![]()
![]()
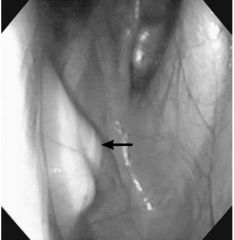
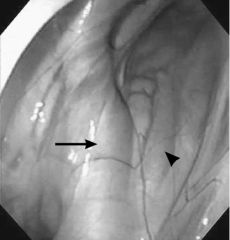
![]()
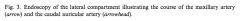
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
91 Cards in this Set
- Front
- Back
|
What is the GP?
|
extension of the Eustachian or auditory tube that connects the middle ear to the pharynx
|
|
|
What is the medial border of the GP?
|
paired pouches are separated by a median septum of mucous membrane, which is ventral to the longus capitus and the rectus capitus ventralis muscles
|
|
|
The rostral border of the GP:
|
basisphenoid bone
|
|
|
The ventral border of the GP:
|
pharynx, retropharyngeal LN, and the esophagus
|
|
|
The caudal border of the GP:
|
atlantooccipital joint
|
|
|
The lateral border of the GP:
|
digastricus muscles and the parotid and mandibular salivary glands
|
|
|
The dorsal border of the GP:
|
petrous part of the temporal bone, tympanic bulla, and auditory meatus
|
|
|
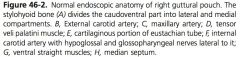
What structures are on the caudal wall of the GP?
|
internal carotid artery, the cranial cervical ganglion, the cervical sympathetic trunk, the vagus nerve, the glossopharyngeal nerve, the hypogossal nerve, and the accessory spinal nerve
|
|
|
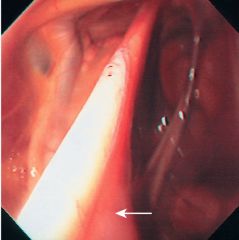
What structures are under the mucosa of the ventral floor of the medial compartment?
|
cranial laryngeal nerve and the pharyngeal branch of the vagus nerve
|
|
|
What structures are located in the lateral wall of the lateral compartment?
|
external carotid artery, its branches, the caudal auricular artery, and the superficial temporal artery
|
|
|
What structures are on the dorsal aspect of the lateral compartment?
|
maxillary artery, CN7 (facial) is located in the caudal dorsal aspect, mandibular nerve, a branch of the trigeminal nerve, travels rostrally
|
|
|
What structure can also be affected by GP diseases that affect the facial nerve?
|
vestibulocochlear nerve (VIII) does not enter the GP, but is closely related to the facial nerve
|
|
|
Cellular composition of The mucous membrane of the GP:
|
pseudostratisfied ciliated epithelium which have goblet cells
|
|
|
What muscles open the pharyngeal orifice?
|
TVP, LVP, palatopharyngeus, and pterygopharyngeus muscles open the pharyngeal orifice to the GP
|
|
|
What is involved with opening/ expanding the auditory tube?
|
increased inspiratory pressure as well as the stylopharyngeus and pterygopharyngeus muscles
|
|
|
GP diseases:
|
tympany, empyema, mycosis, rupture of the ventral straight muscles, and temporohyoid osteoarthropathy.
|
|
|
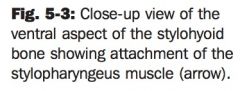
Who is affected by tympany?
|
foals up to 1 year of age, more often in fillies than colts and a breed predilication in Arabians and Paints has been identified
|
|
|
What is tympany?
|
distension of the GP with air under pressure, because Air accumulates due to the mucosal flap acting as a one way valve to trap air in the pouch, inflammation that prevents air escape, or muscle dysfunction that prevents opening of the orifice
|
|
|
Treatment options for typmany:
|
fenestration of the median septum, removal of the obstructing membrane, or creation of a salpingopharyngeal fistula
|
|
|
Approaches to median septum fenestration:
|
under GA with a viborg triangle or a modified whitehouse approach, or it can be performed transendoscopically with laser or electrosurgery
|
|
|
When is Fenestration of the median septum chosen?
|
unilateral disease because it depends on one working orifice to release air
|
|
|
Complications of septal fenestration:
|
closure of the fenestration
|
|
|
What is the plica salpingopharyngeus?
|
mucosal fold on the floor of the pharyngeal orifice, attached medially to the cartilaginous flap of the Eustachian tube and laterally to the pharyngeal wall
|
|
|
Approaches to plica resection:
|
GA by a modified whitehouse approach
|
|
|
Plica resection complication:
|
obstruction of the opening due to inflammation and edema
|
|
|
Approach to creation of a salpingopharyngeal fistula:
|
transendoscopically, and the fistula is created with a laser, caudal to the pharyngeal GP opening
|
|
|
Complications of salpingopharngeal fistula:
|
closure of the fistula and failure to bypass the defective pharyngeal ostium. Fistula closure can be minimized by keeping a foley catheter in the fistula for at least 7-10 days and minimizing inflammation
|
|
|
Treatment of chondroids:
|
maceration within the pouch, removal by suction, grasping forceps, or retrieval baskets, surgical drainage
|
|
|
Disadvantages of non-surgical removal of chondroids:
|
slow and tedious
|
|
|
Advantage of non-surgical removal of chondroids:
|
avoidance of a surgical procedure
|
|
|
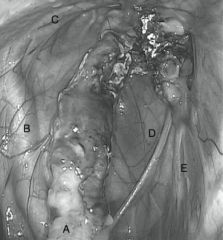
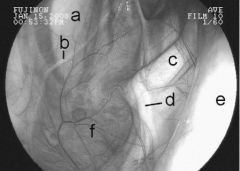
Mycosis most common organism:
|
aspergillus fumigatus,
|
|
|
What is a diphtheritic membrane?
|
composed of necrotic tissue, bacteria, and fungal mycelia
|
|
|
The most common vessel to be affected by mycosis:
|
ICA, but the ECA or the MA is also commonly affected
|
|
|
Horner’s signs:
|
ptosis, miois, enophthalmos, and patchy cervical sweating.
|
|
|
What are The ventral straight muscles of the head?
|
more dorsally located rectus capitis ventralis and the more ventral longus capitus muscles
|
|
|
How can rupture of the straight muscles be distinguished from GP mycosis?
|
With rupture of the straight muscles, the roof of the pharynx is usually collapsed, both pouches are affected, there is no diphtheritic membrane, and the vessels in the caudal aspect of the GP are not affected. This injury may include fracture of the basisphenoid or basioccipital bone, which can be seen endoscopically in the GP after inflammation and hemorrhage have subsided.
|
|
|
Radiographic appearance of rupture of ventral straight muscles:
|
GP is partially obliterated by soft tissue opacity, the pharynx is compressed by soft tissue, and avulsion fragments of the basisphenoid bone may be seen
|
|
|
What is THO?
|
result of a inner or middle ear infection that spreads to involve the temporohyoid joint, stylohyoid bone, tympanohyoid cartilage, and the squamous portion of the temporal bone
|
|
|
Surgical options for THO:
|
partial stylohyoid ostectomy or ceratohyoidectomy
|
|
|
Benefits of partial stylohyoid ostectomy:
|
decreases the forces on the temporohyoid joint, preventing skull factures
|
|
|
Disadvantages of partial stylohyoid ostectomy:
|
associated with dysphagia due to injury to the hypoglossal nerve, and regrowth of the stylohyoid bone and recurrence of clinical signs
|
|
|
Benefit of ceratohyoidectomy:
|
easier than partial stylohyoid ostecomy and more permament
|
|
|
Describe ceratohyoidectomy:
|
10-15 cm incision medial to the linguofacial vein 2 cm from midline and centered on the basihyoid bone. The basihyoid is exposed. The geniohyoid bone is separated to expose the ceratohyoid, which is disarticulated from the basihyoid with cartilage scissors. The ceratohyoid is separated from its attachments to the ceratohyoideus, hyoideus transversus, and the genioglossus before disarticulation of the ceratohyoid from the stylohyoid with cartilage scissors. The separated muscles are sutured over the defect to prevent bone regeneration.
|
|
|
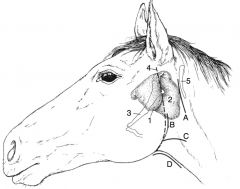
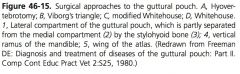
Surgical approaches to the GP:
|
hyovertebrotomy, viborg’s triangle, whitehouse, modified whitehouse and modified garm’s approaches
|
|
|
Risks of surgery of the GP:
|
iatrogenic nerve injury
|
|
|
Describe Hyovertebrotomy:
|
parallel to the wing of the atlas, with cranial reflection of the parotid gland and parotidoauricular muscle
|
|
|
Disadvantage of hyovertebrotomy:
|
does not establish ventral drainage
|
|
|
The borders of viborg’s triangle:
|
tendon of the sternocephalicus, the linguofacial vein, and the vertical ramus of the mandible
|
|
|
Complications of viborg’s triangle approach:
|
transection of the parotid duct or injury to the branches of the vagus nerve on the ventral aspect of the GP
|
|
|
The whitehouse approach:
|
incision on ventral midline over the larynx, dissecting along the larynx until the GP is reached. The pouch is opened medial to the stylohyoid bone.
|
|
|
Complications of whitehouse approach:
|
injury to the pharyngeal branch of the vagus nerve and the cranial laryngeal nerve, which are near the incision into the GP
|
|
|
The modified whitehouse approach:
|
similar to the approach to PL but more rostral. The lateral aspect of the larynx is exposed and blunt dissection exposes the GP.
|
|
|
Why is The modified whitehouse preferred over the whitehouse approach?
|
through a natural plane and there is no incision between the sternohyoideus and the omohyoideus. It can also be performed standing.
|
|
|
Benefits of Both whitehouse approaches:
|
allow access to the roof of the pouch, the lateral compartment, provide excellent ventral drainage, and with penetration of the septum, can allow access to the opposite GP
|
|
|
Modified garm’s techniques:
|
incision is made between the ramus of the mandible and the submandibular LN, blunt dissection is continued until the lateral compartment of the GP is reached
|
|
|
Benefit of modified garm’s:
|
allows access to the lateral compartment
|
|
|
Disadvantage of modified garm’s:
|
plane of dissection is deep and narrow, so there is no visual access and limited room provided, other than a lavage tube
|
|
|
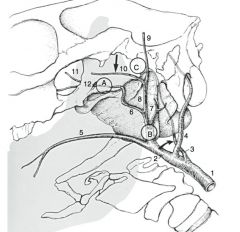
methods of occlusion of the arteries affected by GP mycosis:
|
can be ligated, occluded with balloon catheters or disposable balloon catheters, or embolized with transarterial coils or nitinol vascular plugs
|
|
|
effect of occlusion of the ipsilateral CCA If a horse is bleeding from the ICA:
|
would increase blood flow due to the cerebral arterial circle
|
|
|
effect of occlusion of the ICA if a horse is bleeding from the ICA:
|
would only decrease blood flow but not blood pressure
|
|
|
effect of occlusion of the ipsilateral CCA If bleeding from the ECA or its branches:
|
would temporarily decrease flow
|
|
|
branches of the ECA:
|
MA, caudal auricular, superficial temporal
|
|
|
what is required for successful occlusion of the ICA?
|
vessel is occluded distal to the lesion at the level of the sigmoid flexure.
|
|
|
Disadvantage of ligation techniques for ICA ligation:
|
difficult to access distal location of the ICA because it is deep within the GP
|
|
|
Where is Proximal occlusion of the ICA performed?
|
distal to its origin from the CCA
|
|
|
How is the proximal ICA accessed for ligation?
|
hyovertebrotomy
|
|
|
Source of Retrograde flow to the ECA and its branches:
|
major palatine artery, which forms an arterial loop of both the right and left sides
|
|
|
Where is proximal ECA occluded?
|
just distal to its branching from the linguofacial trunk, or alternatively, through a balloon catheter inserted into the transverse facial artery and passed to just distal to the trunk
|
|
|
What are benefits of occlusion of the proximal ECA through the transverse facial artery?
|
ECA does not need to be exposed with the hyovertebrotomy
|
|
|
Where does distal occlusion of the ECA occur with the balloon system?
|
Balloon inserted into the major palatine artery at the level of the corner incisor. The balloon is passed retrograde for a distance of approximately 40 cm. The balloon is partly inflated the retracted to set against the alar foramen, then fully inflated
|
|
|
Where does distal occlusion of the ECA/ MA occur With the embolization systems?
|
MA is occluded distal to the branching of the superficial temporal artery and proximal to the infraorbital, buccal, and mandibular alveolar arteries. Confirmation is made by passing the catheter to the level of the ophthalmic artery, injecting contrast, and withdrawing the catheter until it is at the level of the alar foramen
|
|
|
Approach for embolization systems:
|
through the CCA in the proximal jugular groove
|
|
|
Advantages of embolization systems over ligation and balloon systems:
|
accurate placement of occluding items, no need to manipulate a remote catheter or protect and indwelling catheter, easier placement of embolization items compared with balloons, rapid induction of thrombosis, visualization of the effects of embolization with fluoroscopy, less invasive surgical approach, with shorter anesthesia and shorter hospitalization
|
|
|
Disadvantages of embolization systems
|
need for fluoroscopy, positioning the horse in the fluoroscopic unit, and additional costs associated the more sophisticated surgery
|
|
|
difference between the coil system and the nitinol plug system:
|
usually only a single plug is required for embolization using the nitinol plugs but several coils may be necessary to occlude the vessel with the coil system
|
|
|
Complications of balloon systems:
|
fatal hemorrhage, blindness
|
|
|
Causes of hemorrhage after vessel occlusion:
|
aberrant vasculature or inappropriate placement of the balloons
|
|
|
Aberrant vasculature associated with the ICA:
|
occipital artery and the ICA arising from a common trunk, and an ICA that leads to the caudal cerebellar artery instead of following its usual path
|
|
|
How can risks caudal cerebellar occlusion be minimized during balloon catheterization?
|
noting that the distance the balloon passes is either much shorter than 13 cm or much longer than 13 cm
|
|
|
How does Blindness occur with vessel occlusion?
|
Improper occlusion of the major palatine artery resulting in steal phenomenon
|
|
|
What is the steal phenomenon?
|
When the ECA is occluded at both the level of the major palatine artery and proximally near the liguofacial trunk, blood flow from the internal ophthalmic, flow from the internal ophthalmic artery is diverted through the anastomosis and supplies branches of the major palatine artery proximal to its ligation (between the 2 sites of occlusion.) These vessels “steal” blood flow to the eye resulting in ischemia to the eye and blindness. If the balloon catheter in the major palatine artery is passed proximal to the anastomosis, then the anastomosis between the external ophthalmic and internal ophthalmic is occluded and blood is not “stolen” to supply branches of the major palatine artery.
|
|
|
Blood flow to the eye:
|
external ophthalmic artery, which is a branch of the ECA, and less so from the internal ophthalmic artery, a branch of the ICA. Often there is an anastomosis between the external and internal ophthalmic arteries.
|
|

|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|

|
|
|
|
|
|
|
|
|
|

