cavity because egress of fluid through the lymphatics and veins is slower than production, or because of excess peritoneal fluid which enters the vaginal cavity
|
|
|
When do hydroceles develop?
|
in association with testicular neoplasia, 180 degree torsion of the spermatic cord, trauma, parasitic migration, hot weather, or with open castration, especially in mules
|
|
|
Treatment of hydrocele?
|
removal of the affected testicle prior to temperature induced dysfunction affecting the contralateral testicle, sac dissected free from fascia, scrotal ligament transected and sac is removed in geldings or no treatment is needed if the hydrocele is not enlarging, and does bother the horse or the owner
|
|
|
What is a hemetocele?
|
blood within the vaginal cavity rather than normal fluid
|
|
|
When does hematocele occur?
|
testicular trauma or an extension of hemoabdomen
|
|
|
Treatment of hematocele?
|
blood should be lavaged from the vaginal cavity to prevent thermal-induced testicular dysfunction. If the integrity of the tunica albuginea is unknown, the testicle should be surgically explored. If the tunica albuginea is ruptured, it should be sutured or the testicle should be removed
|
|
|
What is Rupture of the tunica albuginea associated with?
|
breach of the blood-testicle barrier and exposure to spermatozoa in the parenchyma of the testicle can cause an immunologic reaction
|
|
|
What is a varicocele?
|
abnormal enlargement of the panpiniform plexus because of valvular incompetence at the level of the caudal vena cava or renal vein causes reflux of blood into the plexus
|
|
|
What does varicocele cause?
|
alters the counter-current heat exchange between the plexus and the testicular artery which may induce testicular dysfunction
|
|
|
Treatment for varicocele?
|
removal of the testicle and cord if there is testicular dysfunction
|
|
|
Treatment for Retraction of the testicle into the inguinal canal?
|
cremaster muscle can be transected with an approach over the long axis of the spermatic cord. A 3cm section of the cremaster is resected and fascia and skin are closed after resection
|
|
|
Germinal cell testicular tumors:
|
seminomas, teratomas, teratocarcinoma, and embryonic carcinomas
|
|
|
Non-germinal testicular cell tumors:
|
sertoli cell tumors and leydig cell tumors
|
|
|
Most common testicular tumors?
|
Seminomas are most common, then teratomas
|
|
|
Origin of seminomas?
|
arise from seminiferous tubules
|
|
|
Origin of Teratomas?
|
arise from multiple tissues of different embryologic origin
|
|
|
Origin of Teratocarcinoma?
|
mixture of neoplastic differentiated tissue and undifferentiated embryonic tissues
|
|
|
Origin of embryonic carcinomas?
|
only neoplastic undifferentiated embryonic tissue
|
|
|
What defines sexual identity?
|
genetic makeup, gonads, and morphology of accessory genitals
|
|
|
What is an intersex?
|
Differs in 1 of the definitions of sexual identity
|
|
|
What is a true hermaphrodite?
|
has both ovarian and testicular tissue. Gonads can be either 1 of each or may consist of both testicular and ovarian tissue (ovoteste). External genitalia usually trends toward one sex but does represent both sexes
|
|
|
What are pseudohermaphrodites?
|
have the gonads of only 1 sex but the external genitalia of the other sex
|
|
|
What form of pseudohermaphrodite is most common?
|
Male, with hypoplastic abdominally retained testicles and a rudimentary penis which resembles a clitoris
|
|
|
only method of direct assessment of stages of spermatogenesis:
|
Testicular needle biopsy
|
|
|
how is testicular needle biopsy performed?
|
under sedation and local anesthesia with a vim-silverman needle or a automated biopsy needle
|
|
|
most ideal ideal location of needle biopsy?
|
craniolateral quarter of the testis, where there is less vasculature and is away from the head of the epididymis
|
|
|
Castration Incisional approaches:
|
scrotal, inguinal, per primam, or laparoscopic
|
|
|
Options for scrotal castratio incision:
|
single incision, 2 incisions on either side of the raphe, or removing the bottom portion of the scrotum
|
|
|
Surgical castration options:
|
open, closed, and half-closed
|
|
|
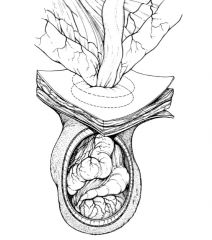
What is Open castration technique?
|
parietal tunic is incised and the tail of the epididymis and the fold of the mesorchium is transected to exteriorize the testis, epididymis, and distal spermatic cord
|
|
|
What is closed castration technique?
|
fascia is stripped off of the parietal tunic to expose the testicle and distal cord within the tunic
|
|
|
What is half-closed castration technique?
|
small incision is made in the parietal tunic and the contents are prolapsed from the incision in the tunic
|
|
|
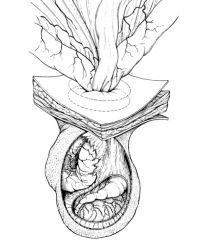
Equipment for emasculation:
|
white’s, reimer, serra, sand’s, or the Henderson equine castrating instrument
|
|
|
Benefit of Half-closed and closed castration:
|
decreasing post-operative complication because the parietal tunic is removed and half-closed allows inspection of the tunic contents
|
|
|
Disadvantages of Half-closed and closed castration?
|
require more dissection so may take longer and may not be advantageous in standing castration
|
|
|
What reduces risk of evisceration?
|
ligature is placed proximally on the spermatic cord prior to transection
|
|
|
Benefits of leaving castration incision open?
|
improves drainage
|
|
|
Benefits of Primary closure of the incision with castration?
|
speeds recovery and healing, decreases pain and edema, and is beneficial when post-operative exercise can not be enforced
|
|
|
Disadvantages of primary closure of incision with castration?
|
need for meticulous hemostasis, adherence to aspectic technique, and time required for closure
|
|
|
When does Testorsterone level fall after castration?
|
within 2 days
|
|
|
Describe Per primam castrastion:
|
dorsal recumbency, incision is made over the superficial inguinal ring after pushing the testicle from the scrotum over the ring. The parietal tunic is incised longitudinally. Within the tunic, the tail of the epididymis is identified and used to evert the testicle from the vaginal cavity. Ligatures are applied proximally on the cord prior to transection. The parietal tunic is closed prior to closure of the primary incision
|
|
|
Benefit of per primam castration?
|
In horses older than 2 years to decrease the likelihood of evisceration
|
|
|
Describe Laparoscopic castration:
|
Using either electrosurgery equipment in combination with ligatures or a ligasure, the testicular vessels and ductus deferens are occluded. Both testicles can be approached from 1 side. Post-operatively, the testicle initially swell with loss of blood supply but eventually atrophy
|
|
|
When do testosterone levels fall after laparoscopic castration?
|
within 7 days
|
|
|
Complication of laparoscopic castration:
|
alternative blood supply to the testicle (cremasteric artery, external pudendal artery) are sufficient to allow persistent hormonal production and stallion-like behavior
|
|
|
Describe Vasectomy:
|
dorsal recumbency, longitudinal incision is made over the testis and the ductus deferens is identified. 3 ligatures are placed on the ductus and a 2-3 cm portion is removed between the 2 proximal ligatures and a distal ligature. The process is repeated for the opposite ductus deferens through the same incision. The tunic is closed prior to skin closure
|
|
|
Cryptorchid Standing approaches:
|
flank and laparoscopic
|
|
|
Cryptorchid Recumbent approaches:
|
inguinal, parainguinal, suprapubic paramedian, flank and laparoscopic
|
|
|
non-invasive cryptorchid castration:
|
Inguinal, parainguinal and laparoscopic
|
|
|
invasive cyrptorchid approaches:
|
suprapubic paramedian and flank
|
|
|
indications Flank and suprapubic paramedian cyrptorchid castration:
|
only used for abdominally retained testicles
|
|
|
describe inguinal cryptorchid castration:
|
incision is made over the superficial inguinal ring. Fascia is digitally transected to expose the inguinal canal. If the testicle is in the inguinal canal it can be exposed. The vaginal sac should be opened to ensure that all structures are being removed. If the testicle is abdominal, the vaginal process must be located. The vaginal process is usually inverted in the abdomen with a complete abdominal cryptorchid but may be in the inguinal canal if the epididymis is retained in the inguinal canal. Once the vaginal process has been exteriorized, a small incision is made and the epididymis is grasped and retracted to evert the testicle. Once exteriorized, the testicle and cord are emasculated or ligated and transected.
|
|
|
how can the inverted vaginal process be identified in cryptorchid castration?
|
locating the inguinal extension of the gubernaculum testis, traction can be placed on it, following to the vaginal process. Another option is passing a finger into the inguinal ring, placing it into the vaginal process, then guiding sponge forceps into the ring to grasp and retract the vaginal process
|
|
|
where is the IEGT located?
|
usually at the medial or lateral aspect of the cranial to mid-portion of the ring
|
|
|
what should the IEGT be distinguished from?
|
genitofemoral nerve, which usually runs in the mid- to caudal third of the ring
|
|
|
how is risk of evisceration decreased with inguinal cryptorchid castration?
|
superficial inguinal ring should be closed or the inguinal canal is packed with gauze that is maintained for 24-36 hours before removal
|
|
|
Advantages of the inguinal cryptorchid approach:
|
locating the testicle is not necessary before surgery, is rapid, and has a small incision
|
|
|
Describe parainguinal cryptorchid approach:
|
incision 1-2 cm medial and parallel to the superficial inguinal ring, though the aponeurosis of the external abdominal oblique muscle, centered over the cranial portion of the superficial inguinal ring. After penetrating the abdomen with digital pressure, a finger is sweep near the ring to grasp the epididymis, ductus deferens, or gubernaculum and exteriorizing through the incision. Once exteriorized, traction is used to help exteriorize the testicle, which is emasculated or ligated and transected. Once the testicle is removed, the aponeurosis of the external abdominal oblique muscle is sutured. the approach incision can be left open or closed primarily.
|
|
|
What is done if there is difficulty in locating the testicle with the parainguinal cryptorchid approach?
|
incision can be converted to an invasive approach to allow the hand access the abdomen
|
|
|
Benefits of the parainguinal approach:
|
smaller incision, non-invasive
|
|
|
Describe suprapubic paramedian cryptorchid approach:
|
lateral to the preputial orifice and extends caudally. Subcutaneous vessels should be ligated. The rectus abdominus is split longitudinally and the abdomen is penetrated digitally. A hand is introduced and swept near the vaginal ring to grasp the testicle and exteriorize it. After testicle removal, the abdominal tunic, SQ, and skin are closed primarily.
|
|
|
Disadvantages of suprapublic paramedian cryptorchid approach:
|
long incision lengthens convalescence time, increased risk of evisceration
|
|
|
Describe flank cryptorchid approach:
|
incision is through a modified grid approach. A hand is introduced and the testicle can be removed after exteriorization or it can be removed intra-abdominally with an ecraseur. After removal, all layers, except for the peritoneum and transverse abdominal muscle are closed
|
|
|
Describe Laparoscopic cryptorchid approach:
|
testicle can be either exteriorized and removed or it can be ligated and transected intra-abdominally and removed through a widened instrument portal
|
|
|
Options for intra-abdominal ligation and transection during laparoscopic cryptorchid approach:
|
endoscopic clips, ligating loops, endoscopic scissors, mono or bipolar electrocoagulation, or vessel sealing devices such as ligasure or enseal
|
|
|
Advantage of intra-abdominal transection with laparoscopic cryptorchid approach:
|
stump can be visualized before removal. Removal of the testicle causes loss of insufflation which decreases visability and impairs ability to address hemorrhage if it has occurred
|
|
|
Advantages of laparoscopic cryptorchectomy:
|
simplicity in locating the testis, the vaginal ring is not disrupted which decreases evisceration risk, and shortens healing time
|
|
|
Post-operative complication of castration:
|
hemorrhage, evisceration, edema, colic, lameness, septic funiculitis, clostridial infection, septic peritonitis, penile damage, hydrocele, continued masculine behavior, and incomplete cryptorchid castration
|
|
|
When does sustained hemorrhage occur?
|
inadequate crushing of the testicular artery
|
|
|
Methods to limit castration hemorrhage:
|
applying the emasculators in the correct position and perpendicular to the cord, separating the cremaster from the cord prior to crushing, and placing ligatures proximal to emasculation
|
|
|
Disadvantage of ligatures on the spermatic cord?
|
increase risk of infection due to the presence of foreign material
|
|
|
How is existing castration hemorrhage stopped?
|
packing the scrotum with gauze and temporarily closing the scrotum for 24 hours, applying curved clamps across the distal end of the stump for 24 hours, or laparoscopic intra-abdominal ligation of the testicular artery
|
|
|
Side effects of formalin by direct injection IV:
|
restlessness, lacrimation, salivation, elevation of the tail, nasal discharge, increased defecation, sweating, fasciculation, abdominal pain, and tenesmus
|
|
|
When does Evisceration usually occur?
|
within 4 hours of castration
|
|
|
What is Septic funiculitis?
|
infection of the spermatic cord and occurs from extension of scrotal infection or contaminated emasculators or ligature
|
|
|
Medical therapy for septic funiculitis?
|
systemic antimicrobials and re-establishment of drainage but is often unsuccessful
|
|
|
Surgical therapy for septic funiculitis?
|
removal of the infected stump
|
|
|
What is Champignon?
|
used to describe septic funiculitis caused by streptococcus bacteria and is characterized by purulent discharge and a muchroom-like mound of granulation tissue that protrudes from the incision
|
|
|
What is scirrhous cord?
|
used to describe septic funiculitis caused by staphylococcus bacteria and is characterized by enlargement of the cord and abscessation
|
|
|
What is botryomycosis?
|
Same as scirrhous cord
|
|
|
Cause of Continued masculine behavior?
|
most likely innate behavior and not caused by exragonadal production of androgens, unless the testicle was incompletely removed, as in the case of a cryptorchid having only the epididymis removed during castration
|
|
|
Approach to routine Ruminant castration?
|
scrotal incision and using a closed technique
|
|
|
Additional castration option in ruminants:
|
bloodless castration, usually with the application of elastic bands to the neck of the scrotum to cause ischemic vascular necrosis and sloughing of the testicles and scrotum in about 3 weeks
|
|
|
Location of Scrotal or inguinal hernias in ruminants?
|
Most are left sided, likely because the rumen weight disposes bull’s to lay with the left rear leg abducted
|
|
|
What is a pseudohernia?
|
prolapse of SQ fat into the inguinal canal
|
|
|
Most common Type of inguinal hernia in ruminants:
|
chronic, affecting testicular function, and can result in adhesions
|
|
|
Surgical options for ruminant inguinal hernias:
|
flank approach, which allows correction of herniation and closure of the vaginal ring, or an inguinal approach, with closure of the external inguinal ring after hernia correction
|

