![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
125 Cards in this Set
- Front
- Back
|
Function of intrinsic nasopharyngeal muscles:
|
support the pharynx by contraction which tenses and dilates the nasopharynx
|
|
|
Function of extrinsic nasopharyngeal muscles:
|
regulate soft palate position, to increase nasopharyngeal diameter and decrease nasopharyngeal compliance (make it stiffer) by moving the tongue, or hyoid or laryngeal structures
|
|
|
What are the intrinsic nasophayngeal muscles:
|
tensor veli palatini, levator veli palatini, palatinus, palatopharyngeus, and caudal stylopharyngeus
|
|
|
Combined function of TVP, LVP, palatinus, and palatopharyngeus:
|
soft palate position
|
|
|
Composition of the soft palate from ventral to dorsal:
|
oral mucosa, palatine aponeurosis, palatinus & palatopharyngeus muscles, and the nasopharyngeal mucosa
|
|
|
What is the palatine aponeurosis?
|
expanded tendon of the TVP
|
|
|
What does the palatine aponeurosis attach to?
|
caudal aspect of the hard palate
|
|
|
Vascular supply to the soft palate:
|
linguofacial trunk and maxillary artery
|
|
|
TVP innervation:
|
mandibular branch of the trigeminal nerve
|
|
|
Origin & insertion of TVP:
|
originates at the petrous temporal bone, pterygoid bone, and lateral lamina of the auditory tube, travels ventral and rostral to the hamulus of the pterygoid bone, and inserts on the caudal hard palate as the palatine aponeurosis
|
|
|
Function of the TVP:
|
tenses the rostral soft palate and depresses it ventrally during inspiration
|
|
|
Origin and insertion of the palatinus:
|
originates just caudal to the palatine aponeurosis, extends caudally to end at the caudal free border of the soft palate, but it sends muscle bundles laterally to form the pillars of the soft palate, uniting dorsally to form the palatopharyngeal arch
|
|
|
Origin and insertion of the palatopharyngeus?
|
orgininates just lateral to the palatinus and form a portion of the nasopharyngeal wall, before terminating on the dorsal edge of the thyroid cartilage and dorsally on midline
|
|
|
Innervation of palatinus:
|
pharyngeal branch of the vagus nerve
|
|
|
Function of the palatinus:
|
shorten the soft palate, depressing it ventrally toward the tongue
|
|
|
Innervation of palatopharyngeus:
|
pharyngeal branch of the vagus nerve
|
|
|
Function of the palatopharyngeus:
|
shorten the soft palate, depressing it ventrally toward the tongue
|
|
|
Origin and insertion of LVP:
|
from the petrous temporal bone to insert within the glandular layer of the dorsal soft palate
|
|
|
Function of LVP:
|
elevates the soft palate during swallowing
|
|
|
Innervation of LVP:
|
pharyngeal branch of the vagus nerve
|
|
|
Origin and insertion of caudal stylopharyngeus:
|
originates on the medial aspect of the middle third of the stylohyoid bone and travels ventral and rostral to insert on the dorsolateral wall of the pharynx
|
|
|
Innervation of caudal stylopharyngeus:
|
glossopharyngeal nerve (CN9)
|
|
|
How do extrinisic nasopharyngeal muscles increase nasopharyngeal diameter?
|
altering the size of the oropharynx or the position of the larynx, which results in stability of the soft palate during exercise
|
|
|
What are the extrinsic nasopharyngeal muscles?
|
geniohyoideus, thyrohyoideus, genioglossus, hyoglossus, styloglossus, hyoepiglotticus, sternohyoideus and sternothyroideus
|
|
|
Origin and insertion of genioglossus:
|
originates within the median plane of the tongue and inserts on the mandible caudal to the symphysis
|
|
|
Function of genioglossus:
|
protracts the tongue, pulling the basihyoid rostral
|
|
|
Innervation of genioglossus:
|
hypoglossal nerve (CN12)
|
|
|
Origin and insertion of geniohyoideus:
|
originates on the medial aspect of the mandible and inserts on the basihyoid
|
|
|
Function of geniohyoideus:
|
tongue is protracted and the hyoid apparatus is pulled rostral
|
|
|
Innervation of geniohyoideus:
|
hypoglossal nerve (CN12)
|
|
|
Function of styloglossus:
|
retracts the tongue
|
|
|
Origin and insertion of styloglossus:
|
originating on the lateral aspect of the stylohyoid bone and inserting on the tip of the tongue
|
|
|
Innervation of styloglossus:
|
hypoglossal nerve (CN12)
|
|
|
Function of hyoglossus:
|
retracts the tongue, depressing the base of the tongue
|
|
|
Origin and insertion of hyoglossus:
|
originates on the lingual process, stylohyoid and thyrohyoid bones and inserts on the dorsal aspect of the tongue
|
|
|
Innervation of hyoglossus:
|
hypoglossal nerve (CN12)
|
|
|
Function of sternohyoideus and sternothyroideus:
|
retract the hyoid and laryngeal apparatus caudally
|
|
|
Origin and insertion of sternohyoideus:
|
originates at the sternum, inserts on the basihyoid bone and lingual process
|
|
|
Origin and insertion of sternothyroideus:
|
originates at the sternum, inserts on the thyroid cartilage
|
|
|
Innervation of sternohyoideus :
|
branches of the first and second cervical nerves
|
|
|
Origin and insertion of hyoepiglotticus:
|
originates on the hyoid bone and inserts on the epiglottis
|
|
|
Function of hyoepiglotticus:
|
pulls the epiglottis ventrally, increasing the ventral dimension of the rima glottis
|
|
|
Innervation of hyoepiglotticus:
|
hypoglossal nerve (CN12)
|
|
|
Location of thyrohyodeus:
|
between the thyroid cartilage and the thyrohyoid bone
|
|
|
Function of thyrohyoideus:
|
moves the larynx rostral so the thyroid cartilage is more dorsal and rostral than the basihyoid
|
|
|
Examples of anatomical nasopharyngeal disorders:
|
nasopharyngeal cicatrix or masses
|
|
|
Where does nasopharyngeal cicatrix predomindately occur?
|
hot climates in horses on pasture
|
|
|
Etiology of nasopharyngeal cicatrix:
|
environmental allergen is though to be the instigator of inflammation that results in a web of scarring
|
|
|
Management of nasopharyngeal cicatrix:
|
removing the horse from pasture and administering topical and systemic anti-inflammatory medications. Laser transection of some of the scar tissue or permanent tracheostomy can be considered in more severe cases
|
|
|
What is not indicated for the treatment of nasopharyngeal cicatrix?
|
Partial arytenoidectomy is not indicated because heavy scarring in the region predisposes to decreasing the diameter of the rima glottis
|
|
|
Surgical approaches to the nasopharynx:
|
nasal endoscopy, pharyngotomy, orally, or laryngotomy
|
|
|
Complications of pharyngotomy:
|
damage to the hyoepiglotticus muscle or its innervation
|
|
|
Describe pharyngotomy:
|
skin incision is centered on midline between the rostral aspect of the thyroid cartilage and the basihyoid bone. The sternohyoideus is separated on midline and the loose fascia between the thyroid cartilage and basihyoid is incised. Deep to this fascia is the hyoepiglotticus, which is separated on midline. The oropharyngeal mucosa is incised. The basihyoid can be split longitudinally with an osteotome to improve visualization
|
|
|
Closure of a pharyngotomy:
|
simple continuous closure of the oropharyngeal mucosa with poliglecaprone, steel wire in the basihyoid, continuous closure of the sternohyoideus, and just the subcutaneous and skin over the basihyoid
|
|
|
Functional disorders of the nasopharynx:
|
rostral pharyngeal collapse, dorsal or lateral nasopharyngeal collapse, and dorsal displacement of the soft palate
|
|
|
What is rostral pharyngeal collapse?
|
fluttering of the rostral aspect of the soft palate
|
|
|
What rostral pharyngeal collapse conditions exist?
|
Rostral palatal instability is billowing of the rostral aspect of the soft palate during inspiration and is associated with minimal obstruction. Palatal instability is billowing of the entire soft palate, which does cause obstruction and may be a precursor condition to DDSP
|
|
|
Medical therapy for rostral pharyngeal collapse:
|
systemic and topical anti-inflammatory medications, and use of a dropped or figure 8 noseband to prevent airflow into the oropharynx
|
|
|
Surgical management of rostral pharyngeal collapse:
|
laser thermoplasty, injection of sclerosis agents, thermal palatoplasty, and tension palatoplasty.
|
|
|
Describe thermal palatoplasty:
|
oral approach under GA. A T shaped iron is heated and used to cauterize the ventral (oral) surface of the soft palate from the hard palate to beyond the palatoglossal arch
|
|
|
Describe tension palatoplasty:
|
9-12 cm elliptical incision on the ventral (oral) surface of the soft palate extending from just caudal to the hard palate, removing a portion of the mucosa and submucosa. The edges are apposed with poliglecaprone in an interrupted pattern
|
|
|
What is maximum tension palatoplasty?
|
repeating the tension palatoplasty procedure 4 weeks after the initial procedure to further increase tension of the soft palate
|
|
|
When can training resume after tension palatoplasty?
|
hand walked for 4 weeks before training resumes
|
|
|
Causes of dorsal or lateral pharyngeal collapse:
|
Inflammation or neuritis may cause these conditions or they can be secondary to GP disease, HYPP, botulism, or EPM
|
|
|
Treatment of dorsal or lateral pharyngeal collapse:
|
directed toward the underlying condition and controlling inflammation
|
|
|
Causes of DDSP:
|
in a small amount of cases can be caused by structural abnormalities such as palatal cysts, subepiglottic masses, and epiglottic entrapment. Most cases are cause by intrinsic muscular disfunction which results in increased compliance (less stiffness) of the soft palate
|
|
|
What tends to confer stability to the soft palate during exercise?
|
Dorsally positioned larynx and basihyoid bone
|
|
|
What does dysphagia with DDSP indicate?
|
more advanced deficit of the intrinsic muscles or innervation and traditional treatments directed toward correction of respiratory impairment caused by DDSP may worsen aspiration associated with dysphagia
|
|
|
Experimental models of DDSP:
|
Model 1 is blockade of the pharyngeal branch of the vagus nerve, but results in both airway and swallowing dysfunction at rest. Model 2 is the thyrohyoideus muscle model which showed that this muscle decreased the collapsibility of the nasopharynx during exercise. Model 3 is blockade of the hypoglossal nerve which determined at the function of this muscle had a stabilizing effect on the nasopharynx
|
|
|
What phase of respiration does DDSP affect?
|
expiratory
|
|
|
What are the differences in diagnosis of DDSP by treadmill or over ground endoscopy?
|
treadmill examination diagnoses DDSP more frequently than over ground endoscopy, presumably due to lack of exercise protocol and reluctance of trainers to work the horse at maximal intensity with over ground endoscopy
|
|
|
How is DDSP diagnosed if neither over ground or treadmill exercise is possible?
|
Resting endoscopy immediately following work
|
|
|
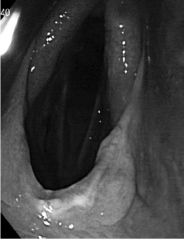
What may be associated with but not pathopneumonic for DDSP?
|
ulceration of the caudal edge of the soft palate and bruising of the dorsal nasopharyngeal wall
|
|
|
Medical management of DDSP:
|
systemic and topical anti-inflammatory medication, allowing immature or unfit horses to mature or become fit, using a figure 8 noseband, using a bit that secures the tongue or restricts caudal movement of the tongue, using a tongue tie, or using a throat support device (cornel collar.)
|
|
|
Bit options for DDSP:
|
W bit, a spoon bit or a serena song bit
|
|
|
Efficacy of tongue tie in DDSP:
|
shown to be effective in 53-61% of cases, but experimentally is not associated with a change in position of the hyoid or larynx
|
|
|
What procedures have not shown to be beneficial in DDSP?
|
Those that aim to stiffen the soft palate, tension palatoplasty, thermal palatoplasty, sclerosing agent injection, and staphlectomy alone are not recommened
|
|
|
When is staphlectomy used?
|
removal of palatal cysts or granulomas, performed with laser application through nasal endoscopy in the standing post-operative laryngeal tie forward patient
|
|
|
Describe staphlectomy:
|
dorsal recumbency, a laryngotomy is performed. The caudal free margin of the palate is grasped with allis tissue forceps and retracted caudally OR by nasal endoscopy with application of laser to caudal free margin
|
|
|
How much of the caudal free margin of the soft palate can be resected with a staphlectomy?
|
less than 1 cm wide and in depth because resection of more than .75cm may disrupt the seal between the oro- and nasopharynx
|
|
|
When can training resume after staphlectomy?
|
2-3 weeks
|
|
|
Complications of staphlectomy:
|
removal of too much tissue from the caudal margin allowing aspiration of feed material
|
|
|
Surgical options for DDSP:
|
standard myectomy, minimally invasive myectomy, and laryngeal tie forward
|
|
|
What is standard myectomy?
|
partial resection of the sternohyoideus and sternothyroideus
|
|
|
Function of standard myectomy?
|
reducing caudal retraction of the larynx
|
|
|
Describe standard myectomy:
|
standing or under GA. A 10 cm incision is made on ventral midline at the junction of the proximal and middle third of the neck. The sternohyiodeus and sternothyroideus muscles are undermined. The proximal and distal aspect of the undermined muscles are clamped with Rochester-calmart forceps then sharply transected to remove a 6-8 cm segment of both muscles
|
|
|
When can training resume after standard myectomy?
|
2 weeks when sutures are removed from the skin
|
|
|
Complications of standard myectomy?
|
incisional
|
|
|
What is minimally invasive myectomy?
|
Llewellyn procedure or a partial sternothyroideus myectomy and tenectomy
|
|
|
Describe minimally invasive myectomy?
|
performed under GA. An incision is made on ventral midline centered over the cricoid cartilage, and dissection continues to expose the ventral, caudolateral aspect of the thyroid cartilage. The tendon of insertion of the sternothyroideus is undermined and transected 1 cm caudal to its insertion on the thyroid cartilage, which avoids injury to the caudal laryngeal artery and the cricothyroid muscle. A 3 cm section of the muscle is removed.
|
|
|
When does training resume after minimally invasive myectomy?
|
In STB, training begins in 2-3 days but in TB training is not resumed for 2-3 weeks
|
|
|
Success of the partial sternothyroideus myectomy and tenectomy?
|
58-70%
|
|
|
Function of laryngeal tie forward:
|
mimic or replace the action of the thyrohyoideus muscles
|
|
|
Describe laryngeal tie back:
|
dorsal recumbency, a 10 cm skin incision is made from 1 cm caudal to the cricoid cartilage to 2 cm rostral to the caudal aspect of the basihyoid. Dissection exposes the ventral and lateral aspected of the thyroid cartilage and the basihyoid bone. 5 fiberwire suture is double passed through the lamina of the thyroid cartilage just ventral to the insertion of the sternothyroideus tendon. A wire passer is placed under the basilyhoid on 1 side of the lingual process from rostral to caudal. The suture ends are passed through the wire passer, with the dorsal suture ends on the ipsilateral side and the ventral suture ends on the contralateral side. Suture is repeated on the opposite side. The head is flexed and the suture is tied so that the thyroid cartilage is dorsal to and 0.1 to 1.5 cm rostral to the caudal border of the basihyoid bone. A sternothyroideus tenectomy is performed prior to closure of the fascia, SQ and skin
|
|
|
How is post-operative success of laryngeal tie forward assessed?
|
Endoscopically the epiglottis is more forward and dorsal and often does not contact the soft palate. Radiographically, the tip of the epiglottis and larynx are more forward and dorsal
|
|
|
When does training resume after laryngeal tie forward?
|
hand walked for 2 weeks and then training can resume
|
|
|
Nasopharyngeal disorders in foals:
|
choanal atresia, nasopharyngeal dysfunction, and cleft palate
|
|
|
What is choanal atresia?
|
congenital abnormality with failure of the bucconasal membrane to resorb. The bucconasal membrane separates the oro- and nasopharynx
|
|
|
When should surgical repair of unilateral atresia be performed?
|
delayed until the foal is a yearling because there is a larger nasal cavity. Larger nasal cavity decreases the likelihood of post-operative fibrosis, and reduced diameter or complete choanal closure
|
|
|
Approaches to choanal atresia repair:
|
standing, laser assisted endoscopic resection of the membrane, a nasal bone flap approach, or through a laryngotomy
|
|
|
When is nasal bone flap approach selected for choanal atresia?
|
cases of bilateral atresia or when the membrane is osseous
|
|
|
When is laryngotomy approach chosen for choanal atresia repair?
|
young foals
|
|
|
How is laryngotomy choanal atresia performed?
|
nasal endoscopic illumination of the membrane. Incision of the membrane is with uni- or bipolar laparoscopic forceps
|
|
|
What causes foal nasopharyngeal dysfunction?
|
immaturity of neonatal neuromuscular reflexes and defenses mechanisms that normal protect the larynx and pharynx
|
|
|
Treatment of foal nasophayngeal dysfunction:
|
generally resolved in 10 to 30 days, with supportive care during this period. A tracheostomy can be considered for severe airway obstruction and enteral feeding in cases of dysphagia and aspiration
|
|
|
Palatoschisis:
|
cleft palate, a congenital defect caused by interruption of embryonic closure of the soft (+/- hard) palate
|
|
|
Options for small cleft palate defect:
|
surgical repair
|
|
|
When should small cleft palate defects be repaired?
|
delayed until the foal is older and the nasal cavity is larger
|
|
|
Options for larger cleft palate defects:
|
repaired or euthanasia
|
|
|
Approaches to cleft palate repair:
|
transoral approach, laryngotomy, pharyngotomy, or mandibular symphysiotomy
|
|
|
When is pharyngotomy used for cleft palate repair?
|
caudal 1/3 of the soft palate
|
|
|
When is mandibular symphysiotomy used for repair of cleft palate?
|
with soft and hard palate defects
|
|
|
Complications of cleft palate repair:
|
dehiscence, osteomyelitis of the mandible, salivary fistulas, and incisional infections
|
|
|
When is cleft palate dehiscence apparent?
|
7 to 14 days
|
|
|
function of caudal stylopharyngeus:
|
tenses the roof of the nasopharynx, preventing collapse during inspiration
|
|
|
Disadvantages of injection of sclerosis agents or laser thermoplasty:
|
have not shown to biomechanically alter the soft palate
|
|
|
Innervation of sternothyroideus:
|
branches of the first and second cervical nerves
|
|

|
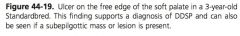
nasaopharyngeal cicatrix
|
|

|
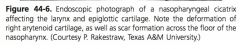
|
|

|
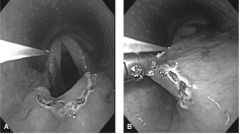
Thermal palatoplasty
|
|
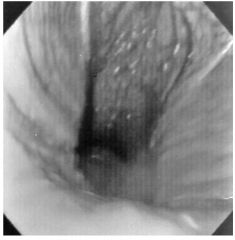
|
Lateral pharyngeal collapse
|
|
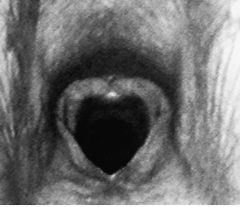
|
DDSP
|
|
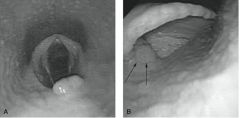
|

|
|
|
|
|
|

|

