![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
149 Cards in this Set
- Front
- Back
|
Most common material for instruments and inserts:
|
high quality stainless steel instruments with tungsten carbide inserts
|
|
|
Most common material for microsurgical instruments:
|
titanium alloy
|
|
|
Disadvantages of chrome plates carbon steel:
|
early deterioration that leads to oxidation and rust formation
|
|
|
Methods to increase corrosion resistance:
|
passivation, polishing
|
|
|
Define passivation:
|
nitric oxide removal or foreign material from stainless steel surface and coating with chromium oxide
|
|
|
Advantages of disposable blades:
|
replacement blades are consistently sharp
|
|
|
Advantages of reusable scalpel with attached blades:
|
blade does not detaches when in heavy connective tissue, joints, or deep tissue planes
|
|
|
What sterilization method is recommended for reuseable scalpels with attached blades?
|
Ethylene oxide
|
|
|
Examples of high energy scalpels:
|
electrosurgical, plasma, water, laser
|
|
|
MOA of high energy scalpels:
|
radiofrequency current produces either incision, coagulation desiccation, fulguration
|
|
|
Range of frequencies in electrosurgical units:
|
1.5-7.5 mHz
|
|
|
What does the effect produced by electrosurgical units depend on?
|
Waveform of the current produced
|
|
|
Characteristics of properly functioning scissors:
|
open & close with a smooth gliding action, tip should meet when closed
|
|
|
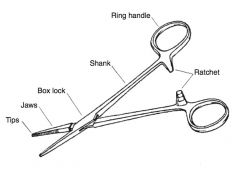
Description of grasping surface of needle holders:
|
cross hatched with central longitudinal groove
|
|
|
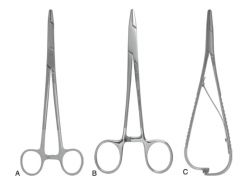
Most commonly used needle holders:
|
mayo-hegar, olsen-hegar
|
|
|
Difference between mayo-hegar and olsen-hegar needle holders:
|
olsen-hegar has scissor to cut suture
|
|
|
Advantage of tungsten carbide needle holder inserts:
|
facilitate needle grip, improve needle holder durability
|
|
|
Classes of thumb forceps:
|
traumatic (smooth or anatomic) and surgical (serrated or toothed)
|
|
|
Effect of traumatic thumb forceps:
|
smooth tips crush tissue because of forces needed to gain purchase on tissues
|
|
|
Effect of surgical thumb forceps:
|
serrations or teeth allow secure hold on tissue with minimal digital crushing pressure
|
|
|
Most aggressive surgical thumb forcep:
|
rat tooth (or tissue)
|
|
|
Least traumatic thumb forceps:
|
Russian
|
|
|
Classification of DeBakey and Cooley thumb forceps:
|
atraumatic (surgical)
|
|
|
Use of Debakey thumb forceps:
|
vascular, thoracic, intestinal surgery
|
|
|
Examples of hemostatic forceps:
|
halstead mosquito, Kelly, crile, Rochester-pean, Rochester-carmalt, Rochester-oschner
|
|
|
Difference between Kelly & crile hemostatic forceps:
|
transverse grooves are only on distal half on kelly but the entire surface on crile
|
|
|
Jaw surface Rochester-pean:
|
deep transverse grooves entire jaw surface
|
|
|
Jaw surface Rochester-carmalt:
|
longitudinal grooves on jaw with a few horizontal cross striation on tip
|
|
|
Jaw surface Rochester-oschner:
|
transverse groove with 1-to-2 interdigitating teeth at jaw tip
|
|
|
Caution with Rochester-oschner:
|
traumatic, use on tissue to be removed
|
|
|
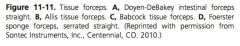
Jaw surface doyen-debakey intestinal forceps:
|
longitudinal serrations
|
|
|
Use of allis tissue forceps:
|
heavy tissue planes, tissue to be excised
|
|
|
Pull of allis tissue forceps:
|
perpendicular to the orientation of teeth
|
|
|
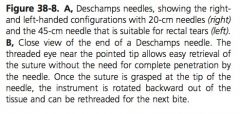
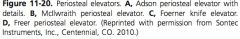
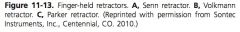
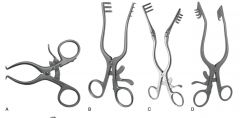
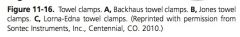
Classes of tissue retractors:
|
finger held, hand held, self retaining
|
|
|
Examples of finger held retractors:
|
senn, Volkmann, parker
|
|
|
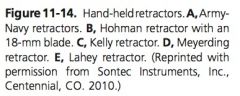
Examples of hand held retractors:
|
army-navy, hohman, Kelly, meyerding, lahey
|
|
|
Use of hohman retractor:
|
blunt projection useful in exposing bone while retracting muscle in orthopedic and reconstructive surgery
|
|
|
Examples of self retaining retractors:
|
gelpi, weitlaner, balfour, finochietto, adson cellebellar, aanes
|
|
|
Difference between weitlaner & adson cellebellar retractor:
|
weitlaner has 2 to 3 or 3 to 4 outwardly pointed blunt or sharp teeth, adson cellebellar has 4 to 4 sharp teeth
|
|
|
Difference between aanes & finochietto rectractor:
|
aanes has interchangeable blades of different depths and finochietto does not
|
|
|
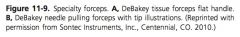
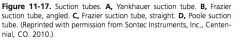
Examples of suction tubes:
|
yankauer, frazier-ferguson, poole
|
|
|
Difference between burns and volkman curettes:
|
burns have a grooved handle, volkman is a double-ended curette with an oval cup on 1 end and either a oval or rounded cup on the other end
|
|
|
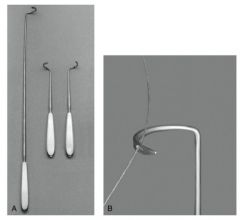
Examples of periosteal elevators:
|
Adson, Mcilwraith, Foerner, Freer
|
|
|
Sharpest periosteal elevator:
|
Foerner
|
|
|
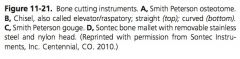
Difference between osteotome & chisel:
|
osteotomes are double beveled at cutting tip, chisels are single beveled
|
|
|
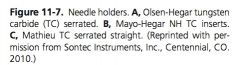
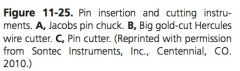
Examples of bone cutting forceps:
|
Liston, Ruskin-Liston, Stille-liston
|
|
|
Maximum sized pin for Jacob chuck:
|
0.6mm (1/4”)
|
|
|
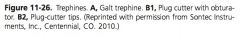
Examples of trephines:
|
galt, Michele
|
|
|
Sizes of galt trephines:
|
from 1.25-2.5 cm (1/2-1”)
|
|
|
Sizes of Michele trephines:
|
0.6-3.1 cm (1/4-1 ¼”)
|
|
|
Cutting surface of galt trephine:
|
end of shaft and outside perimeter of shaft
|
|
|
Cutting surface of Michele trephine:
|
end of shaft
|
|
|
Halsted’s principles:
|
strict aseptics during prep & surgery; good hemostasis to improve procedure & decrease infection; avoid dead space formation; minimize tissue trauma with careful handling; maintain blood supply; avoid tension on tissue; adapt corresponding tissue layers
|
|
|
3 ways to hold scalpel blade handle:
|
pencil, fingertip, palm
|
|
|
indications for pencil grip:
|
short, precise incisions
|
|
|
disadvantages of pencil grip:
|
steep angle so decreased contact of cutting edge with skin
|
|
|
Indications of fingertip grip:
|
long, straight, curved or sigmoidal incisions
|
|
|
Location of scissor cutting:
|
tip of instrument
|
|
|
Advantages of straight scissors:
|
most efficient cutting
|
|
|
Advantages of curved scissors:
|
more comfortable for surgeon, better visualization of tip in deeper planes
|
|
|
3 methods of holding needle holders:
|
tripod, palm, thenar
|
|
|
advantage of palm grip:
|
rapid instrument manipulation when precision not essential
|
|
|
Advantage of tripod grip:
|
precision when releasing needle, especially in delicate tissues
|
|
|
Advantages of electrosurgical incision:
|
reduction in blood loss; decreased need of ligatures; reduced operating time
|
|
|
Undesirable effects of charred electrosurgical instruments:
|
higher power needed to incise tissue; current dispersed to a larger area; increased thermal necrosis at edges
|
|
|
Disadvantages of electrosurgical incisions:
|
delayed wound healing, decreased resistance of wound to infection
|
|
|
Examples of mechanical hemostasis:
|
pressure (manual, hemostatic forceps), ligatures, hemostatic or vascular staples, surgical repair, esmarch system
|
|
|
Vessel diameters occluded with vascular staples:
|
up to 7mm
|
|
|
Disadvantage of vascular staples:
|
expensive, failure on larger vessels
|
|
|
Major holding (suture) layer of vessels:
|
tunica adventitia, tunica media
|
|
|
Pressure for pneumatic tourniquet after placement of esmark tourniquet for distal limb mechanical hemostasis:
|
600 mmHg
|
|
|
Length of time for tourniquet placement for distal limb mechanical hemostasis:
|
2 hours
|
|
|
2 types of thermal coagulative hemostasis:
|
obilterative, coaptive
|
|
|
define obliterative coagulation:
|
direct contact between electrode & vessel causes vessel to shrink & lumen to occlude by thrombosis
|
|
|
Define coaptive coagulation:
|
vessel initially occluded with hemostatic forceps, electrode is applied to hemostats conducting energy to the vessel inducing occlusion
|
|
|
Examples of chemical hemostasis:
|
epinephrine, 10% buffered formalin
|
|
|
Dilutions of epinephrine for chemical hemostasis:
|
1:100,000 or 1:20,000
|
|
|
Dose of buffered formalin for chemical hemostasis:
|
0.02 to 0.06 mL/kg in 0.9% saline IV
|
|
|
Suction pump vacuum pressure:
|
80-120 mmHg
|
|
|
Difference between electrocautery and electrosurgery:
|
ES pass current through tissue to cut, coagulate, desiccate, or fulgurate tissue. no electrical current passes through the tissues or patient with electrocautery
|
|
|
Types of electrosurgical circuits:
|
monopolar, bipolar
|
|
|
Components of a monopolar circuit:
|
generator, instrument (electrode), grounding pad
|
|
|
Describe monopolar circuit:
|
generator, when activated, directs current to the active electrode, through the patient’s body to the grounding pad and finally back to the generator to complete the circuit
|
|
|
Position of electrode for monopolar cutting:
|
holding the electrode slightly away from the tissues in cutting mode
|
|
|
Position of electrode for fulguration coagulation:
|
holding the electrode slightly away from the tissues in coagulation mode
|
|
|
Position of electrode for desiccation coagulation:
|
holding the electrode on the tissues in coagulation mode
|
|
|
Vessel size for monopolar hemostasis:
|
less than or 2 mm
|
|
|
Area of collateral damage from monopolar hemostasis:
|
up to 2 cm from site
|
|
|
How does bipolar differ from monopolar circuit?
|
Circuit does not pass through the patient
|
|
|
Describe bipolar circuit:
|
current passes from the generator, to 1 prong of the instrument, through the tissue in the jaws, to the opposite prong, and then back to the generator
|
|
|
Vessel size for bipolar hemostasis:
|
less than or 3 mm
|
|
|
Area of collateral damage from bipolar hemostasis:
|
up to 8mm from site
|
|
|
Describe ligasure:
|
bipolar RF vessel sealing system consisting of a generator and variety of instruments that can be used to grasp, seal, coagulate, and cut soft tissue
|
|
|
Vessel size for ligasure hemostasis:
|
less than or 7mm
|
|
|
Area of collateral damage from ligasure hemostasis:
|
1.5-6mm from site
|
|
|
Describe harmonic system:
|
generator, a hand piece, and an instrument. energy transmitted from generator to hand piece, activates crystals in the transducer, which produce high-frequency ultrasonic mechanical energy delivered to the tip. No electrical current travels through treated tissue or the patient.
|
|
|
Preferred type of endoscopic light source:
|
xenon
|
|
|
Advantage of xenon light vs halogen:
|
xenon light is whiter which results in better color reproduction
|
|
|
Common size of arthroscopy telescope diameter:
|
5mm or less
|
|
|
Common size of laparoscopy or thoracoscopy telescope diameter:
|
10mm
|
|
|
Lengths of laparoscopes:
|
30cm (from human) 57cm (equine)
|
|
|
Lengths of arthroscopes:
|
15 to 25 most common by 4mm diameter 35 cm length available
|
|
|
Common endoscopic lens angles:
|
0, 25, 30 for all and rarely used 70 for arthrocopy
|
|
|
How is fluid extravasation minimized during arthroscopy?
|
Skin incision slightly smaller than joint capsule incision, decrease fluid pressure
|
|
|
When is gas insufflation required in arthroscopy?
|
Insertion of cartilage grafts, injection of gel into subchondral bone cysts
|
|
|
Minimum and desired insufflator flow rates for abdominal insufflation:
|
10-20 L/min
|
|
|
Flow rates of needles used for abdominal insufflation:
|
veress <3L/min; teat cannula 6-7L/min
|
|
|
Desired patient abdominal pressure with insufflation:
|
15 mmHg or less
|
|
|
Desired patient thoracic pressure +/- insufflation:
|
5 mmHg
|
|
|
Difference between semm laparoscopic forceps and babcock laparoscopic forceps:
|
semm are traumatic and only used on tissue to be removed, babcock are autraumatic
|
|
|
Examples of laparoscopic vessel sealing devices:
|
Ligasure, SurgRx enseal
|
|
|
Define triangulation:
|
placement of telescope and instruments through separate portals so that they converge on the operative target
|
|
|
Effects of trendelenburg postion on cardiopulmonary parameters:
|
decreased pH, increased PaCO2, increased MAP, decreased PaO2
|
|
|
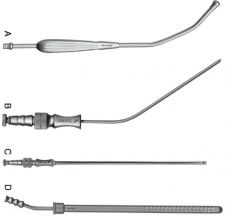
Define arterial embolization:
|
catheter directed delivery of particulate material for the purpose of embolizing selected arteries
|
|
|
Define aortic-iliac thrombosis:
|
chronic arterial occlusive disease of caudal aorta and caudal arteries
|
|
|
Instruments for AI thrombectomy:
|
fogarty graft thrombectomy catheter
|
|
|
Complications of AI thrombectomy:
|
post-anesthetic myopathy, AI thrombosis in the contralateral limb
|
|
|
Components of computer assisted surgery system:
|
instruments with LED, vetgate navigation system, orbic 3d c arm fluoroscopy
|
|

|
|
|

|
|
|

|
|
|

|
satinsky
|
|

|
|
|
|
|
|

|
|
|

|
|
|

|
|
|

|

|
|
|
|
|

|
|
|
|
|
|

|
|
|
|
|
|

|
A bard parker #3
B bard parker long #3 C narrow #7 D bard parker #4 E 10, 11, 12, 15 D 22 |
|

|
|
|

|
|
|

|
|
|
|

|
|

|

|
|
|
|
|
|
|
|

|
|
|

|
|
|

|
|
|

|
veress needle
|
|

|
|
|

|
|
|

|
A Semm
B Babcock |
|
|
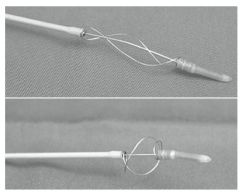
Fogarty thrombectomy catheter
|

